Chapter 96Shock Wave Therapy
Shock Wave Generators
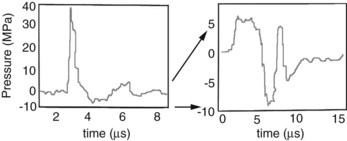
Two distinctly different pressure waves have been loosely described as SWT, SWs and radial pressure waves (RPWs). True SWs are pressure waves that meet specific physical parameters, including a rapid rise time (within nanoseconds), high peak pressures, and a gradual decrease in pressure over a few milliseconds, often with a negative pressure component (Figure 96-1 and Table 96-1).5 SWs occur naturally associated with lightning, planes breaking the sound barrier, or explosions. Electricity is used as a driving energy source to generate SWs used for medical purposes. RPWs are generated by pneumatically powered sources that drive a metal rod to strike a plate in contact with the skin surface. RPWs have slower rise times and lower peak pressures than SWs. Differences between SWs and RPWs are important because they may not affect tissue similarly; consequently, the type and equipment used are critical when evaluating the effect on tissues and efficacy of treatment. Editors’ note: However, published results in the horse have to date shown little difference in efficacy. A comprehensive review of SWs and RPWs, along with a description of equipment currently available, was recently published.6
TABLE 96-1 Comparison of Shock Waves and Radial Pressure Waves
| SHOCK WAVES | RADIAL PRESSURE WAVES | |
|---|---|---|
 | ||
| Rise time | 5-10 ns | 50 µs |
| Focusing | Yes | No* |
| Maximum pressure location | At focal point | On surface |
| Energy loss | Minimal through fluid/tissue | Loss proportional to the square of the distance |
| Peak pressure | ≈100 MPa | ≈10 MPa |
| Energy flux density | 0-3 mJ/mm2 | 0-0.3 mJ/mm2 |
* Includes “focused” end piece.
Reprinted with permission from Robinson EN, Sprayberry KA: Current therapy in equine medicine, ed 6, St. Louis, 2009, Saunders.




