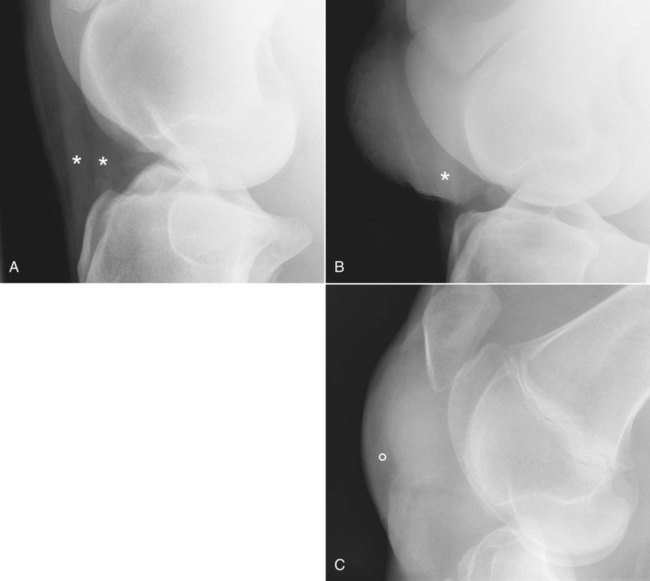
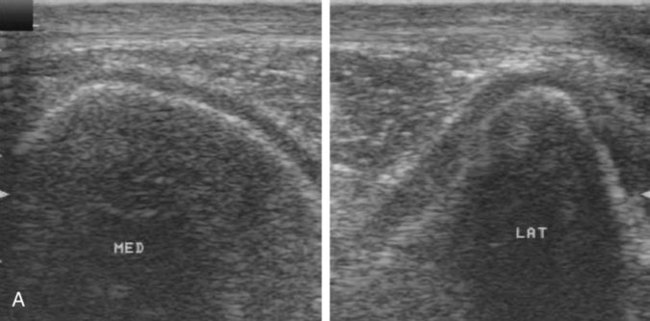
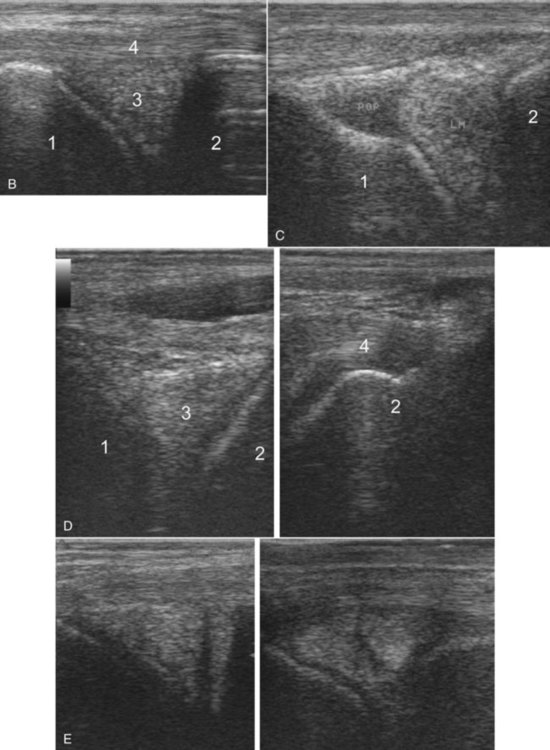
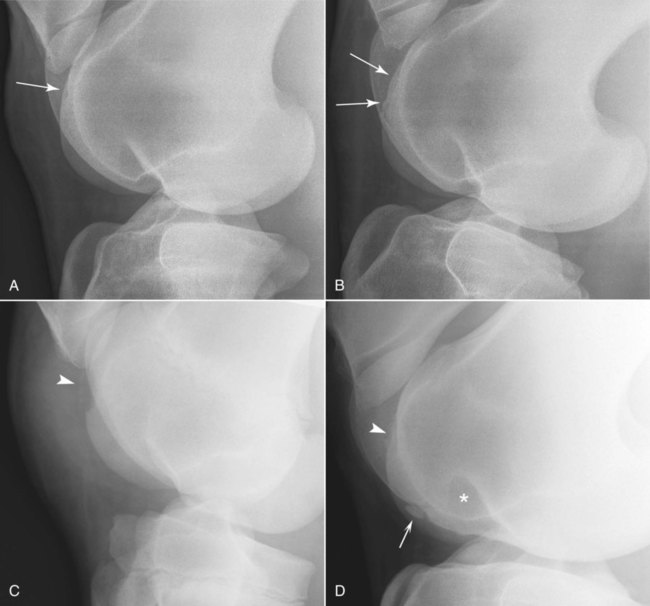
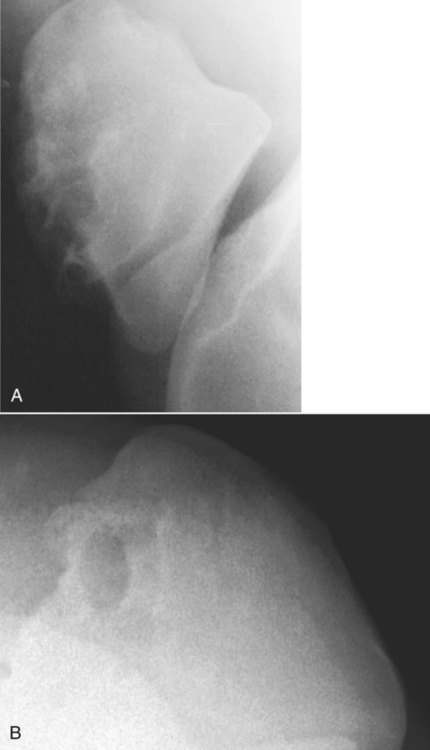
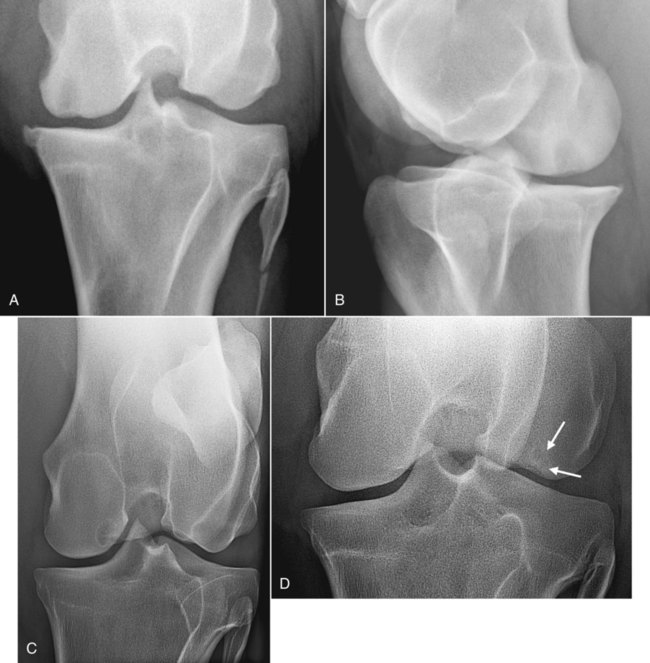
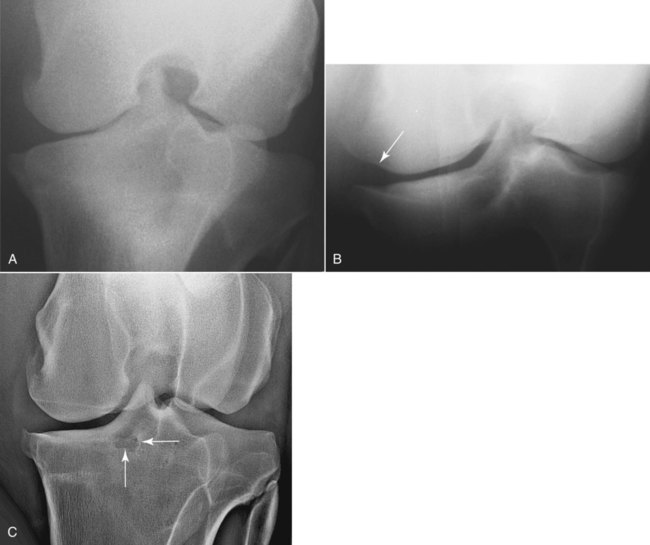
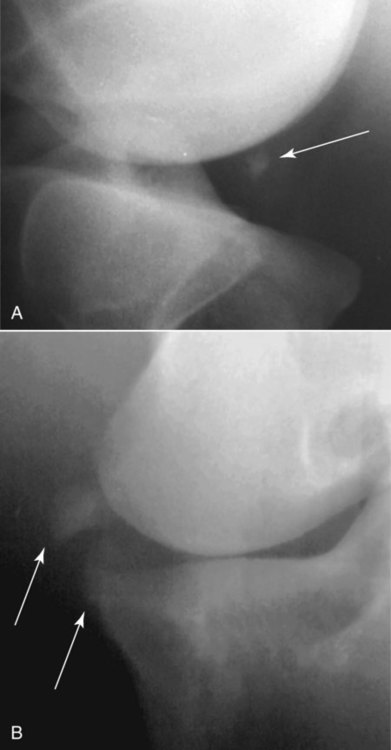
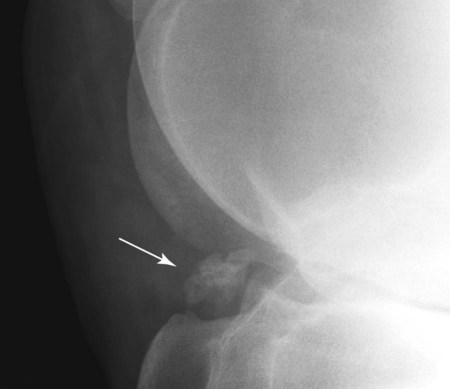
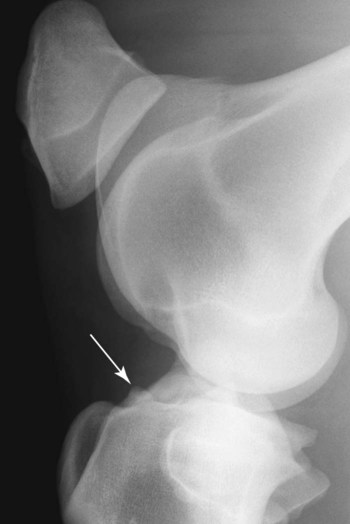
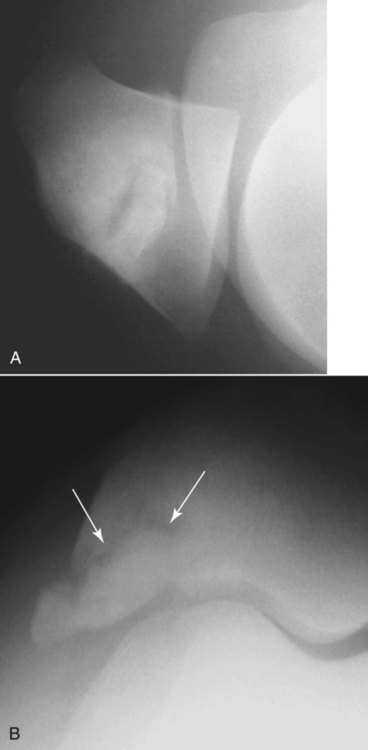
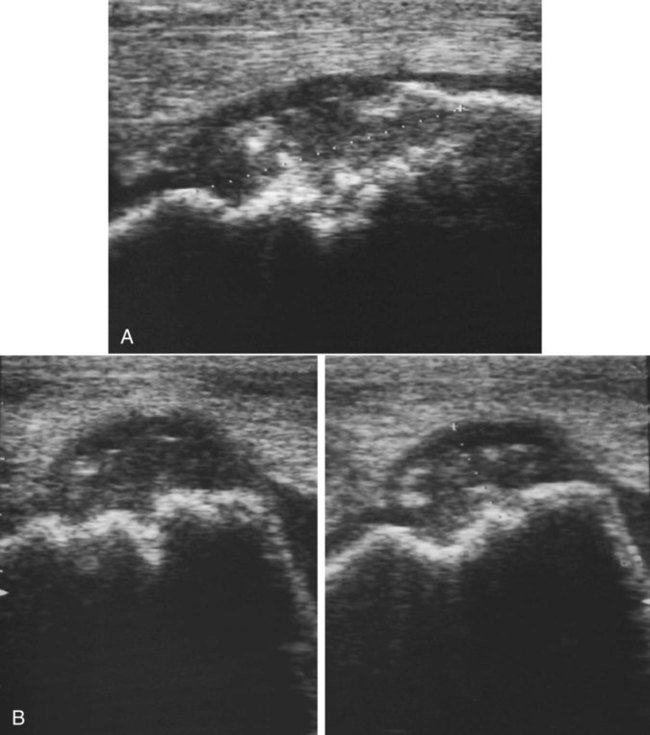
Stifle radiographs are acquired frequently on clinical patients, and in presale examinations and screening radiographic protocols in young horses.1–3 Because positioning errors are the most common reason for radiographs to be nondiagnostic,4 a good knowledge of radiographic technique is crucial to assess the thick stifle region. With the advent of digital radiography and its inherently greater contrast resolution, radiographic evaluation of the soft tissues of the stifle is possible to a certain extent. Lateromedial radiographs of the stifle allow good visualization of the patellar ligaments and the cranial fat pad (Fig. 19-1). Localization of soft tissue swelling as being extraarticular or intraarticular is possible by evaluating border effacement and fat pad displacement (see Fig. 19-1). Subchondral cystlike lesions and tibial or femoral osteophyte formation as a result of osteoarthrosis are the most common radiographic signs of femorotibial disease. Bony fragments, new bone formation, or radiolucent areas at ligament insertions, suggesting avulsion fractures or enthesopathy, may also be seen.5–7 However, because of the high incidence of soft tissue lesions involving menisci and ligaments, femorotibial pain may be present with no or minor radiographic signs.5–7 When clinical signs suggest femorotibial involvement, all abnormalities are not likely to be diagnosed radiographically because assessment of soft tissue lesions is not possible. The severity of the lameness, the midterm prognosis for a return to work, or the long-term prognosis for development of osteoarthrosis depends mainly on the severity of the soft tissue injuries, in particular meniscal damage.8–10 A combination of ultrasonographic and radiographic examination is therefore necessary for complete assessment of the stifle.6 Ultrasonography of the weight-bearing stifle allows easy assessment of the femoropatellar and femorotibial synovial recesses, the femoral trochlea, the patellar ligaments, the menisci, the collateral ligaments, and the medial femorotibial joint margins (Fig. 19-2).11–12 In the flexed stifle, ultrasonography allows visualization of the cranial horns of the menisci, the cranial meniscal ligaments, and a portion of the articular surface of the medial and lateral femoral condyles (see Fig. 19-2).13 Ultrasonography is the technique of choice to diagnose meniscal damage, which frequently affects sport and pleasure horses.8 Although specificity is relatively low using arthroscopy as the gold standard,8 a good correlation between histologic changes and ultrasonographic images has been suggested.14 Although osteochondrosis lesions develop early in life, osteochondrosis of the femoropatellar joint is a common radiographic finding in both young and older horses.1–3,15,16 Lateromedial or caudolateral-craniomedial views are necessary to evaluate the femoral trochlea in young horses with synovial distention of the femoropatellar joint. Radiographic signs of osteochondrosis include flattening, irregular subchondral surface, heterogeneous opacity of the trochlear ridge, and presence of bony fragments attached by a radiolucent junction to the bone surface at the cranial aspect of the trochlea (Fig. 19-3). The most common site of osteochondrosis in the equine stifle is the lateral femoral trochlear ridge, especially the middle third.1–3,15–17 This type of lesion may influence sport and racing performances of affected horses.18 The trochlear groove may be involved occasionally,17 with or without associated trochlear ridge involvement, but trochlear groove lesions generally have less clinical significance than ridge defects. Lesions of the medial femoral trochlear ridge are less common (see Fig. 19-3).3,16,17,19 Patellar lesions are rare and seen mainly with severe trochlear abnormalities.20 An osseous cystlike lesion has been reported in the proximal medial aspect of the patella in a young horse, but because it was located at the site where most patellar fractures occur, the cause was uncertain.21 Taking into account the age of development of osteochondral lesions of the femoral trochlea, radiographic screening of the stifle for osteochondrosis should not be performed before 8 to 12 months of age.15 Because of possible bilateral involvement, both stifles should always be examined. Because the femoral trochlea cannot be evaluated on the caudocranial view, and lateromedial and caudolateral-craniomedial views do not allow precise estimation of the mediolateral extent of the lesion, ultrasonographic examination of the cranial aspect of the stifle may be helpful before surgery to assess articular cartilage damage and to better define the long-term prognosis (Fig. 19-4). Because of its higher sensitivity compared to radiography, especially for medial trochlear ridge defects, ultrasonography is also useful in horses where radiographic signs are equivocal.17 Patellar fragmentation affects the patellar apex and is seen primarily in horses that have undergone medial patellar desmotomy.22–24 The fragmentation is the consequence of patellar instability after desmotomy.22 One or multiple bone fragments may be present (Fig. 19-5). Remodeling of the tibial tuberosity at the insertion of the patellar ligaments and remodeling or enthesopathy of the patella may be present in association with fragmentation of the apex.22–24 An increase in the angle between the proximal articular surface of the patella and the cranial surface of the femur occurs because of patellar instability following medial patellar desmotomy and may be seen in horses with patellar fragmentation.22 For patellar fractures, see the “Fractures Involving the Stifle” section. No radiographic sign can be used to confirm the clinical diagnosis of recurrent upward patellar fixation. Radiographic examination of the stifle is recommended to exclude other lesions. Horses with recurrent partial upward patellar fixation may have remodeling of the patellar apex on lateromedial radiographs.20 Lateral patellar luxation is an uncommon congenital condition and may be unilateral or bilateral.25 Lateral patellar luxation is often the consequence of femoral trochlear dysplasia with trochlear ridge hypoplasia and a shallow trochlear groove. Lateral patellar luxation may be associated with incomplete ossification of the medial patellar angle.25 Patellar luxation is recognized in horses of all ages as a cause of a nonpainful gait alteration, more commonly in miniature breeds and ponies.20,25 Radiographically, lateral patellar luxation is seen as a malpositioning of the patella (Fig. 19-6). An increase in the craniocaudal dimension of the patella on the lateromedial view of the stifle is caused by displacement and rotation of the patella compared with the normal axis of the limb. Chronic osteomyelitis of the patella may develop as a consequence of a chronic abscess at the cranial aspect of the stifle.20 A cranioproximal-craniodistal view of the patella is essential to assess the full extent of involvement (Fig. 19-7). Radiographic signs are periosteal reaction on the cranial patellar surface and areas of reduced opacity within the patella, resulting in a patchy heterogeneous appearance of the patella (see Fig. 19-7). Ultrasonography can help assess concurrent soft tissue infection, localize the abscess, and confirm bony involvement seen as roughening of the bone surface. Subchondral cystlike lesions of the stifle are juvenile osteoarticular abnormalities but may be seen in horses of any age.10 Their typical radiographic appearance is a round to oval radiolucent area with well-defined margins within the subchondral bone of the femoral condyles (Fig. 19-8) or, less commonly, the tibial condyles. Subchondral bone cysts may have a distal base of variable extent depending on communication and proximity with the joint space; they may also be surrounded by a sclerotic rim. The subchondral surface of the femoral condyle is flattened at the level of the cyst. Small bone cysts may be difficult to see within the thick femoral condyle, especially in large horses. Flattening or indentation of the femoral subchondral surface may be the only radiographic sign in some horses.26 Trauma to the medial femorotibial joint may also lead to subchondral bone damage of the medial femoral condyle and induce a radiographically visible radiolucent subchondral cystlike lesion as synovial fluid is pumped into the subchondral bone.10 Ultrasonography of the femoral condyle surface in the flexed stifle may be used to confirm radiographic suspicion13 or to evaluate cartilage and subchondral defects better in horses with subtle radiographic changes. Radiographic signs of degenerative joint disease may be present in older horses with a cystlike lesion as a result of chronic synovitis and secondary meniscal damage (Fig. 19-8, A and B). The most common location for subchondral cystlike lesions is the weight-bearing area of the medial femoral condyle.20,27 In the caudocranial view, these cystlike lesions affect the central portion of the medial condyle most commonly, but they can also be encountered in the more axial aspect of the medial femoral condyle (Fig. 19-8, C). Osseous cystlike lesions have also been reported in the caudal aspect of either femoral condyle in foals.28 This unusual location may be related to a septic origin. Lateral femoral condyle and proximal tibial cystlike lesions are less common (Fig. 19-8, D).20,29 Subchondral cystlike lesions may be difficult to see on slightly underexposed lateromedial radiographs because of superimposition of the femoral condyles. A caudocranial view of optimal exposure and contrast and/or a caudolateral-craniomedial view are the most useful for confirming and localizing the lesion. Degenerative joint disease of the femorotibial joint can be a sequel to any stifle injury and is seen commonly in horses with stifle lameness and meniscal damage.5,7 Involvement of the medial femorotibial joint is more common than involvement of the lateral compartment.5,20 The most common radiographic signs are remodeling of the tibial and femoral joint margins with production of large-based osteophytes (Fig.19-9; see Fig. 19-8, A and B). Tibial osteophytes are usually large with smooth margins and tend to form such that their proximal surface is not in the same plane as the tibial plateau. Femoral osteophytes are seen more commonly on the medial condyle margin. They are usually large-based and, as tibial osteophytes, their distal surface is not in continuity with the arc of the condylar surface (see Fig. 19-9). Narrowing of the femorotibial joint space is less common and is a sign of meniscal prolapse more than a consequence of cartilage thinning in degenerative joint disease (Fig. 19-10). Narrowing of the femorotibial joint space because of marked articular cartilage degeneration is observed only rarely; one instance is following repeated injections of long-acting steroids.30 Areas of subchondral bone sclerosis and lucencies are mainly seen in advanced articular damage with meniscal injury and prolapse (see Fig. 19-10). The menisci, which are of soft tissue opacity, occupy, with the articular cartilage, the space between the distal femoral condyles and the proximal tibial plateau. The menisci cannot be seen radiographically. Therefore meniscal damage can only be suspected when calcification is present in the femorotibial joint space or close to it (Fig. 19-11), or on the basis of secondary bony abnormalities, such as radiolucent areas (see Fig. 19-9, C), new bone formation, or avulsion fragments at the site of insertion of the cranial meniscal ligaments on the proximal tibia (Fig. 19-12, see page 358).5 New bone formation cranial to the medial intercondylar eminence of the tibia has been reported as the most frequent radiographic finding in horses with meniscal damage diagnosed using arthroscopy (Fig. 19-13, see page 358).5 The imaging technique of choice to evaluate meniscal and meniscal ligament damage is ultrasonography (see Fig. 19-2). When the site of pain responsible for the lameness has been proved to be the stifle, or when distention of the femorotibial joint is present, a radiographically normal stifle should not be considered normal anatomically because soft tissue injuries, in particular meniscal damage, are a frequent cause of lameness.6,7 Indirect radiographic signs of cruciate ligament damage are seen as radiolucent areas at the ligament insertion sites on the distal femur or bone remodeling at the tibial insertions (Fig. 19-14). In chronic damage, there can be mineralization of the injured ligament.5 Avulsion of bone at the femoral and tibial cruciate ligament insertions has also been reported.31–34 Fractures of the medial intercondylar eminence (see Fig. 19-14, p. 358) are described most commonly in association with cranial cruciate ligament damage and have been suggested to be caused by lateral pressure of the medial condyle more than avulsion.5 Collateral ligament damage of the stifle as a consequence of acute trauma does not result in any radiographic abnormality except joint swelling. In acute complete traumatic collateral ligament rupture, joint instability can be assessed using a caudocranial projection with the stifle under stress.6 Ultrasonography allows assessment of the medial and lateral collateral ligaments (see Fig. 19-2, B). Chronic enthesopathy may be visible on caudocranial radiographic views as a change in shape or an increased irregularity of the surface of the medial or lateral femoral epicondyles. Patellar fractures involve the medial angle of the patella most commonly.35,36 These fractures occur mainly in steeplechase and eventing horses when the flexed joint strikes a fixed fence.35,36 Fractures of the medial angle may be incidental and not related to lameness. These fractures may be suspected on the lateromedial view because of an area of heterogeneously increased opacity in medial patellar angle (Fig. 19-15, p. 359). A cranioproximal-craniodistal view of the stifle allows confirmation of the diagnosis and a complete assessment of the extent and morphologic features of the fracture. Patellar fracture may be associated with fractures of the trochlear ridges of the femur.20 Ultrasonographic examination adds valuable information in patellar fractures by documenting associated soft tissue injuries and defining the anatomic origin of avulsed fragments; that is, parapatellar fibrocartilages, patellar ligaments, and distal enthesis of the quadriceps femoris muscle. Fractures of the tibial tuberosity are the most commonly reported fractures involving the proximal tibia in adult horses.20,37 Fractures involving the intercondylar eminence or the caudal aspect of the proximal tibia are seen in association with cruciate ligament damage and often involve the ligament insertion sites.31–34
The Equine Stifle and Tarsus
The Stifle
Radiographic Examination
Ultrasonography for Supplemental Stifle Imaging
Diseases of the Femoropatellar Joint
Osteochondrosis
Patellar Fragmentation
Upward Patellar Fixation
Patellar Luxation and Trochlear Dysplasia
Osteomyelitis of the Patella
Diseases of the Femorotibial Joints
Subchondral Cystlike Lesions
Degenerative Joint Disease
Radiographic Signs of Meniscal and Meniscal Ligament Damage
Radiographic Signs of Cruciate Ligament and Collateral Ligament Damage
Fractures Involving the Stifle
Patellar Fractures
Tibial and Femoral Fractures
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Equine Stifle and Tarsus