Chapter 8 Administration of anaesthesia Veterinary anaesthesia may be used for two main reasons: • To obliterate the pain felt during a surgical procedure or other potentially painful procedure. • To restrain the patient during a procedure required for diagnosis or treatment. As such it is one of the most common daily procedures carried out in a small animal practice. The types of anaesthesia may be divided into: • Sedation – use of drugs to calm the animal. It is widely used to reduce the anaesthetic dose, and improve the induction and recovery stages of a general anaesthetic. It is usually given by injection – for a description of the techniques see Chapter 1. • Local – infiltration with local anaesthetic (e.g. lidocaine) to desensitize a restricted area. This is not widely used in small animals, but may be used to stitch up small superficial wounds while the animal remains conscious. They may be used in cases where cardiovascular or metabolic problems make general anaesthesia dangerous. The anaesthetic may be administered by injection (see Ch.1) or in some cases by using creams or ointments designed to be absorbed through the skin. • Regional – involves desensitization of a specified area by blocking the sensory nerves supplying that area. Requires accurate knowledge of the nerve’s pathway and is widely used in large animal diagnosis and treatment (e.g. equine lameness, suturing wounds, caesarean section in cattle), but not used in small animals. • General anaesthesia – the patient is rendered unconscious and, depending on the choice of drugs, will be insensitive to pain. A general anaesthetic can be considered to take place in two stages: • Induction – the administration of a drug to render the animal unconscious. In small animal practice these are usually injectable agents given intravenously or intramuscularly, although some exotic species may be induced using volatile agents in an induction chamber. • Maintenance – the process by which the patient is kept in a state of unconsciousness until such time as it is allowed to recover. This may be achieved by using injectable drugs or gases or volatile agents given via an anaesthetic machine and the appropriate circuit. The use of injectable agents requires very little specific equipment and the administration techniques are no different from those of any other injection (see Ch. 1). The use of inhalational agents (i.e. gases or volatile liquids) requires the use of complicated and expensive anaesthetic machines and monitoring equipment and it is vital for the veterinary surgeon, who bears ultimate responsibility for the survival and recovery of the patient, to understand how the system works and is maintained. Patients admitted for anaesthesia may fall into one of four groups: • Normal healthy animals for elective routine procedures (e.g. neutering). • Apparently normal animals to undergo diagnostic procedures. • Sick animals for treatment – may present an increased anaesthetic risk. • Emergency cases – pre-anaesthetic care and assessment may be minimal as they will be admitted quickly, but support and monitoring are vital. 1. Action: The patient should be starved for 12 hours prior to surgery and owners should be advised of this when they book their appointment. 2. Action: If possible all patients booked in for elective procedures should be encouraged to urinate and defaecate before being brought to the surgery. Owners should be asked to do this. 3. Action: Weigh the patient – should be done for all patients. Rationale: This is essential for the accurate administration of premedicant and induction drugs. 4. Action: Take the client and patient into a consulting room and explain to the client exactly what will happen to their animal during the surgical procedure. You should also give an estimate of cost and this should be written down on the case records. 5. Action: Ask the client to sign a consent form. 6. Action: At some time you should have taken a full history and carried out a detailed clinical examination (see Ch. 2). 7. Action: Collect a blood sample for a pre-anaesthetic blood test. Rationale: This should be a routine procedure in any practice, but many practices will not do the test in young animals having routine operations such as neutering. The test is used to assess whether there are any underlying problems that may increase the anaesthetic risk. Parameters making up the pre-anaesthetic blood test are shown in Table 8.1. 8. Action: Administer your chosen premedicant drugs. The aim of the drugs is to calm the animal, enabling easy handling, and to allow for a smooth induction using a small dose of induction agent. 9. Action: The patient should then be placed in a warm, stress free kennel to await the procedure. Rationale: A calm, happy patient is less of an anaesthetic risk than a nervous, worried one. There are many designs of anaesthetic machine from simple small ones to large cumbersome pieces of equipment that are very often older or bought from hospitals. Whatever their shape and size, they are all designed to deliver accurate volumes of carrier gas and vaporized volatile liquids to the patient to produce anaesthesia. Figure 8.1 shows a generic form of a machine. Nowadays many practices have done away with oxygen cylinders attached to the machine and use piped oxygen from large cylinders kept outside the building. These are more convenient and more economical, although there may still be a small cylinder attached to the machine in case of emergency. There are also machines that extract oxygen from room air. Table 8.2 describes the parts and functions of the anaesthetic machine. Table 8.2 Parts of the anaesthetic machine 1. Action: Turn on the spare oxygen cylinder and check that it is full. The pressure gauge should read 137 bar. 2. Action: Turn the cylinder off and label it as ‘full’. 3. Action: Turn on the in-use cylinder; check the contents by reading the pressure gauge and label it as ‘in use’. 4. Action: Repeat the process for the nitrous oxide cylinder. The spare full cylinder should read 44 bar. 5. Action: Check for leaking gas as you turn the cylinders on. Rationale: A faulty Bodock seal can lead to gas leakage. 6. Action: Open and close the flowmeter valves. Rationale: To ensure that the ball or bobbin can move and rotate freely in its cylinder. 7. Action: Check the low oxygen alarm by turning the oxygen cylinder off and pressing the oxygen flush valve. Turn the oxygen back on. 8. Action: Check that the correct type of vaporizer is fitted to the back bar and that it is full. If more than one vaporizer is fitted, check that only one of them is switched on. Rationale: Each type of vaporizer is calibrated to take a different volatile agent and it is important to select the correct one. In reality most practices stick to one type. The control valve on the vaporizer should move freely. The level of liquid inside can be checked through the viewing port (Fig. 8.2). 9. Action: Select the correct anaesthetic circuit and check it for faults. 10. Action: Connect the scavenging system and if appropriate switch it on. Anaesthetic machines must not be used without some form of scavenging to protect personnel in the area. 1. Action: Check the contents of the gas cylinders and remove any empty ones. Replace them with full cylinders. Rationale: To ensure that the machine is ready for the next use. 2. Action: Open the oxygen flowmeter and allow a flow of 2 litres/min. Close the nitrous oxide cylinder and turn on the nitrous oxide flowmeter until the reading has fallen to 0. Close the flowmeter control. 3. Action: Turn the oxygen cylinder off and press the oxygen flush valve until no pressure reads on the pressure gauge. Rationale: All oxygen must be flushed from the pipes, as in step 2. 4. Action: Wipe the anaesthetic machine with disinfectant. The anaesthetic circuit connects the patient to the anaesthetic machine. All circuits have different uses and advantages and disadvantages. It is recommended that a practice has a range of circuits to satisfy the different clinical situations. Box 8.1 provides definitions of some of the terms used. There are two categories of circuit: • Rebreathing – these allow for a proportion of the exhaled gases to be reinhaled. Inhaled gases consist of only the carrier gas (i.e. oxygen or nitrous oxide) and the volatile liquid anaesthetic, whereas the exhaled gas contains carrier gas, volatile gas, carbon dioxide, water vapour and heat. If these can be reinhaled, less carrier and volatile gas are required to achieve unconsciousness and heat and water vapour are retained. A build-up of carbon dioxide could be fatal so this must be removed from the exhaled gases using soda lime. • Non-rebreathing – these rely on the flushing out of exhaled gases, including carbon dioxide, by the fresh gas inflow. They are therefore less economical and there is a loss of heat and moisture. As the exhaled gases pass out into the atmosphere, efficient scavenging is very important. These circuits are simple, relatively cheap and easily sterilized. They allow accurate control of inspired gases and soda lime is not required.
