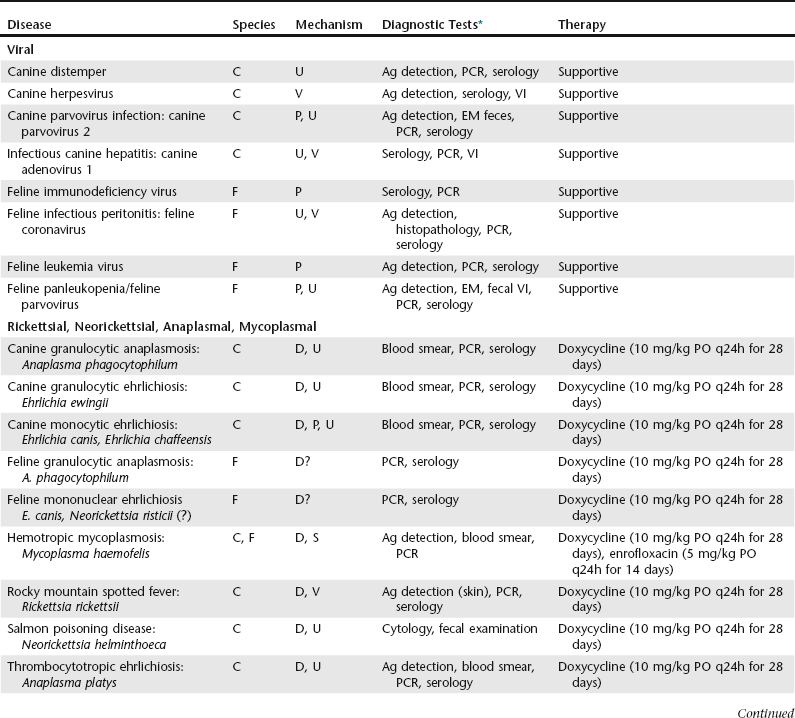
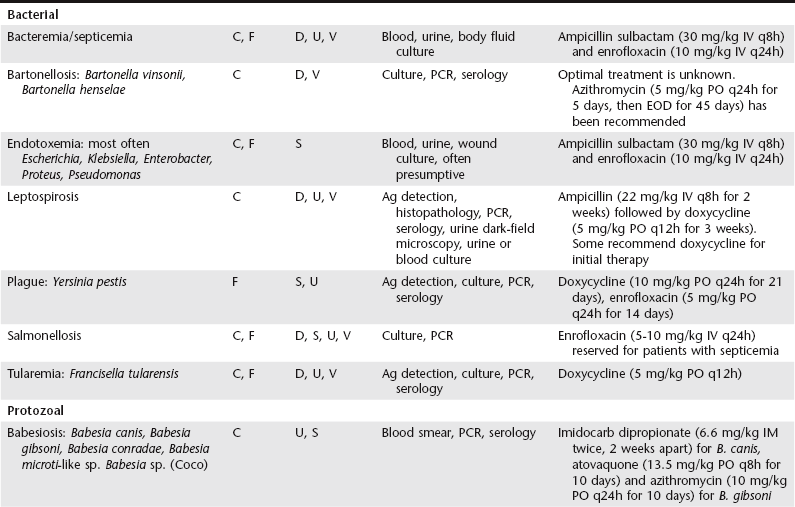
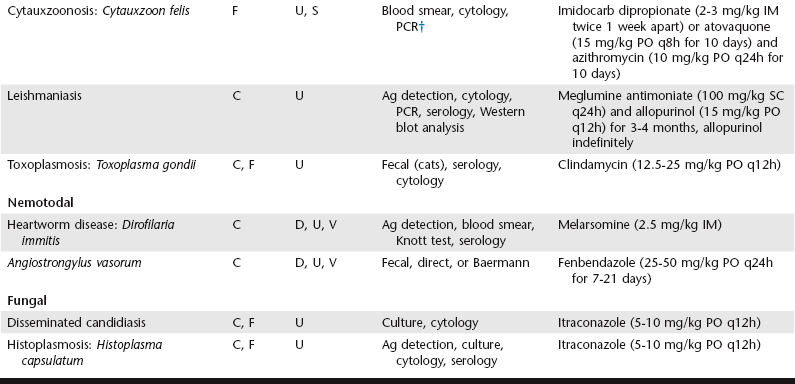
Chapter 61 Thrombocytopenia is the most common platelet disorder observed in dogs and cats. Of dogs and cats presenting to the authors’ institution from 2006 to 2012, thrombocytopenia was found in 17.6% of dogs and 12% of cats, with 6.2% of dogs and 4.8% of cats having counts of less than 100,000 platelets/µl. Previous studies at this university have shown that in dogs the etiology of thrombocytopenia is 5% primary immune mediated, 13% neoplasia, 23% infectious or inflammatory disease, and 59% miscellaneous or multifactorial causes (Grindem et al, 1991). In cats causes of thrombocytopenia included 2% primary immune mediated, 20% neoplasia, 29% infectious diseases, 7% cardiac diseases, 22% multiple etiologies, and 20% unknown causes (Jordan, Grindem, and Breitschwerdt, 1993). Pseudothrombocytopenia occurs when platelets present in a specimen are not counted. This must be eliminated as the cause of a low platelet count. Platelet aggregation that results from activation during blood sampling is a major cause of falsely decreased counts and occurs commonly in cats; one study found low automated platelet counts in 71% of feline samples (Norman et al, 2001). Large platelets are also a cause of low platelet counts on some automated impedance-based hematology analyzers when they overlap with the size of red blood cells (RBCs). Ethylenediaminetetraacetic acid (EDTA)–induced platelet clumping has rarely been reported. Some breeds such as cavalier King Charles spaniels and greyhounds normally have lower platelet counts than most dogs or established platelet reference intervals. Immune-mediated thrombocytopenia (IMTP) can be primary, secondary, vaccine induced, or posttransfusion. Primary, or idiopathic, IMTP is reported most commonly in dogs but has also been reported in cats. This is a disease of exclusion; other potential causes of secondary IMTP must be eliminated before a diagnosis of primary IMTP can be made. Acquired amegakaryocytic thrombocytopenia is a rare form of either primary or secondary immune-mediated disease resulting from autoantibodies directed toward megakaryocytes and has been reported in both dogs and cats (Thomas, 2010). Secondary IMTP occurs when antibody targets nonself antigens adsorbed onto the surface of platelets or when immune complexes become bound to platelet surfaces. Underlying mechanisms include systemic autoimmune diseases (systemic lupus erythematosus), neoplasia, infectious agents, and drugs; occasionally, however, additional causes are identified or suspected, such as pemphigus, juvenile-onset polyarthritis syndrome in Akitas, and possibly canine inflammatory bowel disease (Scott and Jutkowitz, 2010). Thrombocytopenia associated with neoplasia is often multifactorial, with secondary immune-mediated destruction representing one potential component. Lymphoma in dogs has been associated most commonly with secondary IMTP, but it can occur with any neoplasm. In one study 10% of dogs with neoplasia had concurrent thrombocytopenia, and of this group 61% did not have identifiable factors known to cause secondary IMTP (Grindem et al, 1994). As with neoplasia, thrombocytopenia in infectious diseases is often multifactorial and can include a secondary immune-mediated component. Antiplatelet antibodies have been detected in various infectious diseases, including Ehrlichia canis infections and Rocky Mountain spotted fever (RMSF). Drugs are rarely reported to cause a true primary IMTP; more typically it is secondary in nature. With this mechanism the drug acts as a hapten, allowing immune-mediated targeting of the platelets. A few drugs are capable of causing a secondary immune-mediated reaction without a history of prior exposure (e.g., heparin in horses), but most occur following extended use or prior exposure. Several documented cases involving trimethoprim sulfonamide/sulfamethoxazole have been reported in dogs, but it could potentially be caused by any number of drugs. Vaccine-induced thrombocytopenia has been reported in dogs following immunization with modified live vaccines (canine distemper). Typically thrombocytopenia is mild and develops within 3 to 10 days after vaccination, but marked thrombocytopenia can occur. Posttransfusional thrombocytopenia has been reported occasionally in dogs. Table 61-1 lists infectious agents associated with thrombocytopenia in dogs and cats (Greene, 2012). Thrombocytopenia associated with infectious causes is often multifactorial, involving increased consumption, destruction, vasculitis, or sequestration; in many cases the pathogenesis is incompletely understood. As mentioned previously, a number of agents are associated with secondary IMTP. Some are known to cause bone marrow suppression, including feline leukemia virus (FeLV) infection, feline immunodeficiency virus (FIV) infection, feline panleukopenia (parvovirus), canine parvovirus, and chronic monocytic ehrlichiosis (E. canis, Ehrlichia chaffeensis). FeLV and FIV are of particular importance in feline thrombocytopenia. Viral diseases (FeLV, FIV, and feline infectious peritonitis [FIP]) are a major cause of or contributing factor to the development of thrombocytopenia in cats (Jordan, Grindem, and Breitschwerdt, 1993; Thomas, 2010). TABLE 61-1 Infectious Causes of Thrombocytopenia in Dogs and Cats *Refer to Greene CE: Infectious diseases of the dog and cat, ed 4, for more information on diagnostic tests, available test kits, specimens, and commercial diagnostic laboratories. †Available at the North Carolina State University, Tick-Borne Disease Laboratory, Raleigh, NC. The degree of thrombocytopenia can vary. Although thrombocytopenia is most severe in IMTP and overwhelming sepsis (counts of less than 50,000/µl and often fewer than 10,000/µl), it can be moderate to severe in canine monocytic ehrlichiosis. In one report on prevalence of E. canis infection in thrombocytopenic dogs in an endemic region, infection was found in 63.1% of dogs with a platelet count of less than 100,000/µl but in only 21% of dogs with platelet counts between 100,000 and 200,000/µl; nonthrombocytopenic dogs had an infection rate of 1.4% (Bulla et al, 2004). Severe, cyclic thrombocytopenia is also seen with thrombocytotropic ehrlichiosis, but dogs are not systemically sick; clinically ill dogs with this disease should be evaluated for concurrent tick-borne diseases such as monocytic ehrlichiosis. Tests used to diagnose infectious diseases include serology, polymerase chain reaction (PCR), antigen detection in fluids or tissues, cytology, blood smear evaluation, culture, virus isolation, electron microscopy, and histopathology (see Table 61-1; Greene, 2012).
Thrombocytopenia
Immune-Mediated Thrombocytopenia
Infectious Etiologies Associated with Thrombocytopenia
Thrombocytopenia
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


