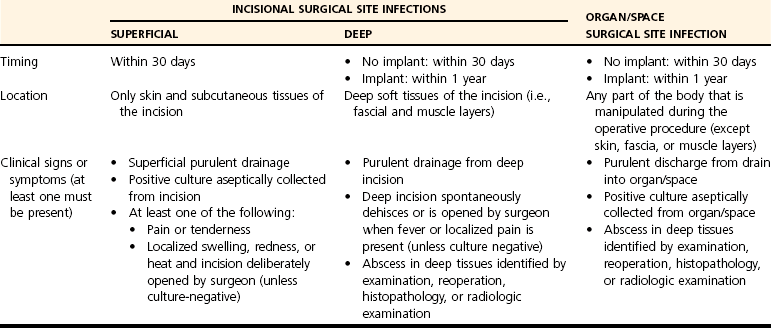
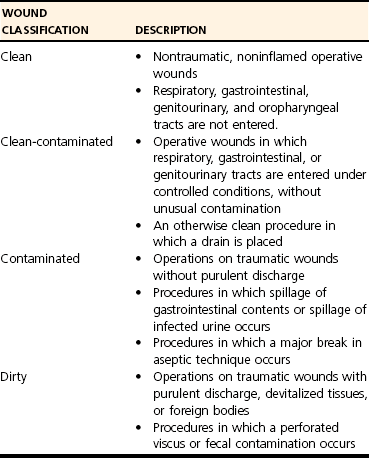
Chapter 10 Surgical site infection remains a serious problem despite the use of modern principles of preoperative preparation of animals and surgeons, antibiotic prophylaxis, and refinements in operative techniques. In addition to discomfort and morbidity in affected animals, there is client dissatisfaction because of increased costs attributable to prolonged hospitalization and treatment. Infection is caused by microorganisms introduced into the surgical wound at the time of the surgical procedure. Most of these microorganisms come from the patient’s endogenous flora, but occasionally the pathogenic organisms are acquired from an exogenous source such as the air in the operating room, surgical equipment including implants and gloves, or medications administered during the procedure.31 When an unexplained outbreak of surgical site infections occurs, investigation should be conducted to identify a potential exogenous source. A surgical site infection is one that occurs anywhere in the operative field following a surgical intervention. The U.S. Centers for Disease Control and Prevention (CDC) has developed standard criteria for defining surgical site infections.28 These criteria classify infections into incisional versus organ/space infections (Table 10-1). Incisional infections are subdivided into superficial (Figure 10-1) versus deep, depending on whether the infection is limited to the skin and subcutaneous tissue only (superficial) or extends into the deeper tissues such as the fascial and muscular layers of the body wall. Organ/space infections occur in any part of the body other than the skin, fascia, or muscle that is manipulated during the operative procedure. Examples include osteomyelitis or joint infection following an orthopedic procedure or peritonitis following an abdominal procedure. Although these definitions were developed to apply to human patients, they apply unmodified to veterinary patients as well. The use of standard definitions is important for making comparisons between reports of surgical site infection incidence and risk factors. Control of surgical wound infections might be enhanced if efforts are focused on high-risk groups. Table • 10-1 U.S. Centers for Disease Control and Prevention Criteria for Defining Surgical Site Infections28 In an effort to describe high-risk groups, operative procedures are classified on the basis of the expected degree of bacterial contamination, as determined by guidelines developed by the National Research Council (NRC)(Table 10-2).36 Although surgical site infections occur more often as wounds become more contaminated (Table 10-3), this classification scheme does not always provide an accurate separation of animals. Excessive variation can be seen within these broad categories, and surgical procedures within the same category can vary widely in their associated postoperative infection rates. For example, dogs undergoing clean elective orthopedic procedures can have a surgical site infection rate as high as 15%,58 which generally is much higher than the range reported for clean wounds.7,12,21,55 Therefore, although the degree of contamination as described by the NRC may be one important factor associated with postoperative infection, many other factors can affect wound healing and infection rate. Table • 10-2 Wound Classification System as Described by the National Research Council, Division of Medical Sciences36 Table • 10-3 Range of Reported Surgical Site Infection Rates in Veterinary Patients (Dogs and Cats) According to the National Research Council Wound Classification36 System Animals whose incision sites are clipped sometime during their hospitalization other than immediately preoperatively are more likely to develop a surgical wound infection.7,12 Scanning electron microscopy shows that skin prepared with an electric clipper tends to have nicks at the creases, producing gross cuts into which bacteria can colonize over time.25 In one study, animals that were clipped within 4 hours of the induction of anesthesia had an equally significant increased risk for surgical site infection as those that were clipped more than 4 hours before the induction of anesthesia.12 This suggests that clipping of the skin anytime other than immediately preoperatively, even just the morning of surgery, should be avoided whenever possible. The normal immune response to surgery is self-protective and necessary for wound healing but may contribute to the development of surgical site infections.50 Suppression of the immune system results in part from a significant decrease in total lymphocytes, CD4+ T-lymphocytes, and CD8+ lymphocytes, and is directly correlated with the duration of surgery.19 In addition, lengthier operations expose the wound to a microbiologic environment for a longer period of time and generally involve more extensive tissue handling with increased use of suture material and electrocoagulation, which can reduce the local immune resistance of the wound.2,10,11,21 In dogs and cats, the risk of surgical site infection approximately doubles for every hour of surgery time.7,12,21,37 Because the duration of surgery can be a significant factor in modulating the immune response, predisposing the animal to postoperative complications with wound healing and infection, it is advisable to limit the surgery time as much as is reasonable. The duration of anesthesia can be a risk factor for surgical site infection independent of the duration of surgery, with a 30% greater risk of wound infection for each additional hour of anesthesia.7 In many cases, the duration of anesthesia is dependent on the duration of surgery, but in some instances, the duration of nonsurgical anesthesia time is much longer than surgical anesthesia time. Long patient preparation times; preoperative and/or postoperative diagnostic imaging procedures such as computed tomography (CT), magnetic resonance imaging (MRI), and radiographs; dental cleanings; and ear flushes while the animal is still under general anesthesia all may fall into this category.7 Increased risk of surgical site infection resulting from anesthetic duration is likely multifactorial. Aside from the contribution of the time that the surgical wound is open, prolonged exposure to anesthetic drugs may predispose to increased wound infection rates. For example, halothane anesthesia depresses neutrophil chemotaxis, phagocytosis, and oxidative function in proportion to anesthetic duration.15 Other mechanisms by which anesthesia could affect the immune response and the incidence of wound infection include extrinsic contamination of anesthetic drugs, particularly propofol,* inhibition or stimulation of cytokine secretion,11,17,23 increased numbers of CD8+ suppressor/cytotoxic lymphocytes,11 and impairment of neutrophil chemotactic, phagocytic, and oxidative function.15,22,49 On the basis of these studies, limiting total anesthesia time, particularly in those patients with other significant risk factors for surgical site infection, is advisable. Propofol use can increase the risk of surgical site infection in dogs and cats.26 It is assumed that this increased risk is due to the fact that lipid-based emulsions such as propofol are capable of supporting rapid microbial growth and endotoxin production.6,10 Administration of a potentially contaminated solution may contribute to surgical wound infection or other patient morbidity. Among the anesthetic practices implicated are preparation of multiple syringes of propofol at one time for use throughout the day, reuse of the same syringe or infusion line on different patients, and use of syringes of propofol that had been prepared up to 24 hours beforehand. Contamination could, theoretically, also occur during the opening of a glass vial whose surface had not been disinfected.61 Strict aseptic technique in the preparation of the solution and prompt disposal of unused propofol are imperative to curtail the potential for extrinsic contamination. The presence of an endocrinopathy, particularly diabetes mellitus, has been associated with increased rates of infection for several conditions, including urinary tract infection and dermatologic disorders.41,43 Although the presence of diabetes mellitus has not yet been definitively associated with an increased rate of surgical site infection in dogs and cats, animals with hyperadrenocorticism and hypothyroidism have been shown, in one study, to be more likely to develop surgical site infection.37 Human patients with hyperadrenocorticism have alterations in natural killer (NK) cell activity and a total decrease in T-lymphocytes characterized by decreased numbers of T-helper cells (CD4), with an increase in T-suppressor cells (CD8) that is thought to result from downregulation of signal transduction through the interleukin (IL)-2 receptor. Contrary to the findings with dogs and cats, hypothyroid human beings have not been shown to be at increased risk of postoperative wound infection. Additionally, studies with mice have shown that an increase in activated T-cells actually occurs in the absence of thyroid hormone. Additional studies are needed to better define the risk of surgical site infection in dogs and cats compared with other species.37 For each additional person in the surgical suite, the risk of surgical site infection can increase by as much as 30%.21 The operating room environment, including the people involved in the surgical procedure and the traffic patterns, can be a source of contamination of the surgical field. Greater amounts of airborne contamination can be expected with increased numbers and activity of personnel.44,52 Given this, limitations on the number of personnel in the operating room may be useful for decreasing the risk of surgical site infection. The risk of developing surgical site infection can be greater for intact male dogs and cats.37 This parallels what is reported in men, who have more than a 50% greater risk of developing a major infection after surgery compared with women. This increased risk is believed to be a direct immunomodulating effect of androgenic hormones.38,51,59 Other risk factors for surgical site infection that have been studied in dogs and cats include the use of immunosuppressive medication, active infection distant from the surgical site, perioperative hypotension, perioperative hypothermia, body condition (i.e., malnutrition and obesity), blood loss, suture material, American Society of Anesthesiologists (ASA) preoperative assessment score, duration of hospital stay, and age.7,12,21,37 Although definitive evidence of an association between these factors and surgical site infection is lacking, in many cases the numbers of animals with these conditions in reported studies were too small to allow a definitive conclusion that an association does not exist. Other risk factors have been defined in human medicine where prospective epidemiologic studies of thousands of patients have been carried out, and some of these may be important to veterinary patients as well. For example, perioperative supplemental oxygen therapy may exert a significant beneficial effect in the prevention of surgical site infection. Oxidative killing by neutrophils is enhanced by high oxygen tension in the tissues, and several studies have investigated providing supplemental oxygen to increase intraoperative and early postoperative inspired oxygen concentrations in an effort to improve surgical site infection rates.2,45
Wound Infections and Antimicrobial Use
Definition of Surgical Site Infection
Risk Factors for Surgical Site Infection
Degree of Bacterial Contamination
NATIONAL RESEARCH COUNCIL WOUND CLASSIFICATION36
RANGE OF REPORTED SURGICAL SITE INFECTION RATES IN DOGS AND CATS7,12,21,55
Clean
2.0%–4.8%
Clean-contaminated
3.5%–5.0%
Contaminated
4.6%–12.0%
Dirty
6.7%–18.1%
Clipping of the Surgical Site
Duration of Surgery
Duration of Anesthesia
Propofol
Endocrinopathies
Number of People in the Operating Room
Sex
Other Potential Risk Factors
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



