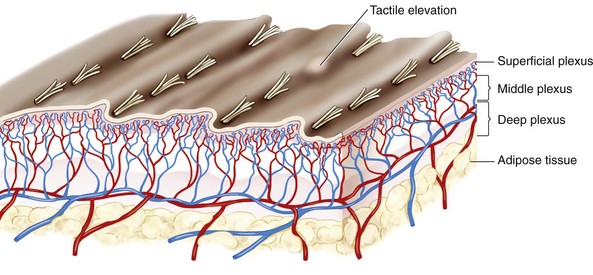
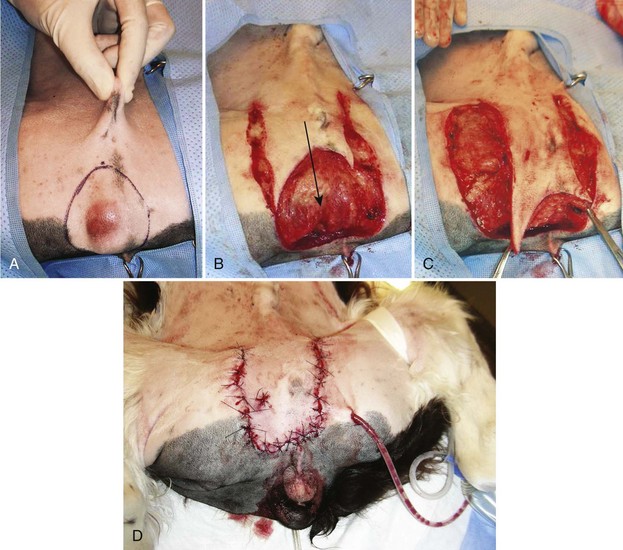
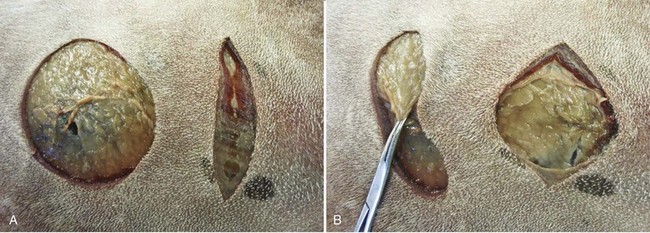
Chapter 78 Subdermal plexus flaps constitute a large and readily available group of skin flaps used to close acute and chronic wounds in small animals. They are full-thickness “tongues” of skin that are generally detached from the surrounding skin along three of four quadrants and then stretched or rotated to fill a nearby defect. Their survival relies on collateral circulation from the remaining cutaneous attachment and its vasculature, the subdermal plexus.9 Successful use is dependent on sound decision making, which should be based on an understanding of cutaneous physiology and factors affecting wound healing and on evaluation of local skin elasticity, mobility, and lines of tension. Lines of tension (see Figure 77-5) in dogs and cats have been identified;9 however, the surgeon should spend some time manipulating the local skin in each patient to determine the most appropriate way to harvest and move a skin flap without an excessive amount of stretching. The skin comprises approximately 12% of the total body weight in a 6-month-old dog. Hairy skin ranges in thickness from 0.5 to 5 mm, depending on location. The thickest skin occurs on the nose.1 Although the skin itself consists simply of the epidermis and dermis (corium), skin flaps also usually include subcutaneous tissue and portions of the thin subcutaneous muscles. The skin has a segmental arterial supply from simple and mixed cutaneous arteries that run between or through muscles, respectively, to arborize in three distinct plexuses that run parallel to the skin surface (Figure 78-1). These plexuses include the subcutaneous (deep) plexus, the cutaneous (middle) plexus, and the subpapillary (superficial) plexus. There are extensive connections between these vascular elements, providing excellent collateral flow to adjacent areas of skin.1,16 Traditional subdermal plexus flaps, which include skin and subcutaneous tissue, receive their blood supply from collateral connections to the subcutaneous plexus. Composite flaps may either be based on the subdermal plexus or on a direct cutaneous artery. The skin is richly supplied with collagen and elastin fibers that impart strength and compliance. Collagen accounts for 90% of the fiber content.1 The skin’s properties of mobility, elasticity, and rich blood supply facilitate its use in formation of flaps to cover adjacent defects. Releasing incisions, undermining, and pre- and intraoperative skin stretching all contribute to successful mobilization. Assuming there is no underlying disease, such as neoplasia or infection, the most critical issues associated with prompt healing of a defect closed with a skin flap are preservation of blood supply, closure with minimal tension, and appropriate systemic nutritional status. Extensive research in experimental animals shows that perfusion decreases to 10% and 40% of normal after initial elevation of single pedicle and bipedicle flaps, respectively.5 In delayed flaps, circulation then rises to 120% to 150% of normal after approximately 3 weeks. Re-elevation of a flap after a 3-week delay results in a much smaller decrease in blood flow (to 90 % of normal), resulting in improved survival rate. Staged development of flaps therefore helps offset the negative impacts of flap rotation and stretching. Major factors contributing to the delay phenomenon are alteration in sympathetic tone, dilation of choke vessels, reorientation of vessels, early and late changes in tissue metabolism, and neovascularization.5,19 Immediately after surgery, the elevated flap is in a hyperadrenergic state, leading to vasoconstriction. After a delay, blood supply is preserved with subsequent flap elevation because of vasodilation secondary to norepinephrine depletion. Additionally, the number and size of blood vessels to the flap increase, and their orientation is changed to favor vessels parallel to the long axis of the flap. In particular, the “choke vessels” that link adjacent vascular territories increase in size and number. Recent work on neovascularization of ischemic myocardium and limbs has cast light on other mechanisms that might also be important in the delay phenomenon. Revascularization occurs as a result of angiogenesis (growth of microvessels from the existing capillary bed) and vasculogenesis (development of new vessels in situ from bone marrow–derived endothelial progenitor cells). Investigation in a delay or vascular ischemia mouse model showed an increase in bone marrow–derived progenitor cell numbers and evidence of functional vessels produced by vasculogenesis by day 21.5 This finding supports clinical recommendations that at least 2 weeks is required for optimal vascular delay. The need for, and advantage gained by, delay is dependent on initial vascularity of the flap. Flaps with adequate circulation do not benefit from delay, but ischemic flaps potentially do. Pavletic15 describes a practical approach to delay of tubed flaps in dogs based on the available literature and taking into account that extrapolation between species may not be valid. He recommends a total 3-week delay. At 18 days, half of the pedicle is divided, and the remainder of the pedicle is severed 3 days later. Because it is dependent for survival on the subdermal plexus at its base, the flap must not be too narrow. Converging incisions that result in a flap with a wider tip than base should also be avoided. If anything, creation of a flap with a wide base that converges toward its far extremity is safer. Although restriction of pedicle width may negatively impact flap survival, an increase in flap width beyond an optimum diameter does not increase survival rates; rather, it simply increases the chance that a direct cutaneous artery might be incorporated in the base.12 Flaps should therefore be designed with a base slightly wider than the overall width of the flap and a length sufficient to cover the defect while still enabling closure of the donor site and maintenance of flap blood supply.16 Specific recommendations for flap length to width are not possible because blood supply varies among individuals and regions of the body. Closure of flaps is usually performed in two or three layers with absorbable buried sutures in the subcutaneous tissues and nonabsorbable sutures or staples in the skin. In one study, the cosmetic impact of subdermal plexus flaps secured with cyanoacrylate was evaluated. The authors concluded that the resultant scars were thinner and more esthetic than those of sutured flaps.21 Cyanoacrylate closure may therefore be worthy of consideration, especially for wounds of the head and those in show animals. A single pedicle flap is usually formed by two skin incisions that are equal in length to that of the defect. These incisions are started at each end of the wound bed, the margin of which comprises the third side of the flap. Incisions diverge toward the flap base to prevent restriction of blood supply (Figure 78-2). The skin of the flap and area surrounding the recipient bed are undermined to release subcutaneous attachments and enable better skin stretching. Wounds can be closed with two single pedicle flaps (an H-plasty) to reduce flap length and maintain blood supply. Bipedicle advancement flaps are created with an incision made parallel to the long axis of the wound. The width of the flap should approximate the width of the defect to be closed (Figure 78-3), and the total length of the flap should be no more than twice the width of the flap base. The flap is undermined and slid into the defect, where it is sutured in place. When tension is minimal at the donor site, the surrounding skin is undermined, and the site is closed primarily. If tension is too great, donor sites are allowed to heal by second intention. Advancement flaps can be used on many areas of the body, particularly the trunk, face, and forehead.14 The main disadvantage of an advancement flap is that elastic retraction and innate tension will be transmitted to the wound edge. If minimal skin tension is desired or if advancement results in dysfunction (e.g., loss of the ability to close or open the eyelids), a rotation or transposition flap is a better choice. Rotation flaps are usually developed in a stepwise fashion in dogs and cats. A curved incision (Figure 78-4) is begun at a point adjacent to the shortest side of the triangular wound (away from the pivot point). The incision is gradually lengthened and the flap undermined until it is of sufficient length to cover the wound without tension. For rectangular wounds, bilateral rotation flaps can be developed. Excessive tension may develop along the end of the incision opposite the wound. Tension can usually be relieved with a small stab wound to backcut the flap at that site.
Local or Subdermal Plexus Flaps
Anatomy and Physiology
Cutaneous Circulation
Skin Elasticity
Delay Phenomenon
Guidelines for Flap Development
Types of Subdermal Plexus Flaps
Advancement Flap
Rotation Flap
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Local or Subdermal Plexus Flaps
Only gold members can continue reading. Log In or Register to continue