CHAPTER 11 The Lymph Nodes
ARCHITECTURE
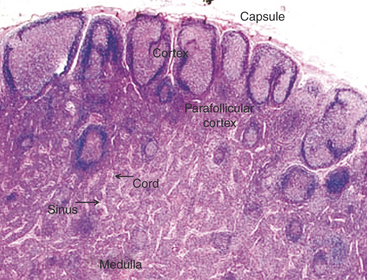
When interpreting a cytological specimen of the lymph node, it is useful to keep in mind the histological structure and different cell types that are found in this tissue. The node is composed of a capsule, cortex, medulla, and sinuses (subcapsular, cortical, and medullary).1 The cortex or more peripheral area of the node is divided into follicular and diffuse (parafollicular cortex or paracortex) regions, and the medulla or more central area, into the medullary cords and sinuses (Figure 11-1).
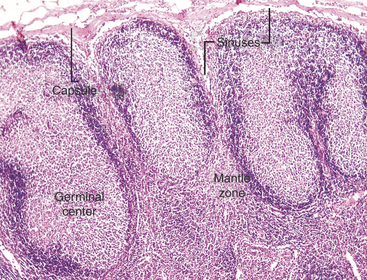
Lymph nodes are strategically located at sites throughout the body and are involved in a variety of local and systemic disease processes. Antigen reaches the node via the afferent lymphatics. The lymph percolates through the sinus and sinusoidal walls into the parenchyma (Figure 11-2), where foreign substances (antigens) are taken up and processed by specialized cells of the MPS. The sinuses (subcapsular, cortical and medullary) form a network of branching channels that converge at the hilus of the node to exit by the efferent lymphatics. The primary functions of the lymph nodes include filtering particles and microorganisms, exposing antigens to circulating lymphocytes, and activating B- and T-lymphocytes. The superficial, subcutaneous location of some lymph nodes (mandibular, superficial cervical, inguinal, and popliteal) allows easy detection of enlargement and access for fine-needle aspiration (FNA) cytology. It is appropriate to aspirate any node that is enlarged, and in the case of lymph nodes draining areas affected by neoplasia, even in the absence of enlagement, aspiration may be justified.2
GENERAL CONSIDERATIONS
Lymph node aspiration cytology has become a popular procedure in human medicine in recent years, because of its great convenience.3 Similarly, this high-yield diagnostic technique is frequently used in veterinary medicine.4–7 There are a few points to consider when obtaining nodal samples for cytological evaluation.
Consideration also should be given to the size of the lymph node when deciding which node to aspirate — very large nodes may have areas of hemorrhage or necrosis. If the node must be sampled, the needle should be directed tangentially, avoiding the more central portions.8 Finally, when obtaining a sample for cytological evaluation, it is important to remember that the lymph node is a heterogenous tissue, and multiple areas within the node should be sampled to be certain that what you have obtained is representative. While keeping the needle in the node, repeatedly advance and withdraw the needle in multiple directions until a small amount of aspirate appears in the hub of the needle. This procedure can be done using a syringe to apply gentle suction or with only the needle. If the former technique is used, release the suction before removing the needle from the node. Overly vigorous aspiration of the lymph node can produce significant hemodilution and cells can rupture, limiting the interpretation of your sample. A large volume of aspirate is not required; the material within the hub of your needle is sufficient for making cytologic preparations. Because the lymphocytes are fragile, care also must be taken to apply only minimal pressure when making slide preparations to prevent excessive rupturing of cells. The slides are air-dried (not heat-fixed) and stained for evaluation.
FINE-NEEDLE ASPIRATION
FNA is a relatively safe and painless procedure, allowing for rapid and inexpensive sampling of peripheral lymph nodes. It does not require hospital admission or anesthesia of the pet. The role of this procedure is summarized in Box 11-1.
Box 11-1 The Role of Fine-Needle Aspiration Cytology of Lymph Nodes
CYTOLOGIC FINDINGS
Normal Lymph Node
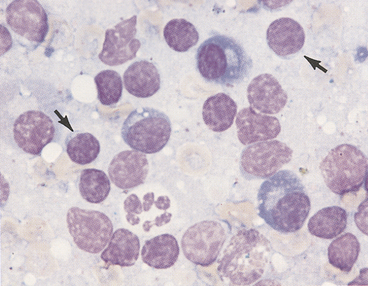
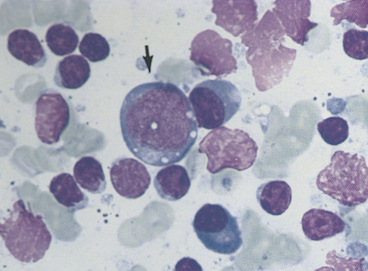
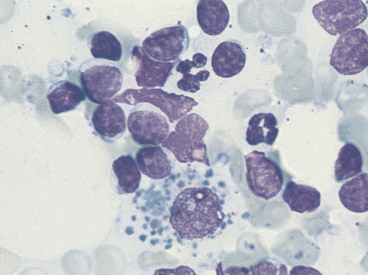
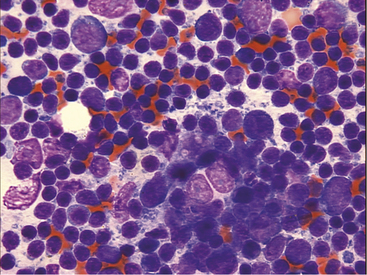
In the absence of architectural features that can be appreciated in a histologic section of a lymph node, the interpretation of cytology relies on proportions of different cell types and an understanding of what proportions are normal versus abnormal for these cell types. Small, well-differentiated lymphocytes compose greater than 75% to 85% of the total nucleated cell population (Figures 11-3 through 11-7).4–7 They have round nuclei that are about 1.0 to <1.5 times the size of a mature red blood cell (RBC) with an overall cell size that is smaller than that of a neutrophil. Their chromatin is densely clumped and nucleoli are not visible. The nuclear-to-cytoplasmic ratio is high with a narrow rim of basophilic cytoplasm. In addition to small lymphocytes, a normal node should have low numbers (<10% to 15%) of lymphocytes that are intermediate to large (often called lymphoblasts) in size; their nuclei are 1.5 to 3 times the size of an RBC with an overall size ranging from about that of a neutrophil or larger to up to 4 times the size of an RBC (see Figure 11-5). Their chromatin is less clumped and nucleoli may be visible and even multiple and/or prominent. The cytoplasm is pale blue and more abundant than in small lymphocytes.
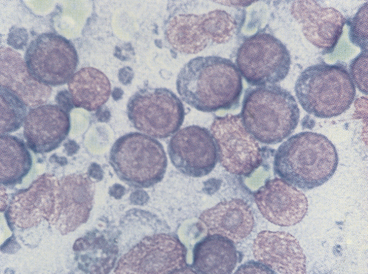
Plasma cells have small, round, eccentric nuclei with condensed chromatin (see Figures 11-3 through 11-6). Their abundant cytoplasm is deep blue and has a prominent, clear Golgi zone. Immature plasma cells (transformed B-lymphocytes) are larger and have less aggregated chromatin and a higher nuclear-to-cytoplasmic ratio (see Figure 11-4). Their very blue cytoplasm may contain discrete vacuoles. Plasma cells in various stages of development are seen in small numbers in normal lymph nodes, but typically represent <3% of the total nucleated cell population.
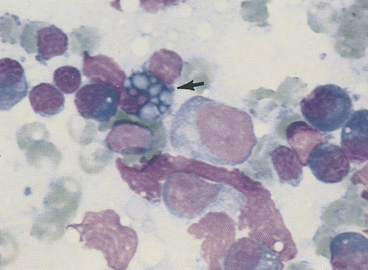
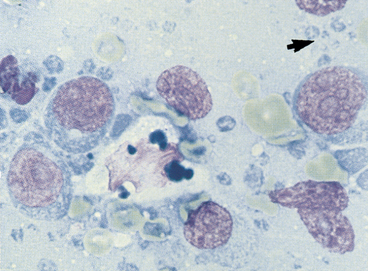
Macrophages, characterized by abundant cytoplasm often containing vacuoles and granular debris, also are found in small numbers (see Figure 11-7). Macrophages from areas of intense lymphopoiesis and cellular turnover may contain prominent basophilic nuclear debris (tingible bodies) (Figure 11-8). Occasionally, small numbers of neutrophils, eosinophils, and mast cells are observed in a normal node (see Figure 11-6). Each of these cell types should represent less than 1% of the cell populations in a normal node. It is important to consider the amount of blood contamination when making this assessment. Reticular cells and endothelial cells are common in lymph nodes, but these tissue-bound cells are rarely aspirated intact. They usually appear as large swollen nuclei, often devoid of cytoplasm (Figure 11-9).
Because of the pressures of the aspiration technique, lymphocytes, which are very fragile, may rupture and release their nuclei. Free nuclei are swollen and uniformly pink in contrast to the blue blocky or granular pattern of intact lymphocyte nuclei (see Figures 11-3 through 11-5). Blue nucleoli are often exposed in the nuclear chromatin of ruptured cells. These free nuclei carry no diagnostic significance and should not be confused with large immature lymphocytes. Lymphoglandular bodies are cytoplasmic fragments and are highly characteristic of lymphoid tissue (see Figures 11-8 and 11-10). They are round, homogeneous, basophilic structures similar in size to platelets.
LYMPHADENOPATHY
Lymphadenitis
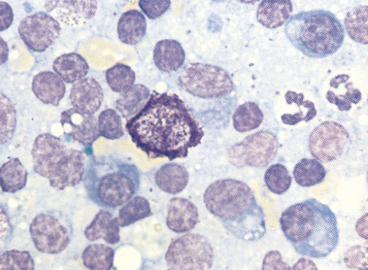
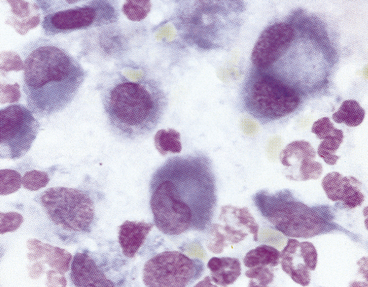
Lymphadenitis or inflammation of the node may be a primary (node itself is inflamed or necrotic) or secondary (node is draining an area of inflammation or necrosis) finding. This process is characterized cytologically by accumulation of inflammatory cells. Neutrophils, eosinophils, and macrophages occur singly or in combination. Inflammation is probably present when the population is >5% neutrophils or >3% eosinophils, provided there is no significant blood contamination. Macrophage numbers can increase in inflammation but also in hyperplasia and sometimes in neoplasia. Macrophages also may appear as epithelioid cells and multinucleated giant cells in granulomatous inflammation. Epitheloid macrophages are characterized by blue cytoplasm with minimal vacuolation and contain very little phagocytic debris (Figure 11-11). Organisms may, however, be present within the cytoplasm. These cells may occur in aggregates. Inflammatory cells may represent only a small portion of the total cell population that otherwise suggests lymphoid hyperplasia, or they may completely replace the normal cell population.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree