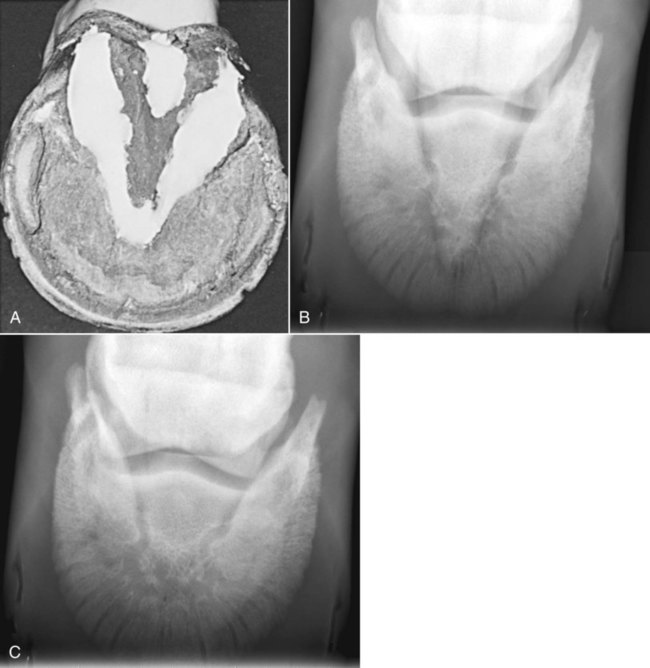
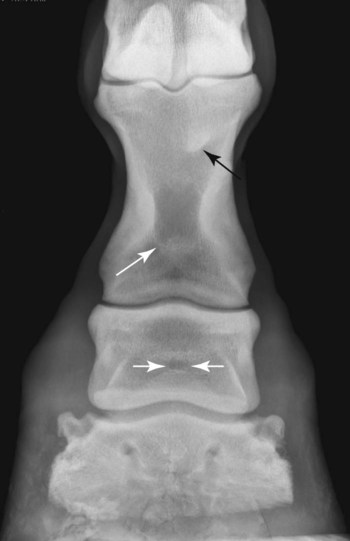
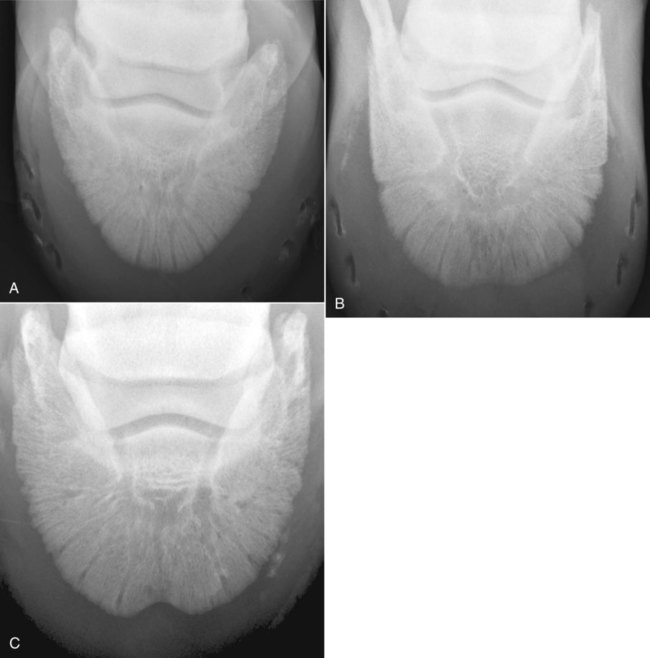
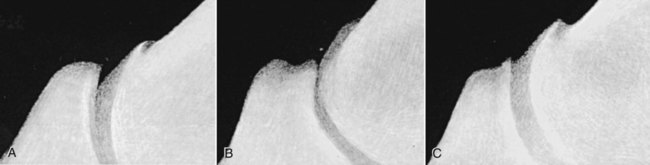
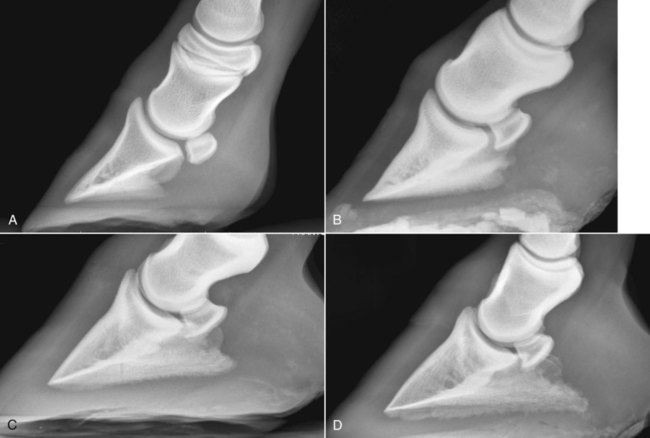
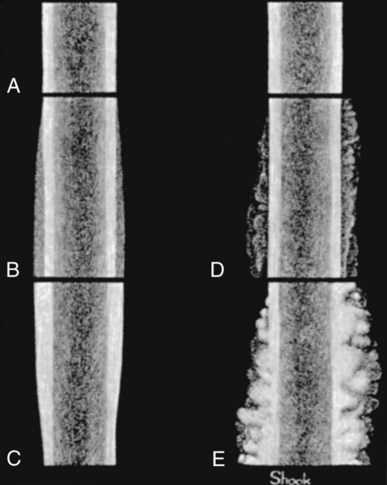
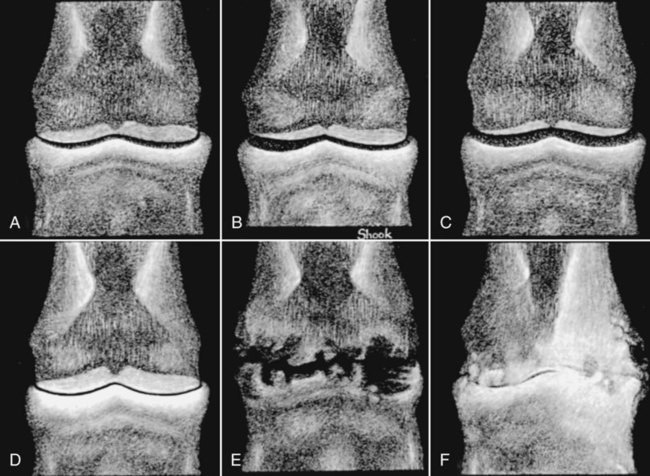
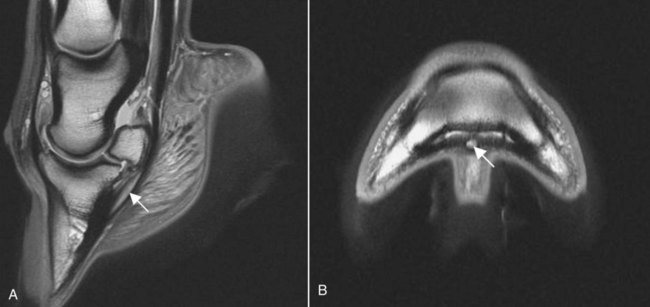
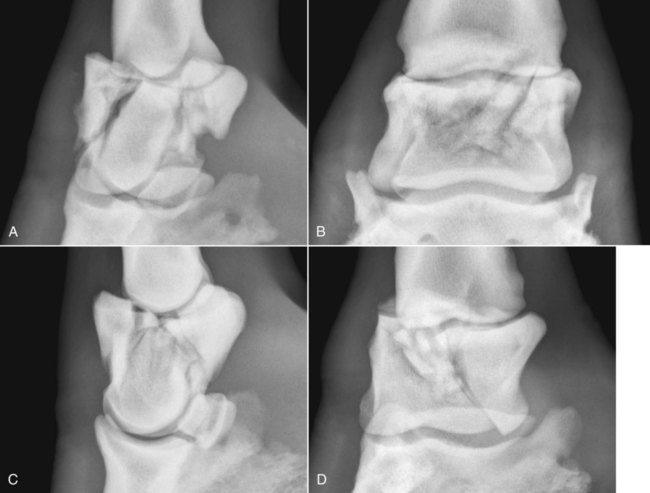
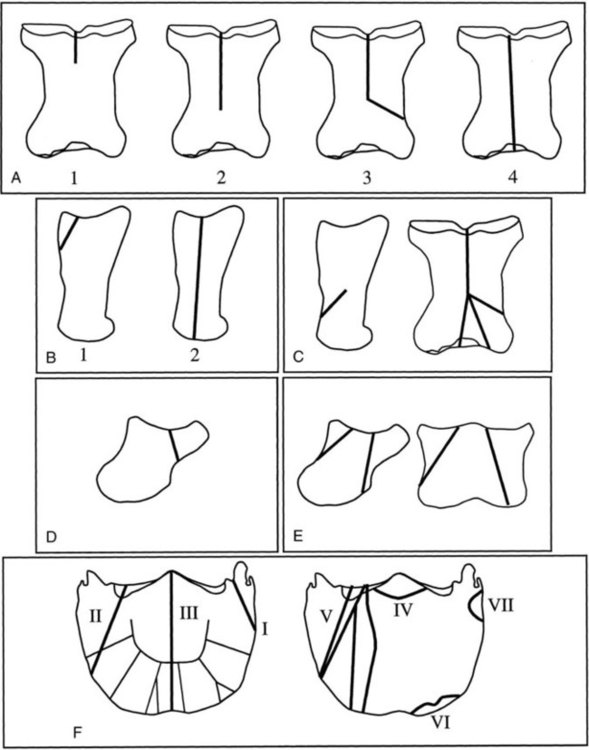
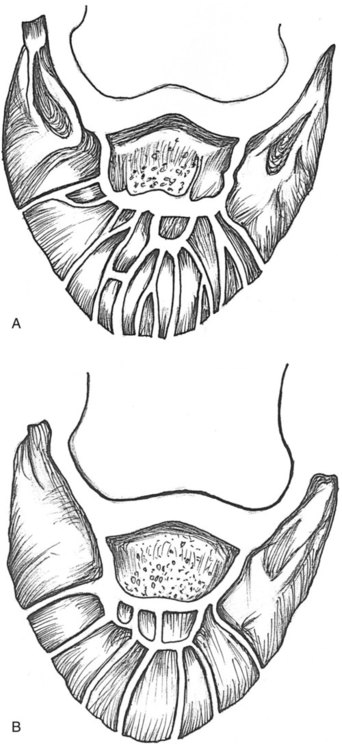
The significance of many radiographic abnormalities of the equine phalanges is difficult to ascertain unless pertinent facts obtained from the history and physical examination, including results of diagnostic nerve blocks, are correlated with the radiographic findings. Dirt, skin lesions, and iodine-containing medications can all produce opacities that complicate radiographic interpretation. All such material should be removed from the hair coat and hoof wall. Shoes and any additional pads should be removed so that optimal radiographs of the distal phalanx can be obtained. The sole and sulci of the frog should be cleaned thoroughly. The sulci may then be filled uniformly with a material of soft tissue opacity (such as Play-Doh, Hasbro, Pawtucket, RI) to the level of the solar surface (Fig. 23-1). Packing the central and collateral sulci eliminates radiolucent linear regions created when the air-filled sulci are superimposed on the distal phalanx in the dorsal 65-degree proximal-palmarodistal* view (see Fig. 23-1). The equine foot is structured such that certain anatomic areas can be imaged as a group (Table 23-1). Excellent descriptions of positioning are available for additional information.1,2 Table • 23-1 Views for Equine Phalanx Evaluation Normal radiographic anatomy of the digit is illustrated in Chapter 13 and other published sources.3–5 However, several anatomic variations that are misinterpreted frequently as abnormal are worthy of mention.6 A nutrient foramen occurs in the proximal phalanx of approximately 87% of Thoroughbreds and Standardbreds that are at least 1 year of age.7,8 When present, these foramina are sometimes symmetric bilaterally and can be located in either the palmar or dorsal cortex. No horses were identified in those surveys to have both a dorsal and a palmar nutrient foramen, although both were present occasionally in foals. When in the dorsal cortex, the foramen is typically seen in a lateromedial view as a radiolucent line running obliquely proximal to distal through the mid-diaphyseal cortex (Fig. 23-2). In a dorsopalmar view, the nutrient foramen appears as a thin lucent line within the medullary region. When in the palmar cortex, the foramen is located in the distal third and courses in a shorter oblique-to-transverse direction. Of greatest importance is that these foramina should not be mistaken for fractures. Variability in the location of the nutrient foramen of the hindlimb proximal phalanx has not been reported. Variations have not been reported in other breeds, but they likely occur. Variations may also occur in the appearance of trabeculae in the medullary cavity of the proximal phalanx. A conspicuous radiolucent center in the medullary cavity surrounded by a ringlike radiopacity is a normal variation and does not indicate cyst formation (Fig. 23-3). The radiographic appearance of the normal distal phalanx in the dorsal 65-degree proximal-palmarodistal view varies in several respects.2,9,9 The most obvious is the number and distribution of vascular channels (Fig. 23-4). The number of vascular channels is typically greater in the rear distal phalanx than in the front distal phalanx (ranges of 9 to 19 and 5 to 16, respectively).9 All vascular channels radiate from the solar canal to the solar border. On their path to the periphery, some give rise to secondary branches that reach the solar border. Although this branching pattern is unique to individual animals, the major channels identified at the solar margin should communicate with the solar canal. A smoothly rounded concavity in the toe of the distal phalanx may be present in the normal horse (Fig. 23-5). This notch is referred to as the crena margins solaris or, more commonly, the crena or toe notch. In a radiographic study of the foredigit of the developing quarter horse, a crena was identified in foals between 4 and 22 weeks of age in 83% of the distal phalanges evaluated.11 The depth of this notch usually does not exceed 1.5 cm.2 The crena is more conspicuous in front than in hind feet.10 Ninety percent of sound racing Thoroughbreds have bilateral symmetry in the presence of the crena in the front feet, 5% asymmetry in the front feet, and 5% in neither front foot.10 The shape of the extensor process of the distal phalanx may also differ among individual animals (Fig. 23-6).9 The margin of the normal process, however, should be smooth regardless of its shape. The palmar processes of the distal phalanx become ossified more extensively with age (Fig. 23-7). The morphologic development of the palmar process has been described in the foal (3 to 32 weeks of age).12 No muscle exists in the phalangeal region of the foot. Many tendons and supporting ligaments, however, are present in addition to joint capsules. Minimal amounts of fat are present in the phalangeal region. Knowledge of the attachment sites of the joint capsules, tendons, and ligaments of the foot is imperative for accurate interpretation of the osseous changes seen in radiographs. Figures 23-8 and 23-9 illustrate the attachment sites of these major structures. A clinical anatomic atlas presents these soft tissue bone relationships through side-by-side comparisons of anatomic sections, prepared in the scan planes of magnetic resonance (MR) imaging, with radiographs, ultrasound, and MR images.5 Most of these soft tissues do not create independently distinct shadows. However, the deep digital flexor tendon can often be seen in the lateromedial view as a slightly more opaque soft tissue band as it passes between the level of the proximal aspect of the middle phalanx and the proximal margin of the navicular bone.9 This is more evident in digital than in analog radiographs (see Fig. 23-7). The hoof capsule produces soft tissue opacity. However, the junction between the outer denser portion (stratum medium) and the inner highly vascularized portion (the stratum internum plus the corium) is well defined in digital radiographs and also visible in optimally exposed analog radiographs.10 The inner portion is less radiopaque (see Fig. 23-7). The junction of the coronary band and the most proximal extent of the hoof wall is not always clearly distinct in lateromedial and dorsopalmar views. The ergot may create a radiopacity when superimposed on the proximal phalanx in the dorsopalmar view (see Fig. 23-3). In the lateromedial view, the ergot can be seen along the palmar surface of the skin. The properly positioned dorsal 45-degree proximal-palmarodistal view is the best for evaluation of the width of the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints. In the normal foot, the metacarpophalangeal joint is usually the narrowest of these articulations, the proximal interphalangeal joint is slightly wider, and the distal interphalangeal joint is the widest (see Fig. 23-3). If the horse is not bearing weight evenly on the leg, the asymmetric loading forces can cause the appearance of narrowing of the loaded side and widening of the nonloaded side of the joint. This artifact can be recognized because it affects all three joints similarly. The collateral cartilages are not visible in the normal foot, and ossification of these cartilages is usually not significant clinically. Because the digit has little soft tissue, x-ray exposure technique for analog radiography is typically selected to best define the bony structures. Supplemental views altering the exposure to demonstrate the soft tissue may be needed. The postcapture image manipulation offered by digital radiography allows evaluation of osseous and soft tissue structures with one exposure per view (Fig. 23-10). Increased opacity within pericapsular soft tissue is usually caused by dystrophic mineralization. Lesions that commonly become mineralized include chronic sprain or strain of supporting ligaments and tendons (Fig. 23-11), pericapsular deposition of corticosteroids, and focal necrosis attributable to neurectomy. Ossification of the collateral cartilages of the distal phalanx should not be mistaken for dystrophic mineralization of soft tissue. The radiographic signs of abnormal bone include alteration of contour, margination, and opacity. These signs are caused by a combination of new bone formation and bone removal. Repeated patterns of bone change tend to be associated with specific injury to the phalanges and associated joints. Figures 23-12 and 23-13 depict the variable appearances of the periosteal surface, joint space, and subchondral bone that occur in the more common diseases of the phalanges. Regions of new bone formation are commonly seen on the cortical surfaces of the phalanges, especially in the proximal and middle phalanx. Many of these are caused by strain and sprain injuries. Strain injury (tendonitis) results from damage to muscle or tendon induced by overuse or overstress. In its mildest form, strain causes only inflammation. With chronic repeated strain or more severe acute strain, disruption within the soft tissue unit or avulsion from its bone attachment occurs. Radiographically, the swelling or inflammation in the tendon may not be evident. Soft tissue changes are best imaged by ultrasound, vascular and soft tissue pool phase scintigraphy, and MR imaging. The latter has become the imaging modality of choice when lameness is persistent and the other modalities have negative or equivocal findings (Fig. 23-14).13,14 Although uncommon, dystrophic mineralization can develop in a chronically inflamed tendon (see Fig. 23-11). Radiography is useful for assessing the bony attachment sites of the tendons. Knowledge of the attachment sites of the flexor and extensor tendons on the phalanges is therefore needed (see Figs. 23-8 and 23-9). Avulsion fracture at the attachment site can occur and will be evident as a bone fragment displaced in the direction of traction of the tendon. Enthesophyte formation indicates a response to stress at the ligament or tendon attachment site. When seen early, it will likely be minimal in volume and have a mildly irregular surface. If the strain injury continues, the enthesopathy enlarges and continues to have a fuzzy, irregular margin. Such a change is seen occasionally at the insertion of the lateral digital extensor tendon on the dorsolateral proximal surface of the proximal phalanx. With further progression, the enthesopathy takes on a smooth, hooklike, or spurlike shape, projecting in the direction of tension or traction. Radiographically aging or determining the activity of these bone changes is difficult. Periosteal new bone formation is typically not visible until 5 to 7 days (in the foal) or 10 to 14 days (in the adult) after stimulation. When a prominent smooth enthesophyte is seen on a first radiographic evaluation of a horse, it should be taken as a signal of strain injury that occurred at least 5 to 6 weeks previously. Stress views may be needed to detect subluxation. Laxity in a subluxated joint is often more apparent at physical examination than at radiography, especially if the horse is unwilling to bear full weight on the leg. Conversely, complete luxation is typically evident and may be accompanied by avulsion fractures at the ligament insertion sites. Non–weight-bearing flexed dorsal 45-degree lateral-palmaromedial and flexed dorsal 45-degree medial-palmarolateral views may improve the visualization of the origin and insertion sites for the collateral ligaments of the distal interphalangeal joint.2 Larger fractures of the phalanges may also be associated with joint luxation. This is commonly seen with comminuted fractures of the middle phalanx and associated loss of congruency of the proximal interphalangeal joint (Fig. 23-15). Secondary changes expected with subluxation are enthesophyte formation at the ligament insertion sites and some degree of degenerative joint disease. The range of change will depend on the severity of the initial injury and the frequency of recurring subluxation. Although not the result of overt joint instability, a common site of enthesophyte formation associated with ligament insertion is on the palmar or plantar margin of the proximal phalanx at the insertion of the middle (oblique) sesamoidean ligament (see Fig. 23-11). Most enthesophytes do not regress after healing of the soft tissues involved in the inciting sprain or strain injury. Collateral ligament desmitis of the distal interphalangeal joint is a significant cause of foot lameness in the absence of radiographic changes. MR imaging is the most useful imaging modality to define the changes in these ligaments (Fig. 23-16).15,16 Most of the lesions are associated with the insertion of the ligament on the distal phalanx, and the medial collateral ligament is affected more often than the lateral ligament. The most frequent type of bone lesion is new bone formation and endosteal irregularity at the middle phalanx origin or distal phalanx insertion. Osseous cystlike lesions are found occasionally at either site. Similarly, evaluation of the straight and oblique sesamoidean ligaments by MR imaging allows identification of lesions not detected by radiography or ultrasound.17 The location of fractures of the proximal phalanx depends on the type of stress applied. The common fracture types are osteochondral edge (chip) fractures at the proximal dorsal periarticular margin and the palmar or plantar proximal tuberosity and longitudinal fractures of the diaphysis.18,19 The most common fracture involving the proximal phalanx is the osteochondral fracture of the proximal dorsal edge, either at the medial or at the lateral eminence. This occurs as an overextension injury of the metacarpophalangeal joint in racehorses. This fracture and those of the palmar eminence are described in Chapter 22. Various classification schemes have been applied to all other fractures of the proximal phalanx.20 By general classification, the fractures are noncomminuted or comminuted, incomplete or complete, monoarticular or biarticular, and in a primarily sagittal or dorsal plane to the long axis of the proximal phalanx. Figure 23-17 illustrates these fractures of the proximal phalanx. The most frequently reported fracture configuration in Thoroughbreds and Standardbreds is the noncomminuted, incomplete, monoarticular sagittal fracture (Fig. 23-17, A).21,22 This fracture is common in 2- and 3-year-old horses in race training or active racing. It occurs in the front limbs and hindlimbs of these breeds. However, fractures are somewhat more common in the front limbs of Thoroughbreds and the hindlimbs of Standardbreds. This fracture typically originates at the proximal articular surface just lateral to or within the midline plane of the sagittal groove (Fig. 23-18). Few originate medial to the midline plane. Two variations of the noncomminuted, incomplete, monoarticular sagittal fracture occur. The short (less than 30 mm extension into the diaphysis) variation is slightly more common than the long (more than 30 mm extension into the diaphysis) variation. Both fractures may course in a slightly spiral or oblique manner. This effect is depicted as two parallel or offset radiolucent lines representing the fracture plane in the dorsal and palmar cortices. The short fracture may be more difficult to identify on an initial radiographic evaluation. Both variations of fracture are seen only on dorsopalmar views. Because the fracture plane typically has very little gap, the x-ray beam must pass parallel to the fracture line for the fracture gap to be detected. Repeat radiographs in 7 to 10 days should allow identification of the fracture more readily, after lysis of bone along the fracture edges has occurred during the first stages of healing. When imaging occurs several weeks after the onset of lameness, periosteal new bone will likely be present on the dorsal or palmar surface, indicating callus. At this stage, the new bone is visible on the lateromedial view, the fracture line may be less visible on the dorsopalmar view, and sclerosis in the adjoining bone should be seen. In the nonathletic horse that may have been managed conservatively for several months, an osseous cystlike lesion may also be present.23 This type of fracture is not mentioned in a report of diagnosis and treatment of quarter horse racehorses.24 This fracture is generally presumed to occur subsequent to a single force incurred during exercise. Lame horses with this fracture but without radiographic lesions can have intense increased radiopharmaceutical uptake and MR imaging changes consistent with bone marrow edema and subchondral sclerosis extending a short distance from the sagittal groove. It is speculated that these changes indicate a prodromal stage of proximal phalanx fracture caused by repetitive trauma.25 Noncomminuted, complete sagittal fractures of the proximal phalanx occur with less frequency than do incomplete fractures in racehorses. This type of fracture is, however, reported to be more common in the Western performance horse. Two variations of this fracture occur: One is biarticular with origin at the metacarpophalangeal joint and exit at the proximal interphalangeal joint; the other is monoarticular and typically exits through the lateral distal palmar or plantar cortex (see Fig. 23-17, A). These fractures are most readily seen in the dorsopalmar view. Comminuted fractures of the proximal phalanx (Fig. 23-17, C) are moderately common. Variations include comminution throughout the phalanx, only in the proximal portion, or only in the distal portion. These fractures frequently have one exit through the lateral rather than the medial cortex and are typically biarticular and more likely to be complicated by being open. The multiple fracture planes of the comminuted fracture are visible in both lateromedial and dorsopalmar views. Oblique views should also be made to obtain a more thorough depiction of the fracture configuration. Comminuted fractures have the most guarded prognosis for survival and very poor prognosis for return to athletic performance. Incomplete or complete dorsal plane fractures that originate at the proximal articular surface (Fig. 23-17, B) are much less common. These fractures may be detected only on lateromedial views. The incomplete fracture typically courses distally toward the dorsal cortex. The complete variation either breaks through the dorsal cortex or extends the entire length of the phalanx to exit in the proximal interphalangeal joint. The latter variation typically splits the proximal phalanx into roughly equal dorsal and palmar (plantar) halves. Other sporadically reported fractures of the proximal phalanx include physeal fractures (typically Salter-Harris type II) and incomplete distal articular fractures.21,22 Fractures of the middle phalanx include comminuted fracture (most common) (see Fig. 23-15), fracture of the plantar or palmar proximal eminence (fracture of both medial and lateral eminences is more common than a single eminence fracture) (Fig. 23-19), and osteochondral edge fracture (rare) (Fig. 23-17, D and E). Physeal fracture can occur in the skeletally immature horse but is reported infrequently. The comminuted (complete and typically biarticular) and eminence fractures (complete monoarticular) are most common in horses whose activity subjects the middle phalanx to extreme simultaneous compression and torsion forces while the foot is fixed to the ground.26 Thus these types of fractures are most common in working or performing Western horses, polo ponies, and jumpers. For both common fractures, the hindlimbs are involved approximately twice as frequently as the front limbs.21,22,22
