Chapter 13 Toxicological disorders
Introduction
Illustrations of toxicological disorders in cattle present problems. The clinical signs may be transient, with death occurring within a few minutes, such as in yew (Taxus baccata) poisoning (p. 249). In many cases the signs may be nonspecific. Where the effects are confined largely to one system, the description has been given in the appropriate section, e.g., ergot and fescue foot are considered under locomotor disorders (7.158–7.160). In this chapter, toxicoses have been broadly grouped into plant, organic, and inorganic chemical sections, and a few examples are given of each group. They are taken from Brazil, China, Germany, New Zealand, South Africa, the UK, the USA, and Zimbabwe.
Plant toxicoses
Bracken (bracken fern)
Clinical features
bracken toxicosis is widespread in several continents. Bracken (Pteridium aquilinum) contains ptaquilosides and other compounds which act as a cumulative poison in two syndromes. Firstly, after ingesting large quantities for a few weeks, cattle may show an acute syndrome resulting from aplastic anemia and thrombocytopenia. Sudden death is occasionally seen. In 13.1 the vulva of the crossbred Angus cow is pale from severe anemia. The pinpoint hemorrhages result from thrombocytopenia. Hemorrhages elsewhere can cause epistaxis, hyphema (13.2) (bleeding into the anterior chamber), or hematuria from bladder mucosal hemorrhage (13.3).
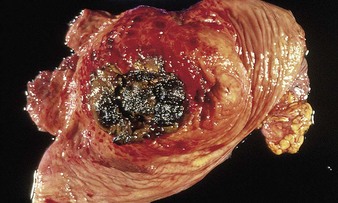
Secondly, long-term ingestion of considerable quantities of bracken for several months can lead to a chronic syndrome of enzootic hematuria. The ptaquilosides are carcinogens and cause bladder neoplasia, resulting in enzootic hematuria and malignancies such as hemangiosarcoma (13.4). Numerous discrete masses, seen protruding from the mucosal surface, bleed readily as the bladder distends and contracts. Some mucosal areas (top right, lower left) appear normal. The hemangiomata can develop into ulcerating tumors of various types. Alimentary tract neoplasms include squamous cell carcinomas and papillomas affecting the pharynx and esophagus, respectively. 13.5 shows pharyngeal squamous cell carcinomas (A) and esophageal papillomas (B) identified in Brazil. Bovine papillomavirus (types 2 and 4) may also be involved in upper alimentary neoplasms.
Differential diagnosis
acute syndrome: anthrax (12.63), septicemic pasteurellosis (5.10), PPH syndrome (9.39), mycotoxicosis (p. 253); chronic cases: pyelonephritis (10.1, 10.2), cystitis, babesiosis (12.41).
Oak (acorn)
Clinical features
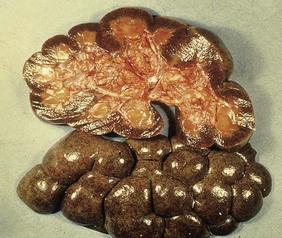
the toxic principle causes renal and gastrointestinal changes. The signs include abdominal pain, often with a hemorrhagic diarrhea, thirst, polyuria, and ventral edema as a result of subacute and chronic toxicity. The esophageal mucosa can be hemorrhagic (13.6). The enlarged, swollen kidneys (13.7) show scattered hemorrhages and a nephrosis, which accounts for the ventral edema, ascites, and hydrothorax seen in cases with renal failure.
Yew
Clinical features
signs usually follow acute exposure and include nervousness, ataxia, dyspnea, and collapse. The opened rumen in 13.8 shows normal ingesta mixed with needle-like yew leaves. Cattle usually die minutes after ingesting a few mouthfuls of yew twigs or berries, typically encountered as fresh or dried clippings thrown over a graveyard hedge into a bare winter pasture. The lethal dose in adult cattle may be as little as 1 kg of leaves. Some cattle may survive up to 3 days before they die.
Ragwort (seneciosis)
Clinical features
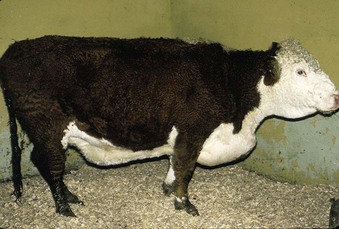
early signs include dark-colored diarrhea, photosensitization, jaundice, abdominal pain, and central nervous system abnormalities. Prolonged ingestion (chronic exposure) results in progressive weakness, weight loss, and liver failure due to cirrhosis, and severe lung disease. In the mature Hereford cow in 13.9, the resulting right heart failure led to the edema affecting the ventral body wall, brisket, and head. Clinical signs may not be seen until several months after digestion, by which time the animal is no longer consuming the toxin, and diagnosis can be difficult. Liver biopsy may be useful for diagnosis. The fresh plant is bitter and usually avoided. Intoxication frequently occurs following its incorporation into conserved forage as this renders the plant more palatable. See also photosensitization (p. 30).
Differential diagnosis
mycotoxicosis (p. 253), lead poisoning (13.29), and other causes of hepatic disease and encephalopathy.
Rape and kale
Clinical features
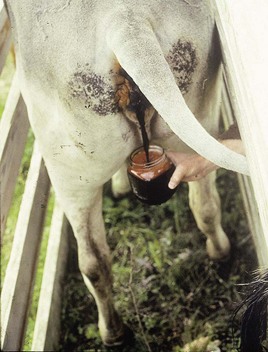
cattle develop hemoglobinuria, voiding dark-red urine (13.10), and are anemic and weak. Autopsy of fatal cases reveals pallor and jaundice of the liver (13.11) and heart (13.12).
Differential diagnosis
postparturient hemoglobinuria (possibly related to SMCO via a cumulative effect in red cells), bacillary hemoglobinuria, nitrate/nitrite poisoning (13.27, 13.28), hypomagnesemia (9.5), babesiosis (12.39–12.43), anaplasmosis (12.44–12.47), acute bracken poisoning (13.1–13.3), chronic copper poisoning (13.33).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree