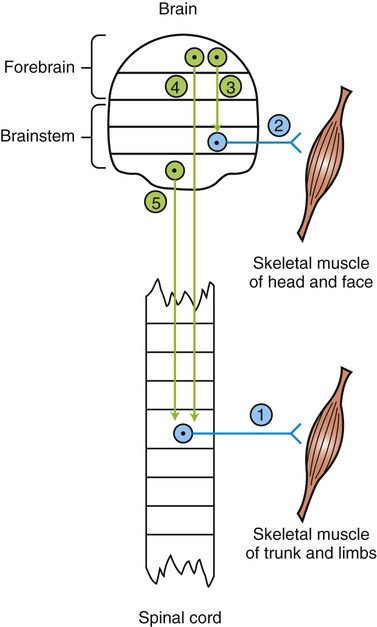
1. The lower motor neuron is classically defined as the alpha (α) motor neuron. 2. Disease of lower motor neurons causes stereotypical clinical signs. 3. Upper motor neurons lie completely in the central nervous system and control lower motor neurons. 4. Signs of upper motor neuron disease differ from signs of lower motor neuron disease. The concept of a lower motor neuron is decades old in neurology. The alpha (α) motor neuron is classically defined as a neuron whose cell body and dendrites are located in the central nervous system (CNS) and whose axon extends out through the peripheral nerves to synapse with the extrafusal skeletal muscle fibers (Figure 9-1). The cell bodies of these neurons are located either in the ventral horn of spinal cord gray matter or in cranial nerve nuclei of the brainstem. This is the “final common path” through which CNS commands to a skeletal muscle are channeled to produce movement. This definition predates the discovery of gamma (γ) motor neurons, which innervate muscle spindles. Some authors would include γ motor neurons in the definition of lower motor neurons. Some also consider the pre- and post-ganglionic autonomic neurons to be lower motor neurons (see Chapter 13). The vast majority of clinical signs caused by lower motor neuron disease, however, can currently be explained by the loss or malfunction of the α motor neuron. • Paralysis or paresis. Disease of the α motor neurons usually prevents the neurons’ action potentials from reaching the neuromuscular junction. Therefore, despite the brain’s command to the muscle to contract, the message cannot reach the muscle, and paralysis is the result. In fact, such paralysis can be so complete that the adjective flaccid is used to describe the paralysis in which no muscle contraction occurs. Because not all the α motor neuron axons of a peripheral nerve may be affected by an insult, and because muscles can be supplied by axons of more than one spinal nerve, paralysis may be incomplete. This symptom is referred to as paresis. • Atrophy. Atrophy is the shrinking or wasting of skeletal muscle mass distal to the lower motor neuron lesion (Figure 9-2). This occurs within days of the injury to a nerve. The exact origins of this atrophy are controversial. However, evidence indicates that the reduced frequency of muscle stimulation caused by α motor neuron insult, and the resulting reduced use of the muscle, trigger reductions in muscle protein synthesis and increases in muscle proteolysis. There is evidence that activation of the ubiquitin-proteosome proteolytic pathway underlies this muscle breakdown. The magnitude of this denervation atrophy can be reduced by direct electrical stimulation of the muscle itself. There is also some recent evidence that manually imposed repetitive stretching may reduce denervation atrophy; a molecular signaling pathway suspected to underlie this atrophy reduction has been identified. • Loss of segmental and intersegmental reflexes. Segmental and intersegmental reflexes require a viable α motor neuron in the reflex arc for the reflex response to occur (see Chapter 7). Therefore, such reflexes as the muscle stretch (knee jerk) reflex and the toe-pinch withdrawal (nociceptive) reflex, as well as the proprioceptive positioning reaction, fail to occur because the motor neuron portion of the arc that activates the skeletal muscle is gone. • Electromyographic changes. Within a few days of damage to α motor neurons, abnormal electrical activity of the muscle can be observed on an electromyogram (see Chapter 6). Upper motor neurons are the neurons of the CNS that influence the lower motor neurons. They are typically considered the neurons of origin of the corticospinal (cerebral cortex to spinal cord), corticobulbar (cerebral cortex to brainstem), and descending brainstem motor (brainstem to spinal cord; also called bulbospinal) pathways (see Chapter 10). Upper motor neurons send axons down to the spinal cord or into the brainstem to control the lower motor neurons (see Figure 9-1).
The Concept of Lower and Upper Motor Neurons and Their Malfunction
The Lower Motor Neuron Is Classically Defined as the Alpha (α) Motor Neuron
Disease of Lower Motor Neurons Causes Stereotypical Clinical Signs
Upper Motor Neurons Lie Completely in the Central Nervous System and Control Lower Motor Neurons
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree