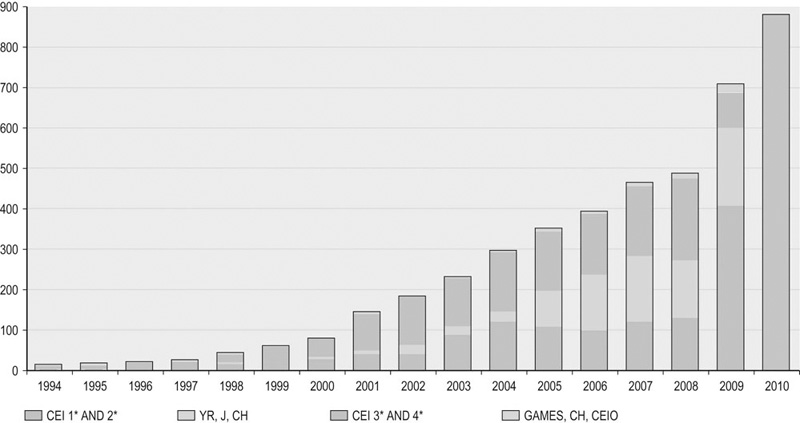
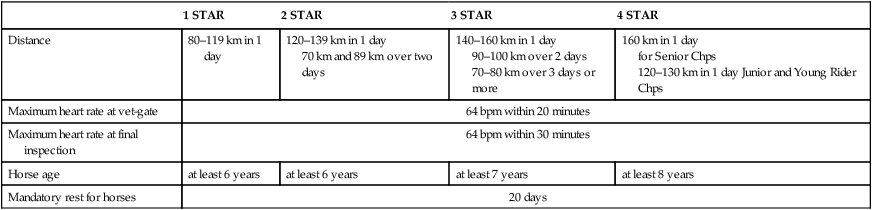
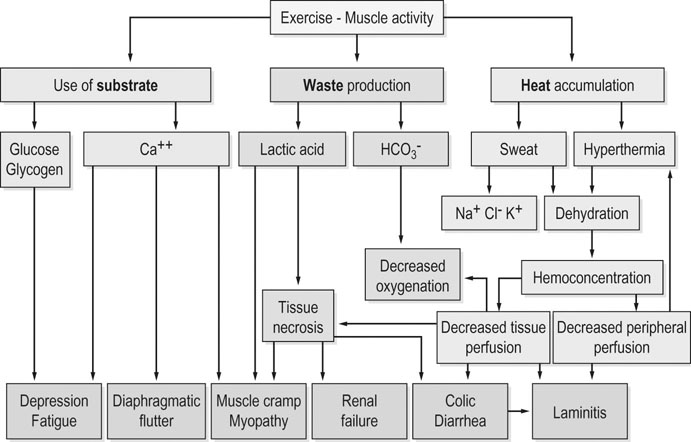
Endurance riding is a competition to test the competitor’s ability to safely manage the stamina and fitness of the horse over an endurance course in a competition against the track, the distance, the climate, the terrain and the clock.1 Endurance is the fastest-growing FEI discipline. The worldwide increase in endurance riding has brought many veterinarians into contact with this equestrian discipline. The trend of faster speeds associated with less technically demanding competitions in international events in comparison to national events is well recognized.2 This translates into much harder training of the horses than 15 years ago. The origin of endurance is related to the historical needs of men to communicate and transfer information from one place to another in minimum time. Postal services in Europe and America illustrate this view of the history of endurance. The example of the famous Pony Express, a 1900-mile route, which connected St. Joseph (Missouri) to Sacramento (California), announced the beginnings of the discipline. As horses used to be the main form of transportation, it was natural to seek a horse that was fit and healthy and had the predisposition to long distances. American and European cavalry used endurance tests as part of their military training, as horses had to be fast and robust to travel long distances and conquer territories. The first endurance competitions occurred during the 19th century in Europe, Australia and the USA. Race conditions were very different from those we know today and the health of animals on arrival were not at all taken into account. In the 1900s, horses were still used in military activities that involved endurance exercise, notably the Brussels Ostend military raid of 1902, run over 132 km at 19 km/h average speed. The sport developed during the second part of the 20th century, with the famous 100-mile (160 km) Tevis Cup Ride that has been run every year since 1955, and the Florac race that was created in 1975 in France. In 1982 the FEI approved Endurance Riding as an official discipline and gradually the number of rides increased. In 1998, the World Championships were held in the United Arab Emirates (UAE). Thanks to the sponsorship of the UAE National Federation, 47 national federations came from all over the world to compete.3 The sport has subsequently undergone tremendous growth internationally. Over the past 12 years, endurance has been the fastest-growing FEI discipline, with 879 international events held in 2010 as opposed to just 63 in 1999 (Fig. 52.1). One event can have several classes, which have specific criteria, such as distance and whether only young riders (aged ≤21 years) are allowed to participate. An ongoing study4 using the FEI database revealed that in 2008 there were 7017 starters at FEI rides of ≥100 km distance. Horses from nine countries, selected based on the anecdotally high number of endurance rides/riders and/or their tradition in endurance riding (Australia, France, Italy, South Africa, Spain, UAE, UK, Uruguay and USA), represented 61.7% of all starters. The greatest number of entries was recorded in the UAE (1497 in total), followed by France (1029) and Spain (408). The mean number of entries per class varied between 10.3 (South Africa) and 71.3 (UAE). The suitability of pure Arabians and Arabian crosses is well recognized for long-distance aerobic exercise. However, most endurance rides are open to horses of other breeds and in FEI Endurance Rules, any member of the Genus Equus counts as a ‘horse’.1 In a recent study5, some breeds including Appaloosas, Missouri Fox Trotters, Tennessee Walking Horses, Quarter Horses, and Thoroughbreds, were all considered to be at higher risk for metabolic elimination, compared with Arabians. Previous studies6,7 have found physiologic differences between Arabians and other breeds during race training. Arabians tend to be smaller and much thinner than their larger, more muscled Thoroughbred racing counterparts; they have a lower body mass index than Appaloosas and Quarter Horses; these factors likely favor thermoregulation during endurance exercise. In endurance competition, the emphasis is placed on the horse finishing in good condition, rather than who finishes first. This explains the stringent rules with regards to veterinary checks throughout the race. The competition consists of a number of sections known as ‘phases’. According to FEI rules, no phase may exceed 40 km and should, in principle, be not less than 20 km in length. At the end of each phase, there will be a compulsory halt for veterinary inspection. These halts are operated by establishing a vet gate with an inspection area that the competitors enter with the horse when they decide that the horse is ready to pass the veterinary inspection. However, before the scheduled presentation time has elapsed, the horse must demonstrate its fitness to continue which is assessed upon three criteria: pulse recovery, metabolic stability and gait. The time spent at each vet-gate prior to inspection by the vets is counted as part of the overall competition time and the aim is to determine whether the horse is fit to continue the ride. Veterinary inspection is followed by a compulsory rest period, or hold time that varies between 30 and 60 minutes, depending on the number of phases and length of the ride. An endurance ride is a competition against the clock. The combination that finishes the course in the shortest time will be classified as the winner of the competition after successfully completing all final Veterinary Inspections.1 The International Endurance Rides are divided into CEI (Concours de Raid d’Endurance International) and CEIO (Concours de Raid d’Endurance International Officiel). They are governed by the General Regulations, the Veterinary Regulations of the FEI and the rules for endurance events.1 CEIs are divided into four different star levels. Characteristics of each type of CEI are described in Table 52.1. Table 52.1 Characteristics of the four levels of International Endurance Rides defined by the FEI Chps = Championship, bpm = beats per minute. Unlike other equine disciplines, many veterinarians are present in endurance events. The Veterinary Commission has absolute control on all matters concerning horse safety, health and welfare. The Veterinary Commission is appointed by organizing committees; it is composed of a President of the Veterinary Commission, a Foreign Veterinary Delegate (for FEI-sanctioned endurance rides) and members whose number depends on the level of the race and the number of starters. One or more treating veterinarians are in attendance to provide emergency care at the event. Team Veterinarians are appointed by their national federation and are responsible for the health and welfare of team horses and, if requested, of individual competitor’s horses. Individual competitor’s private veterinarians can assume any function in the care of private competitors’ horses. Finally, testing veterinarians are specifically responsible for carrying out medication control in certain geographical areas.8 The Veterinary Commission works in coordination with other officials. The Ground Jury will supervise all arrangements made by the Organizing Committee for the judging, veterinary control and timekeeping of the competition. The Technical Delegate must, in coordination with the Organizing Committee, check and approve, in advance, the layout of the course, the technical and administrative arrangements for the conduct of the event, for the examinations and inspections of horses, for the accommodation of horses and riders and for the stewarding of the event. He will supervise the briefing(s) and the conduct of all technical personnel. The Chief Steward is responsible for the organization of stewarding throughout the event.1 The first examination aims to establish the horses’ identity (passports, registration documents, etc.) and to evaluate the general health of the horse, and in particular, to identify any contagious conditions. For most races, this examination is coupled with the first inspection that usually takes place on the day preceding the start of the competition.8 At the end of each phase, veterinary examination is conducted according to the same standards from the beginning of the ride to final inspection. It includes evaluation of heart rate, respiratory system, mucous membranes, gut sounds, soreness, lacerations or wounds, shoes and feet, gait and range of motion. Horses with abnormally high pulse rates, or pulse rates higher than the parameters defined in the schedule will not be allowed to continue in the competition (Table 52.1). Abnormalities in rate or character of breathing of such a nature as to endanger the safety of the horse, generally poor condition or abnormally high temperature will be cause for elimination. Any abnormal heart sounds, evidence of soreness, lacerations and wounds in the mouth, on the limbs and on the body, including girth and saddle galls, must be recorded. If participation in or continuation of the competition is bound to seriously aggravate any injury, the horse will not be allowed to continue. A recent study that evaluated performance and health indicators during a 160-km ride (elimination vs success) in 48 horses confirmed that this standardized veterinary examination allowed veterinarians to detect metabolically compromised horses.9 At any inspection during the course, a horse with an irregularity of gait, which must be consistently observable through evaluation by trotting the horse on a loose lead in hand straight out and back, without prior flexion or deep palpation, will be removed from competition. An individual veterinary card issued before the first inspection is to be completed after each inspection. Endurance is an exercise at a moderate speed, over the long term.10,11 The energy required for the effort mainly results from aerobic metabolism of fatty acids and glycogen in slow-twitch and intermediate contraction muscle fibers.10 Aerobic capacity of a horse can increase with training, but is also influenced by breed; it seems to be lower in Andalusian when compared to Arabian and Anglo-Arabian horses.12,13 Beyond a certain speed, there will be an increase in anaerobic metabolism.10 This speed varies between 18 and 36 km/h depending on the horses and its state of physical conditioning.11 Endurance exercise leads to the generation of considerable intramuscular heat. Only about 20–25% of the energy expended by muscle metabolism is converted into mechanical work while the remaining 75–80% is dissipated as heat.11,14–16 Horses competing in endurance rides produce a metabolic heat load that could raise core body temperature by 15°C/hour if mechanisms of heat dissipation did not exist.17 Since core temperature increases only 1–3°C during the course of several hours ride,14 it is clear that the majority of metabolic heat produced is dissipated. Intramuscular heat must be shed to the external environment via shifts from muscle toward the skin with peripheral vasodilatation and increased skin temperature. The skin is then cooled by convection (wind currents), radiation (to a limited extent), and especially by the evaporation. In horses, heat dissipation occurs primarily by the production and evaporation of large volumes of sweat (65%), followed by respiratory evaporation (25%).18,19 Sweat production has been estimated to reach 10 to 15 L/hour in endurance horses run at 16 km/h, but sweating rates may be up to 50% greater (and total sweat production may be 100% greater) when horses are exercised under hot and humid conditions.18 Field studies of endurance rides have shown body mass losses (a reasonable reflection of fluid losses) ranging from 3 to 7% at the end of 80–160-km rides.20,21 It is well known that equine sweat is hypertonic with respect to plasma osmolarity. Sweat contains relatively low levels of calcium, magnesium and phosphate but relatively high levels of sodium, potassium and chloride.18 Sodium concentrations in sweat and plasma are equivalent.10,22 In response to dehydration, Na+ ions are reabsorbed in the kidney in exchange for K and H+ ions. However, with substantial loss of Na+ homeostasis is disturbed and the circulatory system is affected. This can be responsible for a decrease in blood pressure and increased capillary refill time and heart rate.10 K+ losses in sweat are very high; they are worsened by the mechanisms of renal sodium reabsorption. In addition, during the race, due to the elevation of blood cortisol levels related to stress, loss of K+ in sweat and urine is increased. The loss of Cl− ions in the sweat is the sum of losses in Na+ and Cl−. Cl− is normally the primary ion reabsorbed by the kidneys. When the Cl− concentration decreases, bicarbonate ions (HCO3−) are reabsorbed to maintain the anion gap within its normal range.15 Calcium and magnesium contents in the sweat are greater than that of plasma. Sweating losses therefore can contribute to hypocalcemia and hypomagnesemia. The practice of electrolyte administration by owners has significantly changed over the last 10-20 years; these practices may affect biochemical derangements currently identified on rides. Decreases in plasma [Na+], [K+], [Cl−] and [Ca++] are usually described at the end of the ride as compared with pre-ride values.17,20,21,23 The magnitude of the fluid and electrolyte losses appears to be more marked in exhausted than in successful endurance horses.24,25 Increasing speed, the presence of muddy terrain and increasing temperature contribute significantly to ion losses during endurance rides.22,25 The endurance horse rarely develops metabolic acidosis. Aerobic metabolism associated with a moderate effort over the long term does not lead to a substantial increase in lactic acid levels nor a decrease in pH.14 However, because of thermoregulatory mechanisms, the endurance horse may develop both metabolic and respiratory alkalosis.15 In an attempt to maintain normal anion gap during exercise, bicarbonate is retained when potassium is unavailable for sodium exchange in the distal tubule, resulting in a metabolic alkalosis.16,26,27 The increased respiratory effort to dissipate heat with concomitant loss of carbon dioxide results in some degree of respiratory alkalosis, particularly in hot environments.15 A recent study28 demonstrated that endurance horses frequently develop a complex acid–base imbalance characterized by mild strong ion alkalosis (due to hypochloremia), non-volatile buffer acidosis (due to increased plasma albumin concentration) and mild compensatory respiratory acidosis. The capacity for endurance exercise is highly dependent on the availability of substrate for the synthesis of adenosine triphosphate (ATP), the body’s energy currency. The endurance horse travels at speeds that can be maintained almost entirely by aerobic metabolism, with glucose and fatty acids the primary substrates for ATP re-synthesis in muscle. Glucose is derived from the breakdown of liver and muscle glycogen and de novo synthesis of glucose in the liver. Muscle glycogen is the primary carbohydrate reserve. Muscle glycogen is initially mobilized in slow-twitch fibers, followed by fast-twitch fibers.15 Intramuscular glycogen depletion occurs with endurance exercise in horses.29,30 Once glycogen has been fully depleted, there is little in the way of intracellular substrate for energy production, and muscular exercise often slows or stops. Free fatty acids derived either directly from muscle triglycerides or released from adipose tissue are an important source of energy for aerobic metabolism.10,14,26 In the context of endurance exercise, the endogenous store of triglycerides is virtually inexhaustible. Their utilization allows a sparing of muscle glycogen reserves, a reduction in lactic acid accumulation and possibly help to delay the onset of fatigue.14 A number of studies have reported that exhaustive endurance races induce accelerated generation of reactive oxygen species (ROS). ROS result in lipid peroxidation, which induces adverse effects on the health status and performance of horses.31,32 Both lipid peroxidation and Ca++ are important contributors to cell damage caused by physical injury or ischemia. Shortly after the onset of ischemia or physical injury, the extracellular Ca++ concentration falls dramatically, resulting in intracellular Ca++ accumulation, causing activation of some Ca++-dependent enzymes that may damage the DNA and cleave structural proteins within the cell. Cells can tolerate mild oxidative stress and often respond by raising their level of antioxidant defenses. However, severe oxidative stress and high concentrations of free radicals may produce serious disturbances in cellular structure and metabolism.32 Horses participating in endurance rides must maintain healthy homeostatic mechanisms while optimizing performance. These horses perform for hours over uneven terrain, and often in less than ideal environments (hot, humid weather; cold, chilling winds; rocky, mountainous country; and deep sand or mud). Mechanical problems that must be addressed include stresses applied to muscle, tendon, ligament, and bone that can cause lameness. Metabolic problems that must be overcome include fuel substrate depletion, dehydration, excessive hyperthermia, electrolyte loss, and body pH changes that can result in metabolic disease.33 A high elimination rate from endurance rides has been a regular matter for discussion in professional and public forums; moreover, in recent years, elimination rates seem to have increased.4 Reported elimination rates range from 10% to 60% depending on the course and speed.5,21,23,34–37 In both national and international venues, the primary reason for elimination from endurance competition is lameness. In a study based on records of all sanctioned 2007 endurance horse competitions (40 to 160 km) in the USA, the overall elimination proportion for the number of starts in the study was 18.9% (660/3493), with 147 horses eliminated for metabolic reasons and 312 horses eliminated for lameness.5 The largest and most recent study, based on 2008 FEI records for 9 countries from the 5 continents, confirms these tendencies.4 Data for 4326 endurance ride starters were collected, of which 1991 finished the ride (46.0%). The most common reason for not completing the ride was elimination (45.9%), although 8.1% of all started horses were retired. The highest completion rates were recorded in Australia (63.9%), USA (63.6%) and South Africa (57.6%). There were 3 countries where fewer horses completed the ride than were eliminated: the UAE (34.1%), Uruguay (46.3%) and UK (43.2%). In agreement with results of previous studies,38 lameness was the most frequent cause of elimination in all countries: eliminations for lameness represented 69.2% of all eliminations (31.8% of all entered horses). Eliminations for metabolic reasons accounted for 23.5% of all eliminations (10.8% of the starters). The ratio between elimination for lameness and metabolic reasons varied between countries, but lameness was at least twice as common as other reasons for elimination in all countries.4 While several epidemiological studies have been published investigating risk factors for wastage and/or injuries in Thoroughbred racehorses, there are few data available for endurance horses. The frequency of medical problems encountered in endurance events depends mainly on the temperature and humidity on race day. Under temperate conditions, medical problems are infrequent and represent about 20 to 25% of eliminations.38 When the temperature exceeds 25°C and humidity 70%, metabolic disorders may account for more than half of the causes of elimination. Multivariable analyzes performed on the 2008 FEI data revealed that the risk of elimination due to lameness or for metabolic reasons was significantly associated with country.4 Several countries had increased risk for horses being eliminated for metabolic reasons compared with Australia, where the lowest elimination rate for metabolic reasons was recorded. If the number of entries was ≥80, then horses were at an increased risk of elimination for lameness (OR = 1.60, P = 0.002) than in rides where the number of entries was <80. The number of entries in the ride was also significantly associated with the risk of elimination due to metabolic reasons. No evidence was found for a significant effect of distance on elimination for either lameness or metabolic reasons. AERC records from the ride year 2007 showed that the overall ride distance was associated with increased risk of elimination.5 An interesting finding in that study was that abnormalities in capillary refill time, overall impression by the veterinarian, and gastrointestinal sounds prior to the start of competition were all associated with failure during the ride. Abnormalities in gait prior to the start of the ride were not identified as a risk factor for lameness elimination (or other type of elimination). The welfare of endurance horses depends on the knowledge and skill of their riders and is protected through evaluation of horses by veterinarians before, during, and after these events. The philosophy of veterinary inspections is to pull any horse showing several signs of fatigue, but to let a horse with inconsistent lameness continue.39 The cardiac recovery index used in the vet gates as a supplementary examination during the last phases of a ride; this method is useful for the early recognition of metabolic problems.36,39,40 Equine welfare is further protected by standards set by the FEI. These standards include requiring horses to be fully mature before they are allowed to compete, requiring that horses be ‘fit to continue’ at all veterinary examination points, and requiring that horses not be under the influence of drugs or other performance-enhancing modalities during competition.33 Although musculoskeletal injuries may occur at any point along an endurance ride event, the most pressing emergency situations generally involve metabolic problems. Endurance rides combine a lengthy duration of continuous exercise with resultant loss of body fluids and electrolytes. Coupling this with additional demands placed on these horses from speed, challenging terrain, and possible adverse weather conditions, the most prevalent metabolic concerns fall under the umbrella of a complex known as exhausted horse syndrome (EHS). The fluid and electrolyte losses in EHS result in decreased fluid volume and increased blood viscosity, which can lead to inadequate tissue perfusion (Fig. 52.2). Renal hypoperfusion coupled with the adverse effects of circulating myoglobin (due to muscle injury) may lead to impaired renal function and occasionally to renal shutdown. Decreased substrate availability in muscle may lead to tying-up.41 Decreased intestinal perfusion may contribute to, malabsorption of orally administered fluids and sometimes diarrhea. Fluid loss from diarrhea and endotoxemia may further compound the problem of dehydration, shock, and laminitis. Conversely, impaction of the large colon or caecum may occur due to the severity of the dehydration and the mobilization of water reserves from the colon in an attempt to maintain circulating blood volume.15,16 The distal limbs may be most susceptible to the combined effects of dehydration and initiation of intravascular coagulation, leading to the development of laminitis. Substantial electrolyte losses may also promote neuromuscular irritability, with spontaneous muscular activity (muscle fasciculation), heart arrhythmias and synchronous diaphragmatic flutter.15,16,42 Dehydration also compounds the problem of heat retention, because the horse has less extracellular fluid available to circulate heat to the skin surface and to make sweat in order to lose heat by evaporation16, thus exacerbating the problem of overheating in exhausted horses.15,41 In summary, a sick horse may be affected with myositis, synchronous diaphragmatic flutter, colic, and heat stress or prostration, and also has the potential to develop laminitis.43 There are all degrees of metabolic compromise, ranging from very mild and barely detectable to extremely serious and life threatening. Dehydration can be severe enough to lead to hypovolemic and circulatory shock, resulting in a cascade of pathophysiologic events which may be irreversible, despite all attempts at therapy.15 There is little information available on the specific types of metabolic problems (and their outcomes). A recent study on 30 cases identified during the 2005 and 2006 Tevis Cup rides reported colic (40%), poor recovery (23%), myopathy (23%), synchronous diaphragmatic flutter (10%) and choke (3%).44 In a study on 16 of the 20 CEI** and CEI*** events held in France in 2003, the proportion of horses requiring treatment varied between 4.2 and 16.4% depending on the ride.45 On average 10.5% of the competitors received medical treatment for metabolic reasons. Metabolic eliminations and the need for treatment were more frequent in the latter stages of races (from the 3rd vet-check, e.g. 90 to 100 km). Of a total of 105 horses treated for metabolic disorders, diagnoses were dehydration and poor recovery (30.5%), colic (20.0%), exhaustion (15.2%), myopathy (19.0%), synchronous diaphragmatic flutter (7.6%), laminitis (4.8%) and heat exhaustion (2.9%). About two-thirds of treated cases were considered of mild or moderate severity. However, the other ones (corresponding to 3% of the competitors) were rated as marked or severe and potentially detrimental to the horse’s athletic career.45 Exhaustion is due to the compound effects of dehydration, electrolyte imbalances, heat accumulation, energy depletion and acid–base imbalance (i.e. base excess and alkalosis).41,46,47 The onset or development of endurance fatigue is particularly sensitive to the effects of increased ambient heat and humidity.15 A horse at the initial stages of EHS may exhibit very subtle indications of any or all of the following signs: unstable heart rate, lack of impulsion, lack of attentiveness, lack of interest in food and water, glassiness of the eyes, increased skin tenting retention, increased jugular refill time, absent borborygmi, concentrated or absent urine.41 A poor cardiac recovery (i.e. pulse fails to return toward normal after the cessation of exercise) should always alert the clinician to the possibility of EHS. One or more of the following clinical signs may be present: persistently elevated pulse (>60 beats/min after 30 min rest)19 and respiratory (>40 breaths/min after 30 min rest) rates19, depression, complete anorexia, unwillingness to continue exercise, elevated temperature, delayed capillary refill time and/or pale or marginated mucous membrane color, decreased pulse pressure and jugular distensibility, minimal but quite concentrated urine, dry feces.15,19,43,46,47 Further signs may be atonic bowel, dilated anus, occasional colic, cardiac irregularities, muscle cramps with or without associated lameness, and synchronous diaphragmatic flutter.15,43,46 Other less common signs include atrial fibrillation, diarrhea, rhabdomyolysis, recumbency and laminitis.41 Exhausted horses usually show a high degree of dehydration, with high packed cell volume, total protein, albumin and creatinine values, which could indicate a failure of compensatory fluid shift from the intracellular compartment in response to severe dehydration.24,25,47 Hematology usually reveals increased RBC count, stress neutrophilia and lymphopenia. Most serum electrolytes are decreased (K+, Cl−, Ca++, Mg++ and sometimes Na+). Other changes include elevated CK, AST and LDH from muscular origin. However, electrolyte disturbances and laboatory evidence of muscle damage tend to be mild and do not necessarily aid in delineating sick horses from successfully completing horses.25,44 Diagnosis is based on the horse’s history, clinical signs and laboratory findings. The most difficult task regarding EHS is recognition of the earliest stage of the condition. A severe case is easy to diagnose, but the goal of the endurance ride control veterinarian is to intervene in an impending EHS case while allowing well-adapted horses to continue performing. A hallmark of EHS is the horse’s inability to replace fluid and electrolyte deficits by voluntary consumption of feed and water. Careful observation is essential in identifying the progression of clinical signs in horses that require aggressive therapy from those horses eating and drinking, which may equilibrate with non-invasive supportive care.41 Treatment is based on replacing fluid, electolyte and substrate and returning the horse to a state of adaptative equilibrium (see below ‘General considerations’). EHS usually responds to prompt vigorous treatment, but also can lead to death due to renal failure (especially if it is treated with customary doses of NSAIDs), hypovolemic shock, pulmonary edema, disseminated intravascular coagulation, diarrhea, or laminitis.15,47 Occasionally endurance horses will develop a post-exhaustion syndrome, which can be fatal. On the ride these horses show excessive fatigue and delayed recovery.46 The condition of these horses seems to stabilize after treatment and they are generally permitted to depart. At home, they may remain, however, depressed and have little appetite. At presentation a few days later, they are severely depressed, weak, stiff, and reluctant to move. Clinical signs described above are still present: increased pulse and respiratory rates, dehydration, diminished gastrointestinal motility, and sometimes cardiac irregularities and/or severe, rapidly progressive laminitis. Major serum chemistry abnormalities are usually seen. The most consistent findings are elevated creatinine, bilirubin, liver (γGT) and muscle enzymes (CPK and AST) and marked hypochloremia and hypokalemia. Many of these horses die despite intensive supportive care.46 SDF, commonly known as ‘thumps’, is the synchronous contraction of the diaphragm with the heart beat. This condition has been reported in horses with gastrointestinal disease, sepsis, lactation tetany, blister beetle toxicosis, endurance exercise, hypoparathyroidism, and alkalosis.48 Normally, half the blood calcium exists in the ionized, active form, while the other half is protein bound. Exercising horses can develop a state of alkalosis from hyperventilation,48 massive chloride ion loss caused by prolonged sweating or inappropriate bicarbonate administration.49 Alkalosis can result in hydrogen ion shifts and exposure of negative charges on serum protein molecules, which subsequently bind Ca++ and Mg++ resulting in a relative ionized hypocalcemia and hypomagnesemia with normal total Ca and total Mg values.27,48,49 Lack of calcium allows sodium to diffuse spontaneously into the nerves, increasing nervous irritability and resulting in involuntary muscle contraction and fasciculation. Depolarization of the right atrium stimulates action potentials in the hyperexcitable phrenic nerve as it crosses over the heart.48 This action will cause the diaphragm to contract, resulting in the abdominal muscles contracting in synchrony with the heart rate.15,16,27 SDF often occurs following a rest stop because, if the horse is rehydrated without electrolyte intake, the fluid replenishment further dilutes Ca++ and K+ and exacerbates alkalosis. SDF is recognized by a twitching or convulsive motion in the flank area, almost like a hiccup, either unilaterally or bilaterally.15 This abnormal diaphragmatic activity is in unison with the heart rate and not the respiratory rate.15,27 Careful observation is necessary for appropriate diagnosis in the horse with an elevated respiratory rate as the horse recovers from exercise.15 Other physical parameters may be within acceptable limits or the condition may occur as part and parcel to the exhaustion syndrome.27 Blood analysis usually reveals low Ca++ values. In a recent study,32 comparing blood values measured before the start of the race and at the 90-km check point in 9 horses eliminated for SDF and 9 finishers, there were no significant differences detected between the two groups for Na+, K+ and Cl− concentrations whereas ionized calcium values were lower and lactate concentrations higher in SDF-eliminated horses. The increase in lipid peroxides and malondialdehyde between pre- and post-exercise values was also greater in SDF eliminated horses.32 The condition may resolve spontaneously with rest50 or after the correction of electrolyte and acid–base imbalance and rehydration.49 If the bowel is functional, treatment involves administration of oral fluids containing calcium and potassium.27 Parenteral administration of balanced non-alkalizing fluids with calcium gluconate often speeds recovery.27,50,51 However, hypocalcemic patients with concurrent hypomagnesemia are often refractory to calcium therapy unless the low serum magnesium concentrations are identified and corrected.49 Intravenous administration of magnesium (as MgSO4)49 and dextrose-containing solutions51 may therefore be necessary. SDF is a recurrent problem in some horses.51 Preventative measures should include electrolyte supplementation during the course of the event. Horses prone to development of SDF should have their dietary ratio of calcium and phosphorus adjusted around 1 : 2.27 This adjustment precludes the feeding of alfalfa or other legume hay as the Ca/P ratio is deviated from the ideal depending on quality.27,51 Some horses with chronic recurring SDF may have alterations of the phrenic nerve. Injury or scar tissue subsequent to pneumonia or pleuritis is a potential but unproven cause of refractory cases of SDF.51 Anecdotally, osteopathic manipulations have also been reported to reduce the occurrence of SDF in some horses; in these cases, low cervical vertebral lesions or instabilities might be suspected. Endurance horses appear to develop exertional myopathies (EM) in two circumstances: early after the start of the race (type A), or further into the race in conjunction with exhaustion (type B).52 Type A myopathy usually occurs within the 5–20 minutes following commencement of exercise. EM is well documented in Thoroughbred and Standardbred racehorses, and often is associated with anxiety or improper feeding management.2 Certain Arabian family lines also seem to be predisposed to recurrent EM. Polysaccharide storage disease has been anecdotally reported in Arabian horses.52 Metabolic myopathy (type B) develops later in the ride, in conjunction with exhaustion due to electrolyte abnormalities, glycogen depletion, etc.,14 and possibly compounded by abnormal muscle recruitment patterns that represent compensation for a newly developed unilateral lameness.15 Exercise over difficult terrain and under cool, damp conditions also predisposes animals to EM. Clinical findings vary from simple muscle soreness to paralytic myoglobinuria.46 Affected horses are generally anxious, in pain, and exhibit tachycardia and tachypnea, reluctance to move, and gait abnormalities ranging from stiffness and shortened stride to significant lameness and recumbency.14,53 Localized or more diffuse muscle cramping, hardening, stiffened, pain on palpation, and focal sweating are characteristic of exertional myopathy.15 Muscle spasms may occur but are not consistently found.46 Hindlimb and lumbar muscles are the most commonly affected (Fig. 52.3), but forearm or pectoral muscles may also be involved.2,50 Myoglobinuria is observed in moderate to severe cases. The diagnosis of EM is based on clinical signs of muscle stiffness and pain after exercise in conjunction with elevations in serum creatine kinase (CK) and aspartate transaminase (AST) activities. The degree of elevation of muscle enzymes in serum is dependent on the severity of muscle damage as well as the length of time that has elapsed between the sample collection and the occurrence of muscle damage.53 However, pain and muscle swelling are not associated with CK activities; in a recent study on 22 horses that successfully completed a 160-km ride, there was no concentration difference between finishers and non-finishers.37 Affected horses must be stopped and treated to relieve anxiety and muscle pain and replace fluid and electrolyte losses.2,53 Severe rhabdomyolysis can lead to renal compromise because of the ischemic and combined nephrotoxic effects of myoglobinuria, dehydration, and non-steroidal anti-inflammatory drugs (NSAIDs). In mildly dehydrated horses, provision of free-choice electrolytes and water or administration of fluids through a nasogastric tube may be adequate. Horses with moderate to severe dehydration require IV administration of balanced polyionic electrolyte solutions. Hyperkalemia can occur with severe EM, necessitating the use of isotonic sodium chloride. If hypocalcemia is present, supplementation with calcium borogluconate is recommended.53 In severely affected animals, regular monitoring of serum creatinine is advised to assess the extent of renal damage. Tranquilizers such as acepromazine, xylazine, or detomidine with or without butorphanol provide excellent sedation and analgesia, and are safer compared to high doses of NSAIDs, considering the likelihood of significant concurrent dehydration.2 Doses of flunixin meglumine and other toxic NSAIDs should be minimized in the face of dehydration. For severely affected horses, IV dimethyl sulfoxide (as a <20% solution) may be used as an antioxidant, anti-inflammatory agent, and osmotic diuretic;53 in these horses, the administration of Dantrium (dantrolene sodium; 2–4 mg/kg orally) may also decrease muscle contractures and possibly prevent further muscle necrosis. Horses that have had EM may recover without any further muscle problem. Others may have muscle fibrosis and loss of muscle mass, leading to gait abnormalities and disfigurement.50 In severe cases the myocardium may be affected also with potentially life-threatening consequences.16 EM is a syndrome with many causes.53 Finding ways to reduce stress is recommended to help decrease episodes of myopathy in susceptible horses. Modification of diet and training regimens can also decrease the likelihood of recurrence. A nutritionally balanced diet with appropriate caloric intake and adequate vitamins and minerals are recommended (see Feeding management). Although ileus has been hypothesized as the most likely cause for colic in endurance horses, gastric ulcerations and impaction have also been implicated.54,55 In a retrospective study on 36 horses presented for colic within 48 h of an endurance ride in two equine referral centers in the USA, a diagnosis of open or ileus was made in the majority of horses (56%). During exercise there is re-distribution of blood flow away from abdominal viscera to the muscles and skin.16,56 Reasons for ileus may include electrolyte derangements, dehydration leading to decreased intestinal perfusion and other unknown factors.55 Exercise has also been shown to result in increased intra-abdominal pressure in horses which was postulated to have a role in the development of gastric squamous mucosal ulcers.56 In one study of endurance horses, gastroscopy was performed after the horses completed 50-km and 80-km rides.54 Twenty-seven percent of the horses had bleeding of the gastric glandular mucosa after the competition, a prevalence that is higher than in most other endoscopic reports on horses. The inference was that the gastric glandular mucosal bleeding may have been a sequel to the strenuous endurance rides. Salmonella infection may also represent a significant cause of colic in endurance horses.55 In the study presented above, salmonellosis and enteritis (Salmonella negative) were recognized in 16% of the patients. Most endurance horses with signs of colic during or post-ride have decreased gastrointestinal sounds on presentation. Abdominal ultrasonographic examination can be performed to identify signs consistent with exercise-induced ileus: distended and non-motile small intestine with a normal wall thickness.46 Amounts of gastric reflux can be substantial.55 As such, it is imperative that nasogastric reflux is checked in all endurance horses with colic.47 Rectal examination has to be performed to minimize risk of rectal tearing that may be increased due to dehydration. Rectal examination usually reveals only hard and dry manure, sometimes distended intestine or nothing remarkable. Surgical lesions are uncommon despite significant abdominal pain,44 and therefore medical management appears a viable option in most cases.55 Endurance horses pose unique challenges as they often have severe derangements of hydration and electrolyte parameters that may be related to the competition and not necessarily to the cause of colic.55 Large amounts of IV fluids may be required to replace ongoing losses and deficits. If colic signs continue or recur, assessment for gastric reflux should be repeated because the volume of intestinal fluids can increase once the horse is rehydrated.47 Usual medical treatment includes IV sedatives (detomidine or xylazine, butorphanol) and flunixin meglumine. Depending on race location and conditions, horses will receive treatment in the field or be presented to referral hospital for emergency medical care; in some cases hospitalization may be prolonged. However, colic in endurance horses appears to have an excellent prognosis. In the retrospective study on 36 horses presented in two equine referral centers, all horses survived but one.55 Central nervous system disorders can accompany metabolic disturbances in endurance horses. The exact origin of these disorders is unknown: hyperthermia, hypocalcemia, hyperammonemia, hypoglycemia and hyponatremia have been suspected. In a small case series of horses that developed neurologic abnormalities at the end of a CEI3*, all horses had shown discrete signs of poor performance on the loop prior to the onset of the problem: reduced speed on the track and increased recovery time at vet-gate presentation.57 Heat stroke occurs when the normal thermoregulatory processes fail. It is accompanied by clinically apparent disturbances in water and electrolyte balance and clotting mechanisms. The pulse becomes weak, with congested mucous membranes19 and the horse shows signs of restlessness, dullness and incoordination.46 It may be agitated and become violent or ataxic and collapse.19 Respiratory rate can be elevated above the heart rate.19 Hyperammonemia-associated encephalopathy is usually secondary to intestinal disease or dysfunction.58 The hypothesis is that an excessive production and absorption of ammonia associated with intestinal overgrowth of ammonia-producing bacteria would overwhelm normal liver metabolism causing ammonia toxicity and the encephalopathic signs.
Veterinary aspects of training and racing endurance horses
Overview of the sport
History and evolution
Description of the sport
1 STAR
2 STAR
3 STAR
4 STAR
Distance
80–119 km in 1 day
120–139 km in 1 day
70 km and 89 km over two days
140–160 km in 1 day
90–100 km over 2 days
70–80 km over 3 days or more
160 km in 1 day
for Senior Chps
120–130 km in 1 day Junior and Young Rider Chps
Maximum heart rate at vet-gate
64 bpm within 20 minutes
Maximum heart rate at final inspection
64 bpm within 30 minutes
Horse age
at least 6 years
at least 6 years
at least 7 years
at least 8 years
Mandatory rest for horses
20 days
Veterinarians and officials for endurance events
Veterinary controls
Physiology of endurance exercise
Metabolism
Thermoregulation
Electrolyte losses
Acid–base disorders
Substrate depletion
Oxidative stress
Specific diseases
Prevalence
Prevention and risk factors
Metabolic conditions
Pathophysiology and prevalence
Exhausted horse syndrome (EHS)
Synchronous diaphragmatic flutter (SDF)
Exertional myopathy

Colic
Metabolic encephalopathy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterinary aspects of training and racing endurance horses