Preparation for anaesthesia
Procedure: Patient preparation for anaesthesia
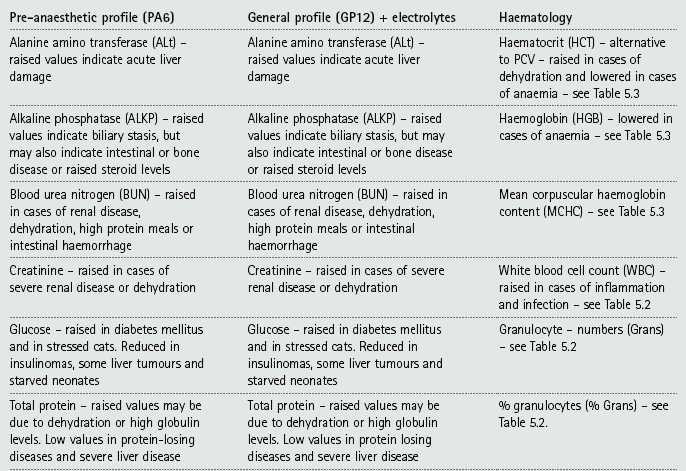
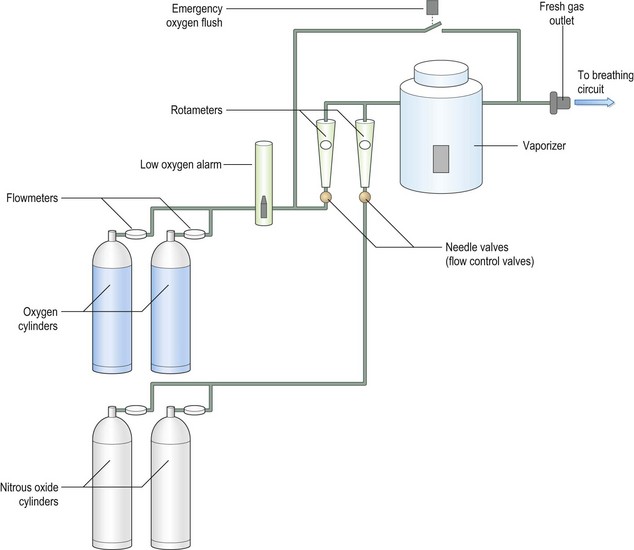
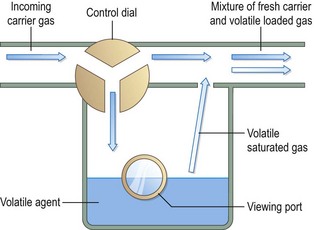
The anaesthetic machine
Component
Description
Function
Gas supply
Oxygen cylinders are black with a white collar. Nitrous oxide cylinders are blue. Smaller cylinders, such as E and F, can be incorporated into the anaesthetic machine. Larger cylinders, J and G, may be kept separate and gas supply to the anaesthetic machine is through pipes in the wall
Supplies fresh oxygen and nitrous oxide to the patient. An E-sized cylinder contains enough oxygen to supply a 20 kg dog for 3 hours
Pressure-reducing valve or regulator
Usually incorporated into the yoke and is therefore impossible to identify
Reduces the pressure of the gas leaving the cylinder to ensure a constant flow to the anaesthetic machine regardless of the pressure changes within the cylinder. It provides a safe operating pressure for the machine
Pressure gauge
Usually attached to the anaesthetic machine. As the pressure in the cylinder falls so does the pressure reading, indicating the amount of gas remaining in the tank. When using nitrous oxide, no pressure change will be seen until the cylinder is almost empty because the pressure does not fall until all the liquid has evaporated. This is not a reliable method for measuring the cylinder content of nitrous oxide – the cylinder should be weighed instead
Indicates the pressure of gas being delivered. It will read zero when the tank is empty or when the tank is switched off and the gas in the pipe evacuated
Flowmeters or rotameters
Consist of a tapered, glass tube with the flow rate written on it and either a glass ball or bobbin in the tube. Provided that the ball or bobbin can rotate freely within the tube, it will give an accurate reading of the gas flow rate. A bobbin must be read from the top, a ball from the middle. Flowmeters are gas specific and control knobs are usually colour coded: they should never be overtightened as the valve seat is easily damaged
Control and measure the flow of gas in litres per minute
Vaporizers: uncalibrated
The Boyle’s bottle (sometimes seen on very old machines) is an example of an uncalibrated vaporizer: whilst output can be varied, it fluctuates with temperature and gas flow changes
Deliver concentrations of volatile anaesthetic, in a vapour form, to the patient
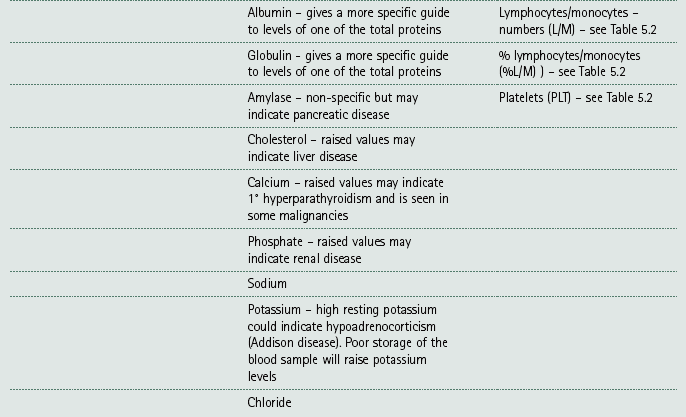
Vaporizers: calibrated
The Tec, Penlon and Plenum vaporizers (Fig. 8.1) are calibrated. They remain accurate despite temperature and gas flow changes. They are agent specific. High and low flow rates may cause problems with accuracy
Deliver a known concentration of anaesthetic vapour to the patient
Back bar
Flowmeters and vaporizers can be attached to the back bar in series. This allows more than one volatile agent to be available. The ‘Selectatec’ manifold allows swift attachment or removal of Tec 3 and 4 vaporizers
Supports the flowmeters and vaporizers
Common gas outlet
Location varies between anaesthetic machines
Connects anaesthetic circuits, ventilators or oxygen supply devices to the machine
Oxygen flush valve
Oxygen reaches this valve swiftly, bypassing the vaporizer. High flow rates are produced. The valve may be locked open in some cases, by rotating it 90°
Provides oxygen in emergency situations and purges anaesthetic from the circuit before disconnection to minimize pollution
Low oxygen alarm
An alarm sounds or, in some cases, a light flashes when oxygen levels become dangerously low
Warns the anaesthetist of low oxygen levels
Procedure: Checking the anaesthetic machine before use
Procedure: Shutting down the anaesthetic machine
Anaesthetic circuits
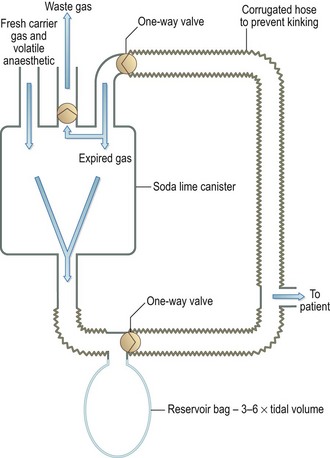
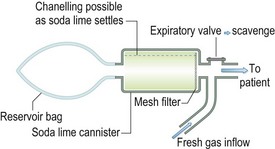
Rebreathing circuits
1 Circle system (Fig. 8.3)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Administration of anaesthesia