Chapter 171 Tumor Lysis Syndrome
• Tumor lysis syndrome (TLS) is a rare but potentially fatal constellation of metabolic abnormalities in veterinary oncology patients.
• TLS is seen most commonly in patients with chemotherapy-responsive or radiation-responsive diseases, such as lymphoma or lymphoid leukemias, hours to a few days after treatment. Patients at highest risk include those with dehydration or advanced disease and with rapid induction of remission with treatment.
• The metabolic complications of TLS are due to rapid tumor cell death and are characterized by hyperphosphatemia, hyperkalemia, metabolic acidosis, and hypocalcemia, with or without azotemia. These metabolic abnormalities may be further exacerbated in patients with renal dysfunction.
• Clinical signs of TLS can include depression, vomiting or diarrhea, or both (many times hemorrhagic), bradycardia, and cardiovascular collapse culminating in shock.
• Rapid diagnosis and therapy for TLS is essential because mortality rates are high. Treatment for TLS is: (1) aggressive fluid therapy, (2) correction of acid-base and electrolyte abnormalities, and (3) discontinuation of chemotherapy or radiation until the patient is normal clinically and biochemical parameters are within normal limits.
PATHOGENESIS AND METABOLIC COMPLICATIONS
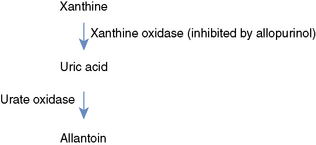
Acute renal failure is a common sequela of TLS and the pathophysiology is likely multifactorial.9 Not only do hyperphosphatemia and hyperuricemia result from TLS, they also contribute to the oliguric acute renal failure in these patients. Causes may include tubular precipitation of calcium phosphate and nucleic acid metabolites (and secondary intraluminal tubular obstruction), intravascular volume depletion, and poorly understood malignancy-associated nephrotoxins. A diagram of the purine metabolism pathway is shown in Figure 171-1 and is discussed further in the Treatment section.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree