Samuel D.A. Hurcombe
Internal Hemorrhage and Resuscitation
Internal hemorrhage in horses is an uncommon but important clinical condition. It may occur in the abdomen (peritoneal space), thorax (pleural space, mediastinum), tissue and fascial planes, or central nervous system. The clinician should be able to identify the source of hemorrhage and the steps needed to potentially stop it, and this is facilitated by understanding the concept and practice of hypotensive resuscitation and how and when to transfuse whole blood. Internal hemorrhage is most commonly encountered as a result of trauma or surgery but may be caused by coagulopathy, rupture of a tumor, or phenylephrine administration in older horses.
Traumatic internal hemorrhage may be the result of external trauma to the abdominal wall, such as a kick from another horse or high-speed impact (racing injury), wherein much of the impact and force are received by internal organs such as the spleen, kidney, and liver. These parenchymal organs receive in total upward of 40% of cardiac output in the resting animal, and if injured can bleed extensively into the peritoneal and retroperitoneal spaces. Reproductive trauma and periparturient hemorrhage are of notable importance in mares, in which rupture of the middle uterine artery within the broad ligament (mesometrium) can occur in the prepartum period, in the postpartum period, or during delivery.
In the hospital setting, postoperative hemorrhage may follow abdominal surgery, particularly if intestinal resection and anastomosis of bowel have been performed or when a tumor or other mass has been removed.
Regardless of the cause, the extent of internal hemorrhage can be difficult to recognize because, unlike with external hemorrhage, the clinician cannot calculate actual blood losses. The latter must be estimated on the basis of signs of hypovolemia and hemorrhagic shock. Treatment of internal hemorrhage also is difficult, because arrest of bleeding by primary ligation of a ruptured or torn vessel is usually impossible: either the vessel is anatomically inaccessible or it is impossible to see among the blood and damaged tissue. In general, surgical intervention is not recommended. Moreover, even if surgical intervention were indicated, adequate stabilization of the hemorrhaging patient to withstand anesthesia would be challenging. Another concern during treatment may be the dislodging of an immature blood clot when blood pressure rises as a consequence of aggressive fluid therapy to increase perfusion and tissue oxygenation. Rapid increases in intravascular volume within the vasoconstricted vascular bed can result in hypertension, which may restart the bleeding.
Recognition of Internal Hemorrhage and Estimation of Blood Loss
By estimating the magnitude of blood loss, the need for blood transfusion and its urgency and the transfusion volume needed can be determined. In humans, the advanced trauma life support (ATLS) classification scheme is used to estimate the percentage of blood loss in a patient with hypovolemic hemorrhagic shock (Table 3-1). Although specific guidelines are not available for horses, blood loss may be estimated from clinical and clinicopathologic findings. Horses with mild (<15% blood loss; ATLS class I) internal hemorrhage may be clinically normal or have only minor derangements in physiologic parameters. These patients do not require transfusion therapy, but rather need close monitoring and frequent reassessment to ensure that they remain stable and that the degree of hemorrhage has not worsened. Horses with mild to moderate (15% to 30%; ATLS class II) blood loss are likely to show signs of compensated hypovolemic shock. Tachycardia, agitation or restlessness, tachypnea, mild colic, and pale pink mucous membranes with a capillary refill time of greater than 2 seconds may be seen. Clinicopathologic indicators of hemorrhage may reflect mild problems with oxygen delivery; for example, the blood L-lactate concentration may be mildly increased. Packed cell volume (PCV) and total protein (TP) concentration may be normal initially, until the decrease in capillary pressure leads to interstitial fluid recruitment, which dilutes the remaining circulating erythrocytes and proteins. This is typically evident by 24 hours after hemorrhage. These patients may benefit from transfusion; however, if the hemorrhage has stopped and physiologic indicators are stable, blood transfusion may not be necessary, and the horse may respond well to fluid volume and blood pressure support alone.
TABLE 3-1
Advanced Trauma Life Support Classification Scheme: Criteria for Estimating Blood Loss in Humans
| Class | Pulse Rate (per min) | Blood Pressure | Central Nervous System Status | Urine Output | Estimation of Blood Loss |
| I | <100 (horse <40)* | Normal | Mild anxiety | Normal | <15% |
| II | >100 (horse 40-60)* | Normal | Anxious, agitated | Decreased | 15%-30% |
| III | >120 (horse 60-80)* | Decreased | Confused, delirium | Minimal | 30%-40% |
| IV | >140 (horse >80)* | Decreased Pulse pressure undetectable | Obtunded, comatose | None | >40% |
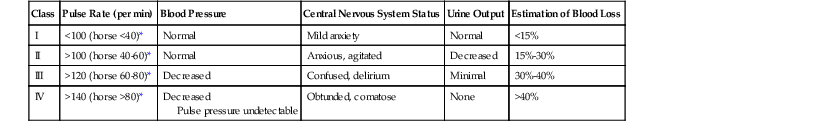
* Suggested modified heart rate responses in horses with hemorrhage.
Horses with moderate to severe (30% to 40%; ATLS class III) blood loss show signs of decompensated hypovolemic shock. Physiologic derangements all attributable to activation of the sympathoadrenal systems are clinically evident and reflect global oxygen and perfusion debt. Moderate tachycardia, tachypnea, flared nostrils, pale mucous membranes, and moderate agitation to somnolence may be observed, along with colic-like behavior, sweating, shaking, and ataxia. Intraabdominal hemorrhage may distend the abdominal contour, whereas respiratory distress and rapid shallow breathing may be striking features of pleural hemorrhage. The PCV may not be dramatically decreased, but the TP is likely to be decreased; however, in the acute setting, interstitial fluid redistribution is unlikely to have occurred to a sufficient degree to reflect the true decrease in circulating erythrocyte mass. Blood L-lactate concentration will be increased, even in the face of crystalloid administration. These patients need immediate transfusion therapy.
Horses with severe (>40%; ATLS class IV) blood loss are at high risk for death, even with aggressive volume and transfusion therapy. Heart rate is extremely fast, but may actually decrease in extremis. Neurologic deterioration is a prominent feature of these horses; obtundation, coma, slow or absent papillary light responses with pupillary dilation, recumbency, seizure, and abnormal breathing patterns may be observed. Diarrhea has also been observed in horses with severe hemorrhage and likely reflects an acute global hypoxic insult to the intestine. The PCV and TP are low, and blood L-lactate concentration is markedly high as a result of global hypoperfusion and hypoxia. These patients will die without treatment, and many will not respond or recover even with aggressive transfusion therapy.