The Equine Phalanges
Technical Factors
Patient Preparation
Recommended Views
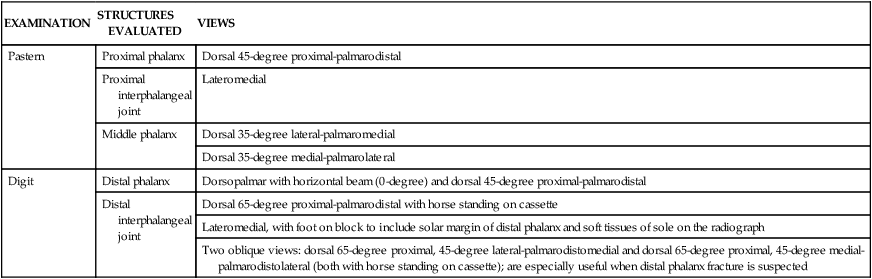
EXAMINATION
STRUCTURES EVALUATED
VIEWS
Pastern
Proximal phalanx
Dorsal 45-degree proximal-palmarodistal
Proximal interphalangeal joint
Lateromedial
Middle phalanx
Dorsal 35-degree lateral-palmaromedial
Dorsal 35-degree medial-palmarolateral
Digit
Distal phalanx
Dorsopalmar with horizontal beam (0-degree) and dorsal 45-degree proximal-palmarodistal
Distal interphalangeal joint
Dorsal 65-degree proximal-palmarodistal with horse standing on cassette
Lateromedial, with foot on block to include solar margin of distal phalanx and soft tissues of sole on the radiograph
Two oblique views: dorsal 65-degree proximal, 45-degree lateral-palmarodistomedial and dorsal 65-degree proximal, 45-degree medial-palmarodistolateral (both with horse standing on cassette); are especially useful when distal phalanx fracture is suspected
Normal Radiographic Anatomy (Including Variations)
Osseous Structures
Soft Tissue
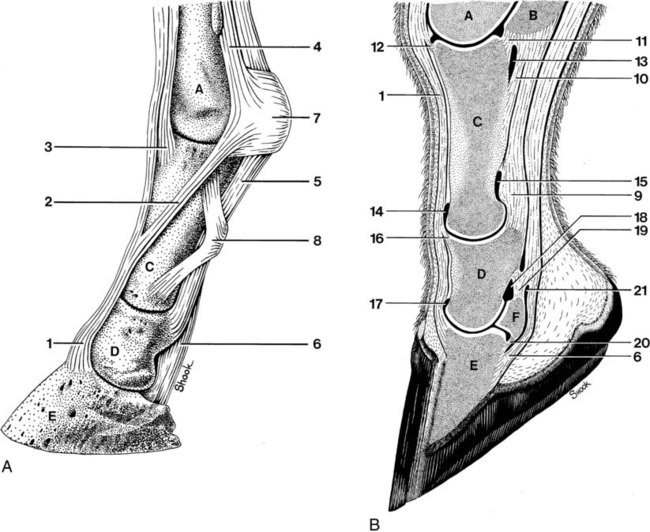
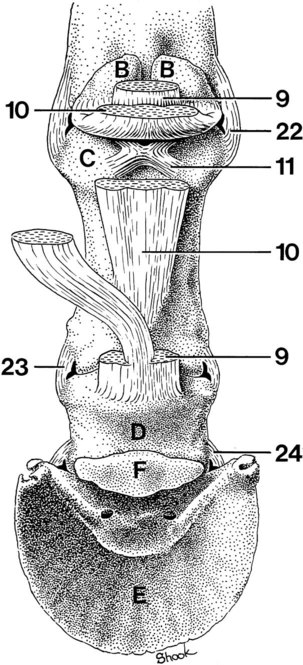
(Illustration by Richard A. Shook, DVM.)
The following anatomic key is for Figures 23-8 and 23-9.
A. Third metacarpal bone
B. Proximal sesamoid bone
C. Proximal phalanx
D. Middle phalanx
E. Distal phalanx
F. Distal sesamoid (navicular) bone
1. Common digital extensor tendon
2. Extensor branch of the interosseous (suspensory) ligament
3. Lateral digital extensor tendon
4. Interosseous (suspensory) ligament
5. Superficial digital flexor tendon
6. Deep digital flexor tendon
7. Superficial transverse metacarpal ligament (palmar annular ligament)
8. Proximal digital annular ligament
9. Superficial (straight) sesamoidean ligament
10. Middle (oblique) sesamoidean ligament
11. Deep (cruciate) sesamoidean ligament
12. Metacarpophalangeal joint capsule (blended with fibers from the common digital extensor tendon)
13. Distal palmar recess of the metacarpophalangeal joint
14. Dorsal recess of the proximal interphalangeal joint capsule
15. Palmar recess of the proximal interphalangeal joint
16. Proximal interphalangeal joint capsule (blended with fibers from the common digital extensor tendon)
17. Dorsal recess of the distal interphalangeal joint
18. Palmar recess of the distal interphalangeal joint
19. Collateral sesamoidean ligament
20. Distal sesamoidean impar ligament
21. Podotrochlear bursa
22. Medial collateral ligament of the metacarpophalangeal joint
23. Lateral collateral ligament of the proximal interphalangeal joint
24. Medial collateral ligament of the distal interphalangeal joint
Articular Cartilage and Collateral Cartilages
Radiographic Changes Caused By Diseases of the Phalanges
General Comments

Strain and Sprain Injuries
Fracture Disease
Proximal Phalanx
Middle Phalanx
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Equine Phalanges