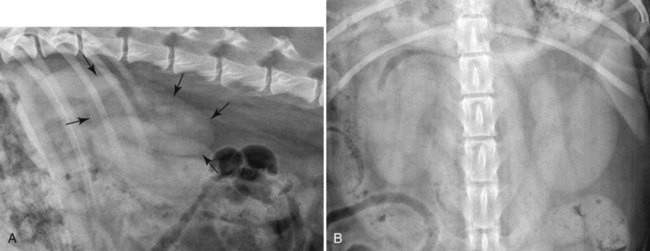
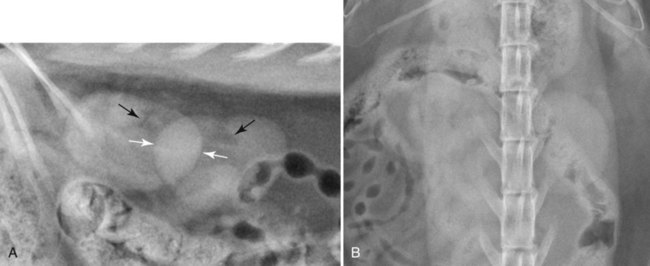
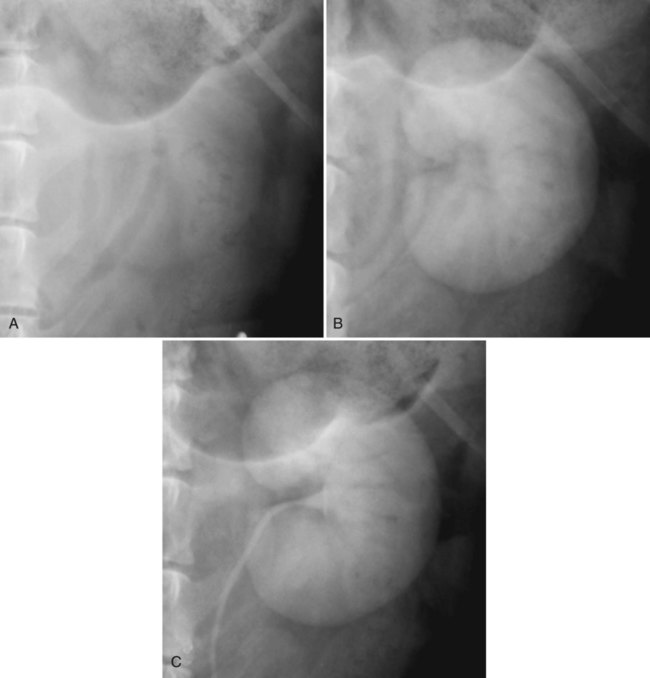
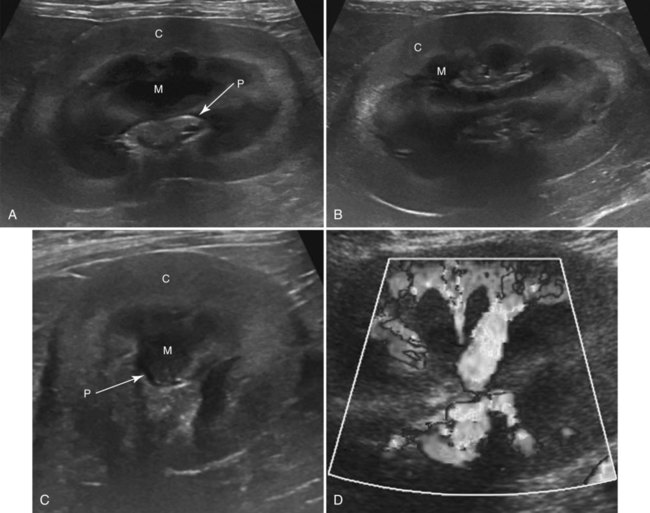
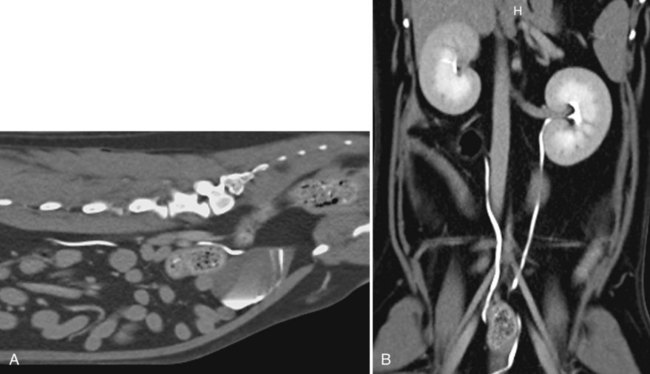
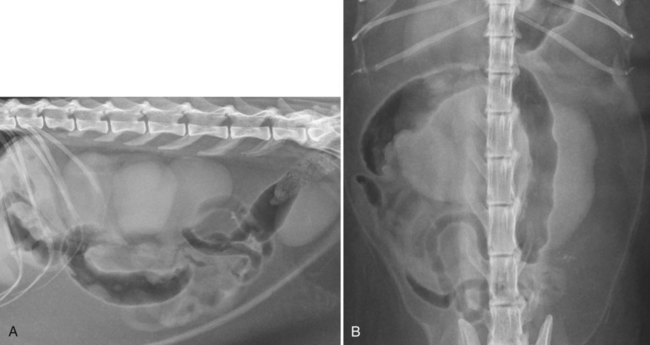
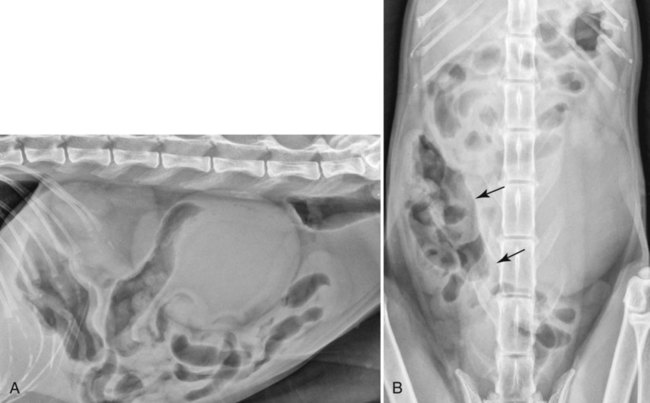
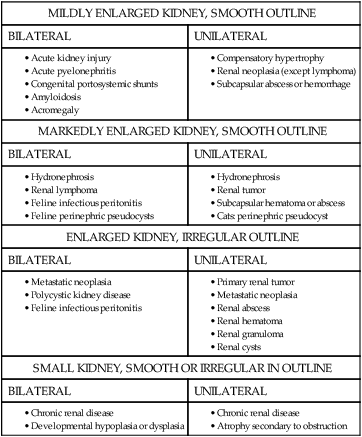
Radiographs are useful to identify changes in size, shape, and opacity of the kidneys and to identify associated retroperitoneal disease. Radiopaque nephroliths and ureteral calculi are identified readily. Radiographs should always be obtained if urinary tract obstruction is suspected because ureteral calculi can be difficult to detect ultrasonographically.1 Also, survey radiographs should always be obtained if there is a history of trauma to the abdomen or pelvis with suspected involvement of the urinary tract or if a dorsal abdominal mass is suspected. Survey radiographs are an essential part of any abdominal radiographic procedure involving contrast medium. Orthogonal radiographic projections are needed for a thorough evaluation of the abdomen. This was discussed in detail in Chapter 35. Right lateral radiographs provide more longitudinal separation between the right and left kidney.2 Suspected ureteral calculi can be separated from gastrointestinal content by use of oblique projections or compression techniques. Feces may have to be eliminated, by means of fasting or an enema, before a radiographic study to evaluate the distal ureters fully. The kidneys are located in the retroperitoneal space and outlined by surrounding fat. Canine kidneys are oval (Fig. 38-1). The cranial pole of the right kidney is often poorly visible because it abuts the caudate lobe of the liver. The right kidney is usually located at the level of the thirteenth rib. The left kidney is located more caudally, at the level of L1-L3, and is visible more consistently. The left kidney is also more mobile than the right, and it can be positioned relatively ventrally in animals with a large amount of retroperitoneal fat. On the ventrodorsal projection, the right kidney is often obscured by liver and other superimposed abdominal organs, whereas the left kidney is normally visible caudal to the gastric fundus and caudomedial to the proximal extremity of the spleen. Feline kidneys are round or oval and are located typically between L1 and L4, either at the same level or with the right kidney in a more cranial position (Fig. 38-2). On lateral radiographs, the caudal pole of the right kidney may overlap the cranial pole of the left kidney and the summation of the two poles can give the false impression of a small rounded kidney or a retroperitoneal mass (Fig. 38-2, A). Normal feline kidneys often have a fat opacity at the renal hilus (see Fig. 38-2, A). Ectopic kidneys in a very caudal location are reported sporadically.3 Normal ureters are not visible radiographically. Detecting a change in kidney size is helpful for classification of renal diseases into acute or chronic. In general, assessment of renal length is more reliable on ventrodorsal projections because there is no overlap of the kidneys, and magnification of both kidneys is equal. Normal renal length has been described in relationship to the length of the second lumbar vertebra. Renal length in normal dogs ranges between 2.5 and 3.5 times the length of L2.4 In cats, the normal renal length has been measured to be 2.4 to 3.0 times the length of L2.5 Older cats without signs of renal disease can have smaller kidneys (1.9 to 2.6 times the length of L2); however, it is difficult to know whether subclinical renal disease may have been present in these cats.5–6 Hormonal influence depending on reproductive status alters renal length in cats, both in males and females. Intact cats tend to have larger kidneys (range 2.1 to 3.2 times the length of L2) than neutered cats (1.9 to 2.6 times the length of L2).7 It is important to realize that these normal relationships were determined from a relatively small number of cats and are intended only to be guidelines. Normal kidneys are of homogeneous soft tissue opacity, although fat deposition in the renal pelvis in cats can lead to focal central radiolucency (see Fig. 38-2, A). Mineralizations associated with the kidneys or ureters are always abnormal, although they may not necessarily be associated with clinical signs. Adverse reactions to intravenous administration of iodinated contrast medium, such as nausea, vomiting, hives, hypotension, and contrast-medium–induced renal failure are uncommon but do occur occasionally. Use of nonionic contrast medium leads to fewer complications because of the lower osmolarity.8–9 Risk factors for contrast-medium–induced nephropathy include renal insufficiency and poor hydration status.10–11 Contraindications for excretory urography, therefore, include anuric renal failure, dehydration, or hypotension and known hypersensitivity to iodinated contrast media. Patient preparation is a key to obtaining a diagnostic excretory urogram. Food, but not water, should be withheld for at least 12 to 24 hours before the study. A cleansing enema can be used to evacuate the colon, preferably several hours before the study to allow fecal material and gas to pass. The patient should be hydrated and have adequate renal function. Because iodinated contrast medium leads to increased urine-specific gravity and may also inhibit bacterial growth for at least 24 hours, urinalysis should be performed before excretory urography.12 Survey radiographs are always obtained before an excretory urogram to ensure correct radiographic technique and assess colon contents, but most important, small radiopaque calculi may be obscured by the contrast medium. Sedation or general anesthesia is recommended, and an intravenous catheter should be in place throughout the study to provide venous access if complications arise. Iodinated contrast medium is administered intravenously as a bolus injection at a dose of 600 to 700 mg iodine (I) per kg body weight.13–14 Ventrodorsal and right lateral radiographs are acquired immediately after injection and are repeated typically after 5, 20, and 40 minutes or until a diagnosis is reached. Oblique projections for better visualization of the ureters can be added at 5 minutes and later time points. To evaluate the renal arteries, a ventrodorsal radiograph should be acquired 5 to 7 seconds after bolus injection of contrast medium. The renal arteries become opacified approximately 5 to 7 seconds after injection of a bolus of contrast medium. The excretory urogram can be divided into two phases: the nephrogram phase and pyelogram phase. In the nephrogram phase, contrast-medium arrival in the glomerular vessels and filtration into the nephron leads to uniform opacification of the renal parenchyma (Fig. 38-3, B). Initially, the cortex can be more opaque than the medulla. The nephrogram begins after approximately 10 seconds and lasts up to 2 minutes until the pyelogram phase starts and the nephrogram begins to fade. Nephrogram opacity should continue to decrease progressively; only approximately 25% of normal