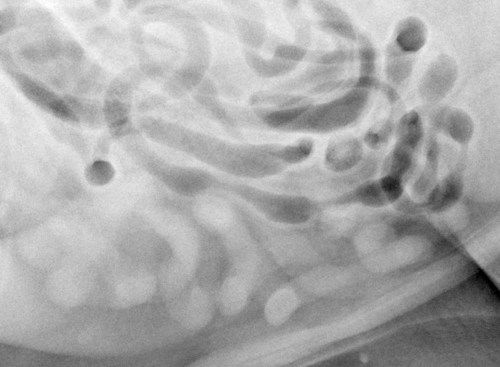
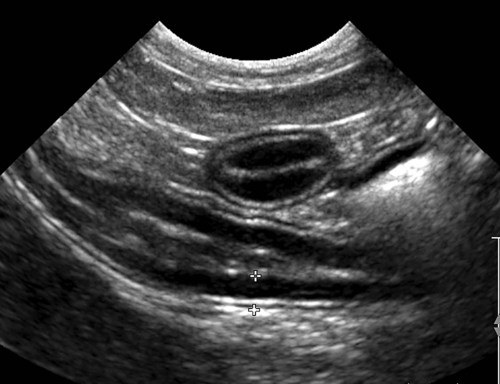
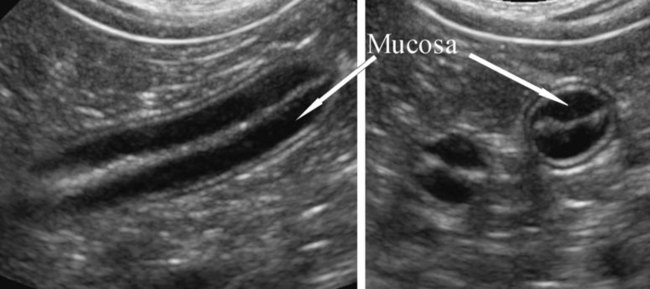
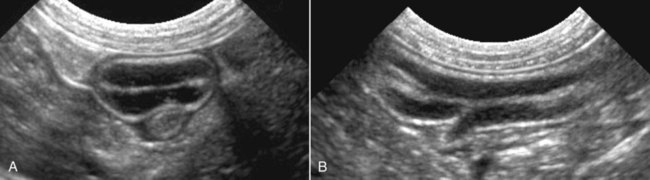
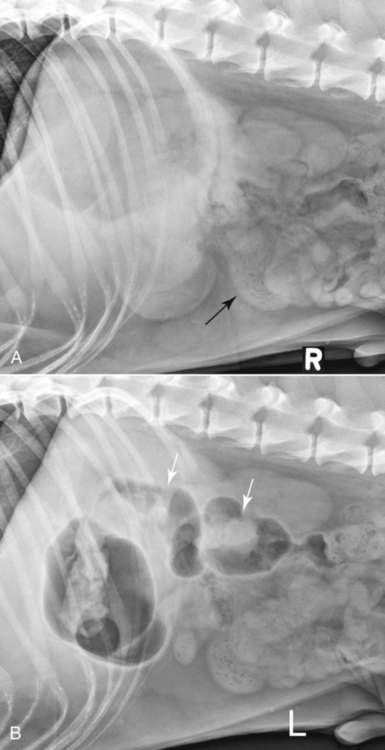
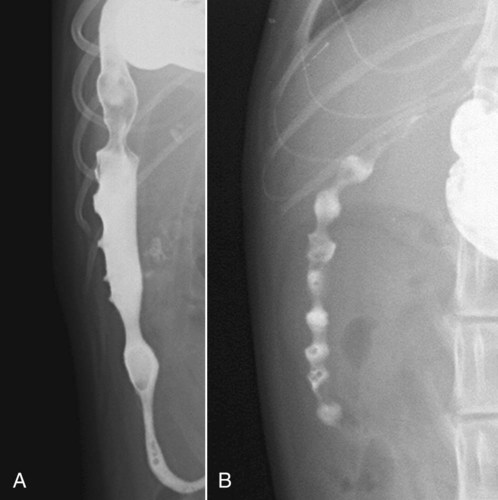
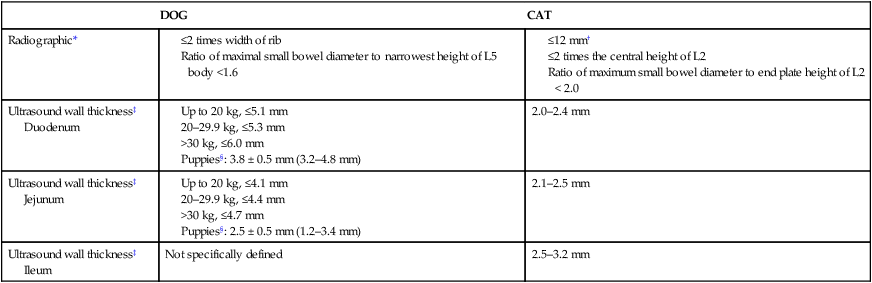
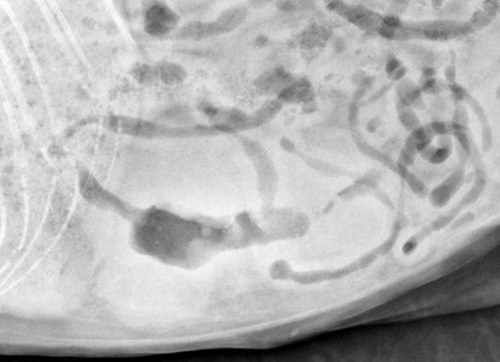
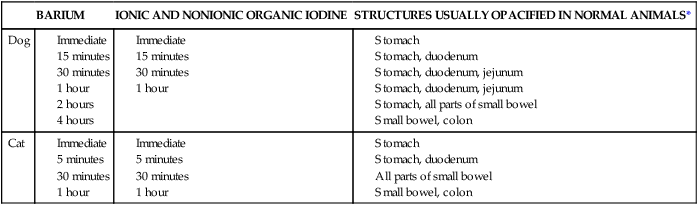
The standard views used to evaluate the small bowel are the recumbent left-to-right lateral and ventrodorsal (VD) views. As discussed in Chapter 35, there is rationale for obtaining left-right and right-left lateral views, in addition to the VD view, as standard in every patient.1 Briefly, obtaining both lateral views takes advantage of repositioning of intraluminal gas to change the conspicuity of various bowel segments, leading to a more complete examination. Other views, such as compressions radiographs, may also be useful.2 Withholding food for 24 hours and administering a cleansing enema 2 to 4 hours before radiography will optimize radiographic interpretation, but daily routine usually prohibits this extent of preparation. For the patient with acute abdominal pain; acute persistent vomiting; or palpable, enlarged fluid- or gas-filled bowel, no preparation is needed, and in fact, the native pattern of gas and fluid can be helpful diagnostically, and this valuable information may be altered by an enema. The roentgen sign assessment for the small intestine is summarized in Box 44-1. Abnormal margination, size, position, shape, and radiopacity can be assessed by survey radiographs, but mucosal irregularities and abnormal peristalsis or transit time must be determined from ultrasound or contrast studies. A moderate amount of intraperitoneal fat provides good contrast for definition of the intestinal serosal surfaces (Fig. 44-1). Animals younger than 6 months or emaciated animals have poor serosal definition because of a lack of intraabdominal fat for contrast.3 Serosal surfaces should be smooth and are seen most easily in regions where superimposition of bowel is minimal. A false interpretation of decreased serosal definition often results when the small bowel loops are overlapping in the central abdomen, when loops are crowded together by an abdominal mass, or when little or no gas is present in the bowel lumen (Fig. 44-2, A). These effects should not be misinterpreted as abdominal effusion. If gas is present in the stomach, a left lateral view may redistribute the gas into the bowel and confirm that the effect was simply lack of bowel lumen contrast (Fig. 44-2, B). Because of the variation in canine body size and the magnification effects of radiography, no accurate, specific measurement for normal diameter of the small bowel exists. Table 44-1 summarizes the schemes for relative bowel diameter that use nearby bones as reference structures. The maximal normal diameter (serosa to serosa) for the dog has been reported to be less than twice the width of a rib,4 or less than 1.6 times the height of the L5 vertebral body at its narrowest point.5 Because most cats tend to have a similar body size, a more specific definition of normal bowel diameter has been stated as not exceeding a 12 mm diameter when gas filled,6 or twice the height of the central portion of the L4 vertebral body.7 Cats without intestinal disease had a maximum small intestinal diameter to L2 vertebral endplate height ratio of 2.0 or less when compared with cats with gastrointestinal disease.8 For measurements and calculated ratios to be most accurate, optimally positioned radiographs and positive identification that it is the small bowel being measured needs to be ensured. Although the duodenum may be slightly wider, the jejunum and ileum should have approximately the same diameter.9 In reality, as a clinician gains experience in evaluating abdominal radiographs, qualitative assessment of bowel size will become just as accurate as measurement techniques. Table • 44-1 Small Bowel Normal Measurements †Mucosa to mucosa based on gas or barium filled. Attempts to judge the thickness of the intestinal wall on survey radiographs are unreliable. An empty bowel loop with a small volume of intraluminal air should not be mistaken for a pathologically thickened segment. However, there will be patients in which the bowel wall is unquestionably too thick (Fig. 44-3). In most instances, true thickening of the intestinal wall is better judged by ultrasound, contrast study, or palpation than by radiography. The normal small bowel is recognized in survey radiographs as smooth, continuously curving tubes or as solid circles or rings (see Fig. 44-1). These shapes are produced by the contractile activity of the smooth muscle. Segmental contractions give rise to spherical shapes, whereas peristaltic contractions cause long tubular shapes. The radiopacity of the normal small intestine is variable because of differing opacities of material within the lumen. In a nonfasted animal, any of the following may be seen in the lumen: air; grainy-appearing mottled ingesta, which may include mineral or metal; or fluid of homogeneous soft tissue opacity. The nondiscretionary eating habits of some dogs and cats may result in mineral or metallic opacities of small size being present in the small bowel. Clay-based cat litter and small gravel from dog runs are common examples. Gastrointestinal medications that contain calcium, magnesium, aluminum, bismuth, or silicate can impart significant radiopacity to the intestinal content.10 Some pet vitamin and mineral supplements contain sufficient mineral to be visible radiographically. In general, tablets or capsules containing minerals, either as active ingredients or in the coating, are more likely to be visible than liquids containing these minerals.10 In a fasted animal, the lumen may contain a small amount of ingested air, or it may be of homogeneous fluid or soft tissue opacity. The amount of bowel that contains gas in the normal cat and dog is variable. In nonfasted cats with no gastrointestinal disease, 65% had gas in greater than 25% of the small bowel.8 Cats without gastrointestinal disease that are not fasted before radiography may have gas throughout the bowel.8 In the fasted cat, gas is rarely present in the small intestine, but in fasted dogs, 30% to 60% of the small bowel content may be gas.6,11 Animals stressed by handling or dyspneic animals frequently are aerophagic, resulting in more air-containing small bowel. The gas pattern is variable; however, most cats and dogs have a linear pattern with gas in a continuous column except where interrupted by contraction. The bowel wall should be of uniform soft tissue opacity. This uniformity is most easily assessed in loops that contain air. As noted before, bowel wall thickness cannot usually be determined accurately in survey radiographs. Ultrasound or contrast radiography is indicated when the following are present: • Acute, persistent vomiting with negative findings on survey radiographs • Recurrent vomiting, especially in animals refractory to symptomatic therapy and without other organ disease to explain the vomiting • Palpable abdominal mass without obstructive bowel signs on survey radiographs • Acute abdominal pain with an unusual or unexplained abnormality seen in the survey radiographs • Weight loss with intermittent or recurrent diarrhea The major obstacle for optimal ultrasound imaging is the presence of gas in the bowel. When gas is present, the far wall cannot be assessed (Fig. 44-4). Repositioning the patient, using gravity-based transducer placement, administering fluid by orogastric intubation, or repeating the examination at a later time may overcome the artifacts induced by gas. The normal small intestinal wall pattern consists of alternating hyperechoic and hypoechoic layers. When no fluid or gas is present, a thin, hyperechoic line represents the lumen. From the lumen to the serosa, the layers and echogenicities are as follows: mucosa and hypoechoic, submucosa and hyperechoic, muscularis and hypoechoic, and serosa and hyperechoic (Fig. 44-5). The hypoechoic mucosal layer is the thickest of the individual layers and thus is dominant visually.12 When fluid is in the lumen, the mucosal surface is normally hyperechoic (see Fig. 44-4). If gas is present within the lumen, a prominent reverberation artifact occurs in a relatively long length of bowel and a comet tail reverberation artifact is present during peristaltic contraction. Both of these artifacts inhibit the assessment of the deeper wall. However, the presence of gas helps to identify the lumen in some abnormal segments. Acoustic shadowing artifact occurs frequently, either with focal luminal gas or with dense particles of ingesta in transit. A short linear or focal hyperechogenicity occurs frequently at the equatorial tangents of transverse sections of empty bowel. This occurs as a result of widening of the intervillous space when the bowel folds.13 Wall thickness variations for the dog and cat are summarized in Table 44-1. Higher frequency transducers and measures of wall thickness in a longitudinal axis segment provide a correlation between the thickness of the duodenum and jejunum relative to the weight of dogs.14 When a 10 MHz linear transducer is used in the normal cat, a subtle difference in thickness is found from the duodenum through the ileum.15 In normal 7- to 12-week-old beagle puppies ranging in weight from 2.3 to 5 kg, the bowel wall thickness was less than in adult dogs of similar weight.16 The normal duodenum can be identified distinctly by its superficial right-side location and can be traced cranially into the stomach and caudally to the descending loop, which courses to the left. With high-resolution transducers, the duodenal papilla can be seen in many cats and dogs (Fig. 44-6). The feline duodenal papilla ranges from 2.9 to 5.5 mm wide and averages 4.0 mm in height when imaged in the transverse plane.17 The major duodenal papilla is intimately adjacent to the right limb of the pancreas. Pseudoulcers can be seen occasionally in the canine duodenum, and the strong segmental contractions described as the string-of-pearls in a barium series can be seen in the feline duodenum. The jejunum and most of the ileum appear as nondescript loops. The terminal 1 to 2 cm of the ileum, or the ileocolic junction, in the cat has the appearance of a wagon wheel because of projection of the mucosa into the lumen.15 Peristaltic contractions can be seen and vary from less than 1 to 3 per minute in the small intestine depending on the fasted state or amount of time after being fed.18 Regional lymph node assessment should be included in any assessment of the small bowel. The duodenum is drained by hepatic and pancreaticoduodenal nodes. These nodes are not seen consistently in normal patients. The jejunum and ileum are drained by the jejunal and colic nodes, respectively, in the dog. In the cat, an ileocecal node is also present. Normal mesenteric lymph nodes can be difficult to identify with 5 MHz transducers; however, when 7.5 MHz or greater frequencies are used, these lymph nodes can be found in the majority of patients.15 Normal lymph nodes are typically isoechoic to adjacent fat and may not be differentiated readily. In the adult dog, the normal length of the jejunal nodes ranges from 5 to 200 mm.19 In normal beagle puppies, the jejunal lymph nodes were easily found and hypoechoic. Mean thickness ranged from 1.5 to 12.5 mm (mean 7.5 mm).16 In cats, the normal lymph node size guidelines in millimeters are pancreaticoduodenal length (L) 8.4 (6.6 to 13), diameter (D) 4.6 (3.6 to 6.2); jejunal L 20.1 (11.4 to 39.0), D 5.0 (2.8 to 7.2); and ileocecal L 11.8 (6.7 to 23.2), D 4.1 (2.7 to 4.8).20 Contrast studies of the small bowel can be used to identify the location of the bowel (e.g., displacement through hernias), to determine patency of the lumen, to identify perforation, and to identify irregularities in the contrast medium/mucosal interface. The concept of gastrointestinal contrast studies has been limited typically to the use of positive-contrast agents. However, the inherent gas contrast in the stomach and bowel should be used to full advantage as a contrast medium when present. The simple addition of the opposite lateral view and less frequently the dorsoventral view may shift the gas sufficiently to confirm an initial suspicion (Fig. 44-7) or discover new findings (Fig. 44-8).1 Ultrasound imaging affords greater contrast differentiation between soft tissue and fluid and between different soft tissue components such as the bowel wall layers. Because of this ability, ultrasound studies have replaced most radiographic positive-contrast studies of the bowel. If ultrasound imaging or the needed ultrasound interpretation expertise is not available, the positive-contrast small bowel study still has value. Probably its greatest usefulness for the general practice situation is the identification of abnormal bowel location and complete bowel obstruction. A few comments regarding positive-contrast small bowel studies follow; however, the reader is referred to the previous editions of this text for more thorough information.21 Positive-contrast evaluation is not indicated in the patient with clearly defined survey radiographic evidence of bowel obstruction.22 Minimal additional information will be gained because of the slowed passage through atonic bowel proximal to the obstruction, especially in a weakened or debilitated animal. If the clinical and survey radiographic findings are strongly suggestive of mechanical obstruction, surgery is indicated. Further attempts to define the specific site and type of obstructing lesion with contrast medium only delay and possibly complicate surgery and cause additional patient stress. Patients with survey radiographic evidence of free peritoneal gas that is not residual from recent celiotomy, penetrating trauma, or abdominocentesis are also not appropriate patients for intestinal contrast studies. In these patients, the peritoneal gas is most likely from gastrointestinal perforation.23 The combination of barium and ingesta within the peritoneal cavity causes more severe peritonitis, foreign body granulomas, or serosal adhesions.22,24,24 However, if treated promptly and aggressively, patient outcome can be good.26 Attempting to identify the location of the perforation is not as important as providing aggressive medical and surgical intervention. Ultrasound can also be used to detect free peritoneal gas associated with gastrointestinal perforation and prevents the additional contamination associated with barium leakage. Water-soluble organic iodine contrast media are either ionic or nonionic.27 Most ionic contrast media are hypertonic and cause an influx of fluid into the gastrointestinal tract. Ionic iodinated contrast media are not recommended for oral administration in young and debilitated patients and especially dehydrated patients, because the resultant fluid shift can worsen any hypovolemic state.28 A brief presentation of the techniques and interpretation of intestinal contrast studies follows. More detailed descriptions of techniques and normal interpretation can be found elsewhere.21 Contrast studies can be divided into two categories based on the radiographic opacity imparted by the contrast medium. Positive-contrast studies increase the opacity of the bowel lumen and are done with barium sulfate suspensions, iodinated products, and barium-impregnated polyethylene spheres (BIPS, Chemstock Animal Health Ltd., Christchurch, New Zealand). These contrast media are given orally or by orogastric intubation. Because the stomach is also opacified by these agents, except for the special case of BIPS, the phrase upper gastrointestinal contrast study is used. The volume of contrast medium in the intestinal lumen is a critical factor in interpretation. The intestine should be distended to its reasonable physiologic maximum. Failure to administer an adequate volume of contrast medium is one of the most frequent causes for a nondiagnostic barium study. Some recommended dosages for contrast medium are given in Table 44-2. A summary of the portions of the gastrointestinal tract seen at specific intervals after positive-contrast medium administration is presented in Table 44-3. Table • 44-2 Recommended Dose Rate for Contrast Medium †Follow manufacturer’s specific directions for administration with or without food. Table • 44-3 Upper Gastrointestinal Tract Film Sequence *Because of the extreme variability of individual transit times, this list is only an approximation of the parts of the gastrointestinal tract seen at these times. Normal anatomic features of the duodenum made visible by positive-contrast medium should not be misinterpreted as lesions. Dogs often have multiple square-shaped outpocketings on the antimesenteric side of the descending duodenum. One or several may be present. These are termed pseudoulcers and are normal and caused by mucosal depressions over submucosal lymphoid accumulations (Fig. 44-9). Pseudoulcers are not found in the cat. Approximately 30% of normal cats have strong segmental contractions throughout the length of the duodenum that produce a string-of-pearls effect during the contrast study (see Fig. 44-9).6 Pseudoulcers and the string-of-pearls appearance are seen mainly in positive-contrast studies and only rarely in survey radiographs. Throughout the remainder of the small bowel, concentric narrowing of short lengths of bowel should be seen and are caused by peristalsis (Fig. 44-10). The location of such narrowing should vary during the time of study in the normal animal. In a normal upper gastrointestinal study, barium and gas may be present simultaneously in loops (see Fig. 44-10). A double-contrast effect is present when the distention by gas is greater than that caused by the barium. The barium/mucosa interface appears typically in such loops as a thin opaque line. In other loops, gas may be present only as small bubbles. Findings on the barium contrast images that most strongly correlate with abnormalities are changes in the diameter of the bowel, extensive changes in the barium/mucosa interface, and changes in the rate of passage of barium. The intestinal tract is normally characterized by dynamic changes; thus documenting a suspicious finding on multiple radiographs over time increases the significance of the finding. BIPS are used mainly for evaluation of gastric dysmotility and intestinal transit time in the dog and cat. The spheres are made in two diameter sizes: 1.5 mm and 5 mm. The larger spheres are designed to become trapped at the oral aspect of an obstructing lesion, making them suitable for evaluation of partial and complete obstruction (Fig. 44-11).29
The Small Bowel
The Normal Small Bowel
Radiography
DOG
CAT
Radiographic*
Ultrasound wall thickness‡
Duodenum
2.0–2.4 mm
Ultrasound wall thickness‡
Jejunum
2.1–2.5 mm
Ultrasound wall thickness‡ Ileum
Not specifically defined
2.5–3.2 mm
Ultrasound
Contrast Examinations
Indications
Technique and General Interpretation
CONTRAST MEDIUM
DOG
CAT
Barium sulfate suspension*
6–12 mL/kg 20% (w/w)14
or 6–10 mL/kg 60% (w/w)
12–16 mL/kg6
Organic iodine preparation (full strength)
2–3 mL/kg8,14,14
2 mL/kg15
Organic iodine, nonionic (240–300 mg iodine/mL)
10 mL/kg (1 : 2 dilution)28
10 mL/kg (1 : 2 dilution)28,31
Radiopaque markers (BIPS)†
10 5-mm and 30 1.5-mm spheres
10 5-mm and 30 1.5-mm spheres
BARIUM
IONIC AND NONIONIC ORGANIC IODINE
STRUCTURES USUALLY OPACIFIED IN NORMAL ANIMALS*
Dog
Cat
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Small Bowel