Chapter 46The Stifle
Imaging Considerations
Radiography
Scintigraphy
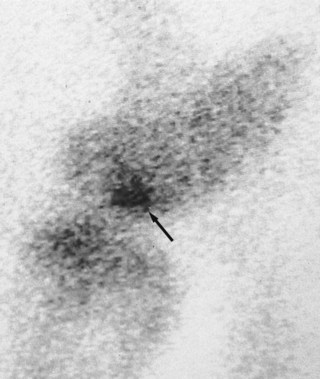
Nuclear scintigraphy is most consistently valuable in diagnosing incomplete avulsion fractures associated with the stifle.22,23 However, although positive results may be obtained within 24 hours of injury, in some horses at least 3 days must elapse before clinically significant increased radiopharmaceutical uptake (IRU) occurs. Subchondral cystic lesions that cause lameness may be scintigraphically positive or negative (Figure 46-1). The lesions are more likely to be detected in older horses, using a caudal image, than in an immature horse with high background activity. Absence of radiopharmaceutical uptake was thought to be the result of osteoclasts being the dominant cells in certain stages of the condition.24,25 However, in the Editors’ experience the majority of subchondral cystic lesions do have focal IRU. Although scintigraphy has been used to assess osteochondrosis in people,26 bone scan findings are not well documented in horses. I have seen positive and negative scintigraphic results associated with clinically significant osteochondrosis of the lateral femoral trochlea. Soft tissue injuries of the stifle are often scintigraphically negative, but in my experience IRU can occasionally be encountered in these horses, especially in association with enthesopathy.
Articular Diseases
Femoropatellar Joint
Osteochondrosis
Signs and Diagnosis
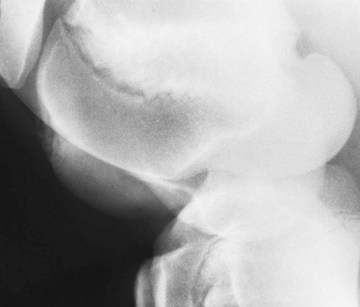
Radiological changes include the following: no detectable signs, slight loss of contour or loss of outline of the lateral trochlear ridge, irregular defects in the trochlear ridge, radiodense fragments within the defect (Figure 46-2), round radiopaque bodies loose in the joint, and more rarely, irregularities on the patellar apex or the medial trochlear ridge.1,32,33 Lateromedial and caudolateral-craniomedial oblique images are the most useful projections. Horses with radiological lesions do not always show lameness.25,27 Some horses have no detectable radiological abnormalities, but osteochondrosis lesions are diagnosed on arthroscopic examination. Lesions without fragmentation in young foals may resolve with time,32,33 but many progress.34
 years of age. The tibial apophyseal-epiphyseal physis closes by 1 year of age. The apophysis does not fuse with the metaphysis until 3 years of age. This apophysis is an important radiological feature in a young horse and can be mistaken for a fracture. The distal femoral physis closes by about
years of age. The tibial apophyseal-epiphyseal physis closes by 1 year of age. The apophysis does not fuse with the metaphysis until 3 years of age. This apophysis is an important radiological feature in a young horse and can be mistaken for a fracture. The distal femoral physis closes by about  years of age. In young foals, the margins of the femoral trochleas and the patella are irregular for the first 3 months of life because of incomplete ossification. The fibula is not evident radiologically until about 2 months of age, and a high percentage of adult horses have one and occasionally up to three horizontal radiolucent lines in the fibula distal to its head. These should not be confused with fracture lines.1
years of age. In young foals, the margins of the femoral trochleas and the patella are irregular for the first 3 months of life because of incomplete ossification. The fibula is not evident radiologically until about 2 months of age, and a high percentage of adult horses have one and occasionally up to three horizontal radiolucent lines in the fibula distal to its head. These should not be confused with fracture lines.1