dogs still have a detectable nephrogram 2 hours after contrast medium injection.15 In the pyelogram phase, contrast medium is concentrated in renal tubules as a result of reabsorption of water and excreted into the renal pelvis with its diverticula, and the ureters (Fig. 38-3, C). If renal function is normal, the collecting system is consistently more opaque than the renal parenchyma. The normal renal pelvis is curvilinear and less than 2 mm in width. The pelvic diverticula may be seen in some dogs and most cats and appear as thin (1 mm) spikes radiating from the pelvis toward the periphery. Neither the renal pelvis nor diverticula should have blunted, rounded edges. The ureters tend not to be filled with contrast medium uniformly throughout their length because of ureteral peristalsis. Radiographs, therefore, may have to be repeated to assess the entire length of the ureters. Normal ureters are not more than 2 to 3 mm in width. They terminate at the dorsal aspect of the bladder neck, where they curve cranially for a short distance before entering the wall. Duration and intensity of the opacification of the kidney during an excretory urogram depends on the dose of contrast medium administered; renal perfusion; glomerular filtration; tubular reabsorption of water; the patient’s hydration status, which is important to maintain adequate renal perfusion; and patency of the renal outflow tract.14 Duration and degree of kidney opacification during an excretory urogram is an indication, although not very precise, of renal function and has to be monitored closely throughout the study, as described later under renal function. Ultrasound-guided injection of contrast medium into the renal pelvis leads to excellent opacification of the collecting system because the contrast medium is not diluted, and its presence in the collecting system is not dependent on renal function. This procedure can be performed in azotemic patients without loss of image quality. In addition, each renal pelvis and ureter can be assessed individually. Other advantages include the lack of systemic contrast-medium reactions, and collection of urine directly from the renal pelvis for urinalysis and microbiologic testing. The main indication for this procedure is suspected ureteral obstruction. Some degree of renal pelvis distention (at least 3-5mm) has to be present to perform the procedure. Contraindications include clotting disorders, as some hemorrhage may occur. Contrast medium may also leak into the retroperitoneal space.16 Although this leakage is usually insignificant clinically, radiographic interpretation may be compromised. Loss of renal function secondary to the procedure is minimal but should be a consideration in patients with already severely compromised renal function. Sedation or general anesthesia is necessary. The skin is prepared aseptically, and a 25-gauge needle connected with an extension set and three-way stopcock is introduced into the renal pelvis under ultrasound or fluoroscopic guidance. Depending on the size of the renal pelvis, 1 to 2 mL of urine is removed for laboratory testing. Ionic or nonionic iodinated contrast medium equivalent to half of the volume of urine removed is then introduced slowly, and the size of the renal pelvis is monitored with ultrasound or fluoroscopy.16 Occasionally, replacement of the entire volume of urine removed is needed. Overdistention of the renal pelvis should be avoided because rupture may occur. Immediately after contrast-medium injection, ventrodorsal, oblique, and lateral abdominal radiographs are acquired. If bilateral abnormalities are suspected, the procedure can be repeated on the contralateral side. The renal pelvis becomes distended with mild blunting of the pelvic diverticula, as contrast medium is introduced under mild pressure. If the ureter is patent, contrast medium should appear in the urinary bladder almost immediately (Fig. 38-4). Narrowing of the ureter may be observed because of peristalsis. Ultrasound is the method of choice to evaluate renal architecture and vascularity. Ultrasonographic evaluation of the renal parenchyma is indicated at the first sign of renal dysfunction. Although ultrasound findings are usually not disease-specific, it allows differentiating acute and chronic renal changes, mass lesions, cysts, mineralizations, and alterations of the collecting system and ureters. Needle aspirates or biopsies can be obtained under ultrasound guidance.17–19 Renal ultrasound can be used as a screening tool for congenital renal disease such as aplasia, hypoplasia or dysplasia, and polycystic kidney disease.3,20–22 Abnormal renal perfusion caused by infarction, transplant rejection, or mass lesions can be investigated using Doppler ultrasound.23 Contrast-enhanced ultrasound of the canine and feline kidney has potential for delineation of renal parenchymal lesions such as masses or infarcts.24–26 The highest frequency transducer that manages to penetrate adequately should be chosen to image the kidneys. In smaller dogs and cats, 7.5 to 15 MHz is appropriate; 5 MHz or lower frequency transducers should be used only in large dogs. Subcostal or intercostal windows with the patient in sternal or dorsal recumbency allow access to the kidneys, depending on patient size and thoracic conformation. Standard image planes include dorsal (Fig. 38-5, A), sagittal (Fig. 38-5, B), and transverse (Fig. 38-5, C) views, always followed by fanning the transducer through the entire kidney. The renal pelvis is visible best in dorsal and transverse image planes. The ureters can be followed caudally from the renal pelvis if dilated. To verify patency and normal location of the ureterovesical junction, the bladder should be evaluated for presence of two urine jets from the dorsolateral bladder wall. If not seen with conventional grayscale imaging, Doppler ultrasound can be used to better delineate the jet. In some animals, administration of a diuretic is necessary to increase urine production and alter the specific gravity of the urine produced compared with the urine already present in the bladder; this will increase the frequency and visibility of a ureteral jet. Normal canine and feline kidneys are outlined smoothly by a thin hyperechoic capsule and have a clear distinction between cortex and medulla (see Fig. 38-5). The renal cortex in most patients is hypo- to isoechoic to the liver and spleen, although dogs and cats without evidence of renal disease may have a renal cortex that is hyperechoic to liver.27 In cats, cortical hyperechogenicity can be seen in association with fat deposition.28 The normal medulla is very hypoechoic, creating a well-defined transition to the cortex. The interlobar vessels and pelvic diverticula give the renal medulla a lobulated appearance. The arcuate vessels are seen at the corticomedullary junction as short, hyperechoic parallel lines that may produce a distal shadow, not to be confused with renal mineralization. The renal pelvis is collapsed normally, but a smoothly margined, thin rim of fluid of up to 2 mm in diameter can be seen in normal animals, especially when using high-resolution transducers.29 Increased diuresis, caused by exogenous fluid administration or polyuria/polydipsia, results in mild pyelectasia.29 The pelvic diverticula are not visible normally. The renal pelvis is surrounded by the hyperechoic sinus, which contains dense fibrous tissue and fat, particularly in overweight cats. Normal kidney size in cats ranges between 3.0 and 4.3 cm.30–31 In dogs, size is much more variable depending on body weight and conformation. As a rule of thumb, 10 mm per 10 pounds can be added within the normal range of 3 to 10 cm.32 A ratio of 5.5 to 9.1 of the maximal renal length to the luminal diameter of the aorta at the level of the kidney is proposed to take patient size into account.33 Even using this method, the large range of normal values makes detection of subtle size changes challenging. Renal length, therefore, is not very helpful as an isolated criterion, unless markedly abnormal and all other ultrasonographic findings have to be taken into account to determine if a kidney is normal or not. With Doppler ultrasound, the renal artery and vein, interlobar, arcuate, and interlobular vessels can be identified (Fig. 38-5, D). The resistive index should be less than 0.72 in dogs and 0.70 in cats, and the pulsatility index less than 1.52 in dogs and 1.29 in cats.34 Normal ureters are visible only with high-resolution imaging systems, and ideal patient-related conditions. Ureters are best followed from a transverse view of the renal pelvis, as they turn medially and can be tortuous until they extend caudally, lateral to the aorta and caudal vena cava. Thin hyperechoic walls and occasional waves of peristalsis with a small bolus of fluid passing through can be seen in a normal ureter. Computed tomography (CT) is being used with more frequency for renal imaging. Indications are essentially the same as for an excretory urogram, but CT has the advantage that the entire urinary tract can be imaged without superimposition of any other structure. A reduced dose of contrast medium (400 mg I/kg body weight) results in adequate image quality, which could be advantageous in patients with compromised renal function.35–36 Multiplanar and 3D reconstructions add valuable information. Additionally, it is possible to calculate glomerular filtration rate using contrast-enhanced CT imaging.37 As with excretory urography, limitations include the need for anesthesia or sedation and the need for intravenous contrast-medium administration. Imaging protocols always include a precontrast image series to identify presence of mineralization in the renal parenchyma or collecting system because mineralization cannot be differentiated from the hyperattenuating contrast medium. In most patients, intravenous contrast medium has to be administered (400 to 800 mg I/kg body weight) to outline renal parenchymal lesions and filling defects in the collecting system. The renal parenchyma is enhanced immediately after contrast-medium administration. Optimal ureteral opacification occurs 3 minutes post injection35; however, image series may have to repeated several times to visualize the entire course of both ureters because of ureteral peristalsis. Ureteral opacification persists for about 1 hour.35 Patient positioning in sternal recumbency with the pelvis elevated is helpful in outlining the ureterovesical junctions because the contrast medium will accumulate in the bladder apex away from the neck, facilitating the distinction between the contrast-medium–filled ureters and the bladder neck (Fig. 38-6). Filling the bladder with carbon dioxide increases the contrast between the bladder and ureters further; however, the balloon of the Foley catheter may distort anatomy and impair visibility of the ureteral openings. Dual-phase renal angiography can be performed to assess the arterial and venous blood supply of the kidneys separately. This is used mainly for presurgical assessment of feline kidney donors.38–39 Normal kidneys are soft tissue attenuating, except for a small amount of fat surrounding the renal pelvis. Uniform contrast enhancement is expected, followed by concentration of the contrast medium in the renal pelvis and diverticula, ureters, and urinary bladder (see Fig. 38-6). Magnetic resonance imaging is used in people to assess renal diseases, perfusion, and function, but little work has been performed in small animals. Advantages and indications are similar to those described for CT, but use has so far been limited by cost, availability, and duration of the imaging studies. Protocols for magnetic resonance angiography of the renal vasculature in renal transplant donors are available.40 Compared with other renal function testing, renal scintigraphy using technetium-99m diethylenetriamine pentaacetic acid has the advantage of being able to determine the relative contribution of each kidney to total renal function. This is especially important in patients with impaired renal function before planned nephrectomy. To describe the technique of renal scintigraphy in detail is beyond the scope of this chapter, and readers are referred to the literature.41 It is important to keep in mind that renal size and shape may be normal in the presence of renal disease. Especially acute toxic, inflammatory, or infectious nephropathies, as well as amyloidosis, do not always lead to alteration of renal size or shape.42 Renomegaly leads to a mass effect in the retroperitoneal space, evidenced by ventral displacement of the gastrointestinal tract and other organs (Fig. 38-7). Left renal enlargement leads to ventral or lateral displacement of the descending colon and small intestines (Fig. 38-8), whereas right renomegaly is associated with ventral displacement of the ascending colon and duodenum (Fig. 38-9). Differential diagnoses for renomegaly are subdivided based on presence of unilateral versus bilateral enlargement and alterations in margination and are listed in Table 38-1.43 Contrast procedures (excretory urography or CT), as well as ultrasound, have to be used to determine if the renal enlargement is caused by parenchymal disease or by dilation of the collecting system or renal capsule. Ultrasound is currently the method of choice to evaluate an enlarged kidney; detailed findings are described later. Table • 38-1 Differential Diagnoses for Changes in Renal Size and Shape
The Kidneys and Ureters
Normal Anatomy and Imaging Procedures
Radiography
Indications
Technique
Normal Imaging Findings
Excretory Urography
Indications
Technique
Normal Imaging Findings
Antegrade Ultrasound-Guided Pyelography
Indications
Technique
Normal Imaging Findings
Ultrasonography
Indications
Technique
Normal Imaging Findings
Computed Tomography
Indications
Technique
Normal Imaging Findings
Magnetic Resonance Imaging
Scintigraphy
Renal Diseases
Abnormal Renal Size
Large Kidneys
MILDLY ENLARGED KIDNEY, SMOOTH OUTLINE
BILATERAL
UNILATERAL
MARKEDLY ENLARGED KIDNEY, SMOOTH OUTLINE
BILATERAL
UNILATERAL
ENLARGED KIDNEY, IRREGULAR OUTLINE
BILATERAL
UNILATERAL
SMALL KIDNEY, SMOOTH OR IRREGULAR IN OUTLINE
BILATERAL
UNILATERAL
The Kidneys and Ureters