Laura K. Tulloch, Justin D. Perkins
Update on Recurrent Laryngeal Neuropathy
Recurrent laryngeal neuropathy (RLN) is a common cause of upper respiratory tract obstruction and poor performance in equine athletes.
Pathology
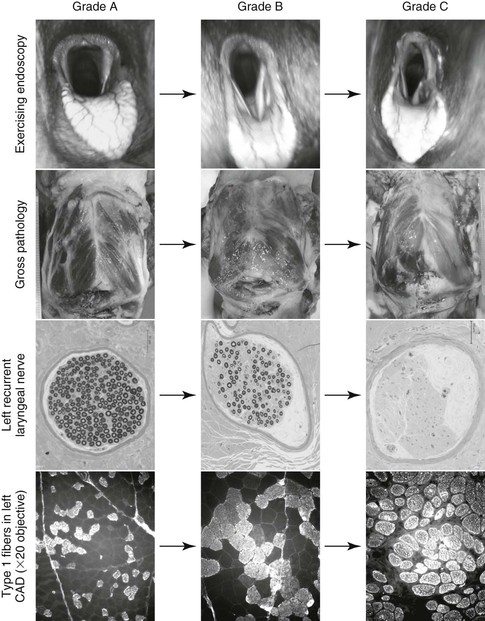
Recurrent laryngeal neuropathy is characterized by a bilateral distal axonopathy of the recurrent laryngeal nerves, resulting in a progressive loss of large myelinated fibers, with the left recurrent laryngeal nerve being more severely affected (Figure 52-1). These nerves are the longest in the body, with the left nerve looping around the aorta and the right turning around the subclavian artery within the thorax. The total length of the left recurrent laryngeal nerve is up to 250 cm in horses (>30 cm longer than the right recurrent laryngeal nerve). The recurrent laryngeal nerve is composed predominantly of medium-sized myelinated fibers. Changes that indicate an axonal lesion include collapsed myelin sheaths, an increase in the relative thickness of the myelin sheath, regenerating Schwann cell membrane clusters, and so-called onion bulb formations, all indicative of segmental demyelination and remyelination.
Damaged innervation results in neurogenic atrophy of intrinsic laryngeal muscle, histologically characterized by muscle fiber atrophy and hypertrophy, fiber type grouping, appearance of angular fibers, fewer type 1 muscle fibers and increased numbers of type 2 fibers, fibrosis, and fat replacement. Collateral axonal sprouting and reinnervation of previously denervated muscle (demonstrated by fiber type grouping) indicate that the muscle is attempting to repair. The cricoarytenoideus lateralis (CAL; laryngeal adductor) muscle is affected before the cricoarytenoideus dorsalis (CAD; laryngeal abductor) because there are more large myelinated fibers in the left adductor branch of the recurrent laryngeal nerve, making it more susceptible to the disease process. Although the adductor muscles are affected earlier and more severely than the CAD, it is the pathologic changes within the CAD that result in functionally relevant clinical signs because of the CAD muscle’s key role in increasing the size of the rima glottidis lumen during exercise (see Figure 52-1). Histopathologic changes consistent with RLN have also been described in clinically normal horses.
Etiology
The definitive etiology of RLN is not known, but both genetic and acquired causes are considered possible. Histologic changes associated with RLN have been identified in young foals, supporting a genetic influence, and some authors believe that RLN is inherited as a polygenic trait, since progeny of RLN-affected stallions are more likely to be affected with RLN than are progeny of unaffected stallions. A recent genome-wide association study (see Dupuis et al in Suggested Readings) of more than 500 horses revealed two large loci that appeared protective against RLN, although no disease-associated loci were identified. Acquired causes include jugular perivascular injection of irritating substances and lead poisoning.
Clinical Manifestation and Diagnosis
Horses with RLN are often identified by abnormal inspiratory noise during exercise and by poor performance. If the arytenoid cartilage cannot abduct properly, the cross-sectional area of the rima glottidis is reduced. Consequently, inspiratory airflow is obstructed, and an abnormal inspiratory noise is heard secondary to increased air turbulence. A horse with RLN hypoventilates during strenuous exercise, and the resultant lack of oxygen results in early exhaustion. Exercising horses with RLN are more hypoxemic, hypercapnic, and acidotic compared with unaffected horses. Atrophy of the left CAD muscle may also be detected during percutaneous laryngeal palpation.
Endoscopic examination of the larynx at rest and preferably during exercise (either on a treadmill or with a remote endoscope; see Chapter 51) confirms the diagnosis of RLN. During resting laryngeal endoscopic examination, the arytenoid cartilages and vocal cords must be observed with the horse unsedated. Diagnosis of severe RLN is usually straightforward, but identification of mildly affected horses is more challenging. Maximal abduction of the arytenoid cartilages can be induced by occluding the horse’s nares or by inducing swallowing, either by flushing a small volume of water into the pharynx through the endoscope or by touching the nasopharyngeal mucosa with the tip of the endoscope or guidewire. Inducing swallowing allows evaluation of both abduction and adduction of the arytenoid cartilages. At present, function of the left arytenoid cartilage is graded during resting endoscopy with a subjective seven-point system (Table 52-1). However, some clinicians use four- and five-point systems to grade laryngeal function at rest. Moderate daily intrahorse variability has been reported, and results of resting endoscopic examinations performed on a single occasion should be interpreted cautiously. Endoscopic examination during exercise uses a three-point system (Table 52-2) and enables identification of horses that have relatively normal laryngeal function at rest but develop arytenoid collapse during strenuous exercise (Table 52-3).
TABLE 52-1
Havemeyer Endoscopic Laryngeal Grading System*
| Grade | Description | Subgrade |
| I | All arytenoid cartilage movements are synchronous and symmetric, and full arytenoid cartilage abduction can be achieved and maintained. | No subgrades. |
| II | Arytenoid cartilage movements are asynchronous and/or asymmetric at times, but full arytenoid cartilage abduction can be achieved and maintained. | |
| III | Arytenoid cartilage movements are asynchronous and/or asymmetric. Full arytenoid cartilage abduction cannot be achieved and maintained. | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|