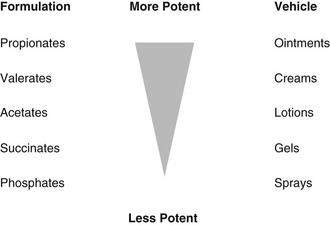
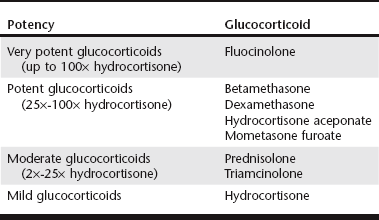
Chapter 109 Drugs of the glucocorticoid class work by reducing pruritus, pain, swelling, exudation, tissue proliferation, and stenosis. In addition, glucocorticoids (particularly dexamethasone) appear to reverse the ototoxicity associated with Pseudomonas infections (Takeuchi and Anniko, 2000). The clinical decision is not whether to use glucocorticoids, but how their use should be combined with ear cleaning and antimicrobial therapy to ensure a successful outcome (see Chapters 110, 111, and 113). Long-term maintenance therapy with glucocorticoids is often required to prevent recurrence in animals with underlying conditions such as atopic dermatitis. The choice between topical and systemic glucocorticoids depends largely on the severity of the otitis. It is important carefully to assess the degree of pain, firmness, mobility, erythema, swelling, fibrosis, hyperplasia, and stenosis of the ear canals by palpation and otoscopy (see Chapter 108). Topical therapy is preferred because it delivers the drug to the affected site, avoiding systemic exposure. The ear canal is a self-contained unit ideally suited to topical treatment, and most polyvalent ear products contain a glucocorticoid. Systemic treatment is necessary if the ear canals are stenosed, if there is severe fibrosis or hyperplasia, if topical therapy cannot be administered safely, and/or with some cases of otitis media. Once the ear canals have opened it is usually possible to switch to topical therapy. Animals may also tolerate topical therapy better once the pain and inflammation have decreased. The antiinflammatory potency of topical glucocorticoids varies widely (Table 109-1 and Figure 109-1). Lotions and gels are easier and less messy to apply and dry quickly, leaving fewer residues. Oils, creams, and ointments may moisten and soothe dry and inflamed skin but can be occlusive and are contraindicated for use in exudative or seborrheic ears. TABLE 109-1 Relative Potency of Topical Glucocorticoids Commonly Used in Veterinary Medicine This table should be used for guidance only, because the relative potency of topical glucocorticoids also can vary with the concentration, formulation, and preparation (see Figure 109-1). For example, in human dermatology, for the same steroid, occlusive preparations (e.g., ointments, creams) and certain esters (e.g., propionates and valerates) are more potent. Products should be applied once or twice daily until remission occurs; efficacy may be greater with more frequent administration, but compliance with treatment may be lower. Once the otitis has resolved, topical glucocorticoids should be used at the lowest frequency that controls the inflammation or discontinued if possible. When continued use is required, data on owner compliance from studies of atopic dermatitis and recurrent pyoderma suggest that a regimen of treatment on 2 or 3 consecutive days each week (i.e., “weekend therapy”) is better adhered to than therapy every other day or twice weekly (Carlotti et al, 2004; Martins et al, 2012).
Topical and Systemic Glucocorticoids for Otitis
Why Use Glucocorticoids for Otitis?
Should Topical or Systemic Glucocorticoids Be Used?
Which Topical Glucocorticoids Should Be Used?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree