Chapter 15
Vacuum-Assisted Wound Closure in Chelonians
Wound Management
The Vacuum-Assisted Closure (VAC) Therapy system (KCI, San Antonio, Tex) is a noninvasive wound management technique that uses negative pressure wound therapy (NPWT) to accelerate the healing process of difficult wounds.1 This relatively new technique has been proven successful in small and large mammals (including humans) and reptiles.1–10 Chelonians are excellent candidates for NPWT because of their unique shell, which allows easy bandage placement, and their tractable nature, as they are not prone to rolling and entangling the vacuum hose. Although this technique requires more equipment compared with traditional wound management, it is relatively simple to apply, and the speed and quality of healing in complicated cases more than outweigh the costs of extended hospitalization (weeks to months).
In chelonian medicine, VAC therapy is used to treat challenging wounds involving carapace and plastron defects and tissue exposure, most often caused by trauma and less frequently by thermal burns or infection. The therapy should be used in the early stages of treatment and can be followed with traditional therapy once wound healing is progressing well with a healthy granulation bed. VAC treatment time for shell injuries in land chelonians has been reported to be from 3 to 43 days, whereas in sea turtles, treatment is generally a few weeks to as long as a year or more, depending on the severity of the wound.8
The Theory of Vacuum-Assisted Closure Therapy
NPWT promotes wound healing in several ways: (1) promotes contraction of wound margins to facilitate closure, (2) encourages granulation tissue formation, (3) increases tissue perfusion, (4) removes exudate and (5) reduces edema.1–3 Reduction of edema that would otherwise accumulate in the wound increases perfusion and provides nutrients, inflammatory cells, oxygen, and growth factors while removing free radicals.1–3 Severe wounds to the carapace often lead to collapsing of the lung. NPWT has the added benefit of bringing lung tissue back into its original location, favoring a more normal anatomic orientation and preservation of the coelomic space. With NPWT, mechanical force is applied to a wound to promote healing. This is accomplished through two active principles: macrostrain and microstrain. Macrostrain is the visible deformation that occurs when negative pressure is exerted on the foam and it collapses. It is a visible, physical response that draws the wound edges closer together, evenly distributes negative pressure, and removes exudate and infectious material. Microstrain refers to microdeformation, which leads to cellular stretching. This biologic response occurs at the cellular level to promote perfusion, reduce edema, and promote the rapid formation of granulation tissue. Microstrain facilitates cell migration to the wound, enhancing immune function and increasing the rate of granulocyte cell division.11
Indications and Contraindications
In humans, indications for the use of VAC include acute to chronic, traumatic, and dehisced wounds, partial-thickness burns, ulcers, incisions, flaps and grafts, and diabetic wounds.3 New applications continue to be described, such as spider bite management, osteomyelitis, and exposed bones.12–14 In chelonians, the main indication for VAC therapy is the treatment of carapace and plastron defects with soft tissue exposure.
Incomplete wound debridement before starting NPWT may result in proliferation of granulation tissues over necrotic tissues and delayed wound healing.9 Negative pressure should not be used directly over exposed organs, blood vessels, or nerves. If these are present, closed cell foam should be used to protect exposed lungs or other organs. Hemostasis should be verified before application of negative pressure. It should not be used for neoplastic lesions or patients with a bleeding disorder.
Equipment Needed
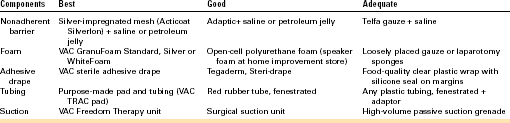
Basic VAC therapy relies on open-cell foam that is placed into the wound bed, covered by an airtight plastic dressing, and attached to a suction machine by plastic tubing (Figure 15-1). Additional materials such as tape and adhesives have proven useful for the chelonian patient when leaks are present after the initial VAC application and have been included in Table 15-1 (see also Case 15-1). Purpose-made equipment is commercially available at KCI Animal Health (San Antonio, Tex), and clinicians can order wound care kits that fit the needs of a specific patient. Because this treatment can become costly over time, economical alternatives to the VAC components are also included in this chapter.
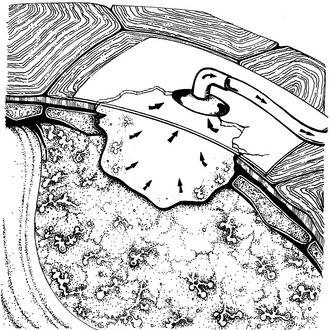
FIGURE 15-1 VAC therapy on a chelonian patient. The foam is placed into the defect and covered with a clear dressing. An egress tube is attached and linked to a suction unit (not shown). (Drawing courtesy Lori E. Hunt.)
Adhesive Drape
Several types of occlusive plastic adhesive films can be used and cut to fit. These include VAC adhesive drape (KCI), Steri-drape and Tegaderm (3M, St. Paul, Minn). For large wounds, several drapes may be required and overlapped to cover the foam. Once the vacuum has been applied, leaks may become apparent. Troubleshooting leaks (air or water) can be performed with a variety of techniques and products at the margins of the draped area, including the application of additional adhesive drape material, 100% silicone, or adhesive paste (Stomahesive paste, ConvaTec, Skillman, NJ) (Case 15-2). Bridge defects, especially the ones that connect to the skin from the foreleg or hindleg, can be challenging to drape. Immobilizing the hindleg (in flexion or extension) with gauze and tape can be very helpful in achieving a stable bandage seal.
Suction Pump
The purpose-made VAC Freedom suction pump is the apparatus of choice for this treatment. The advantages of the purpose-made pump include quiet operation, a smaller and more portable unit (some are battery operated), accurate pressure adjustment, and alarm system when the seal is breached. The unit can be either purchased or rented from the manufacturer for the duration of treatment. Continuous or intermittent suction settings are programmed. Intermittent suction has been associated with more rapid cellular division than continuous suction but may create patient discomfort. Therefore it is best to start with the continuous setting until the wound bed is well-developed. The intensity feature addresses how quickly pressure is achieved. Low intensity is recommended for patients new to therapy because the creation of pressure is slower. Higher intensity settings are recommended for larger wounds so that a more rapid seal is obtained. Alternatively, any surgical suction pump or passive suction grenade can be used to generate negative pressure.