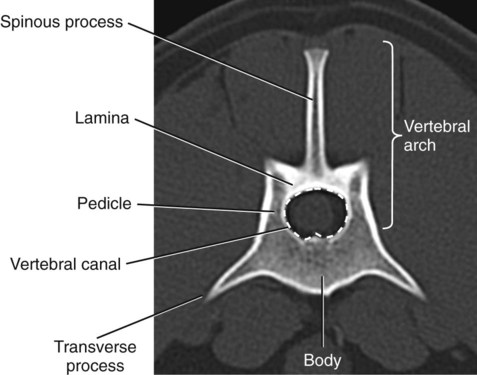
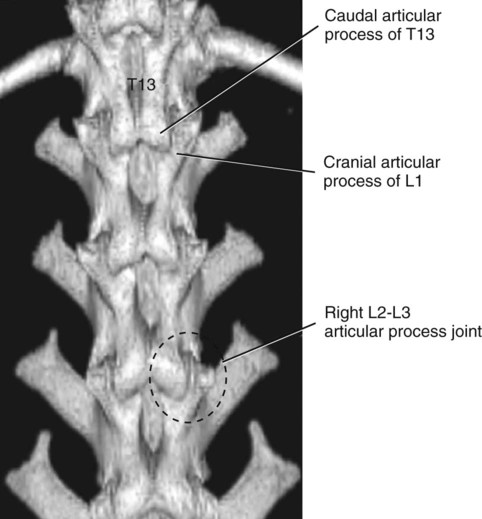
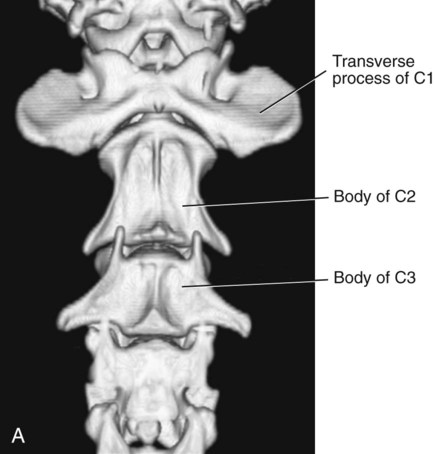
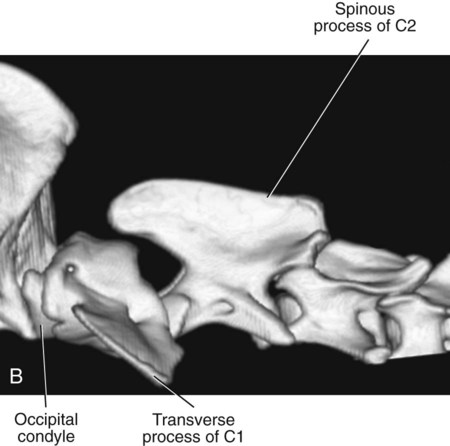
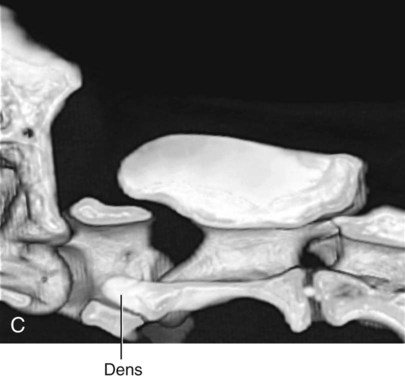
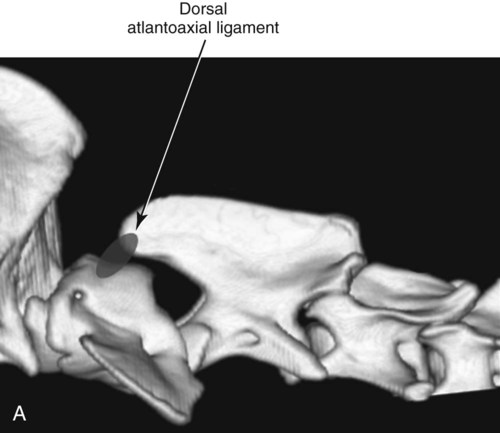
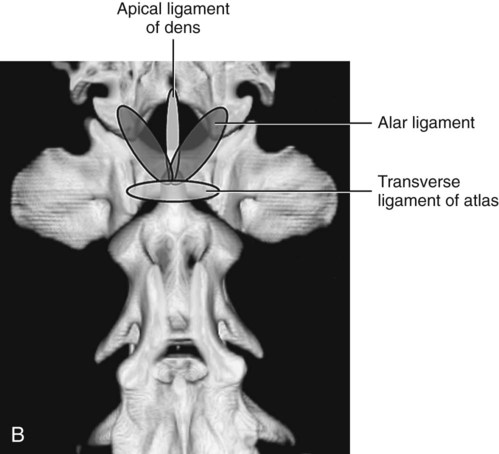
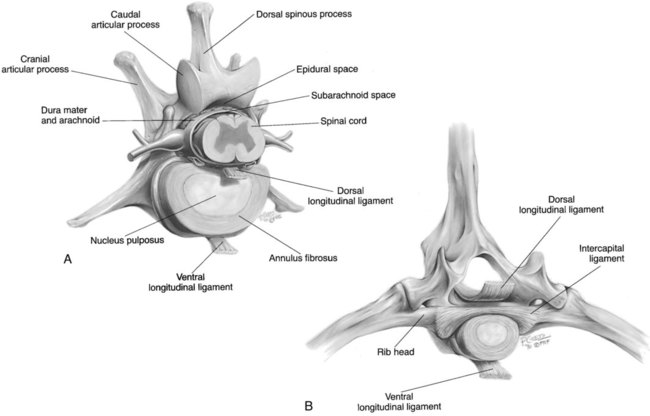
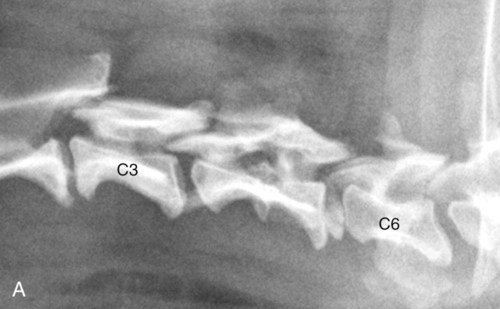
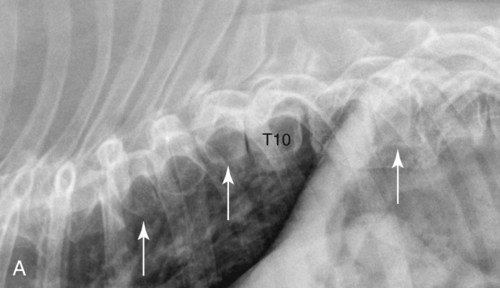
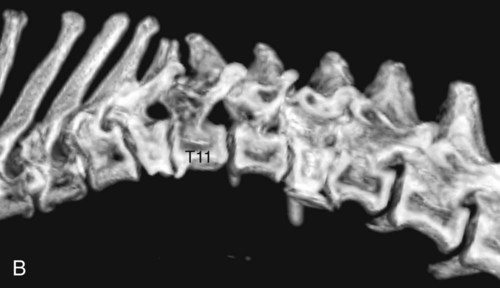
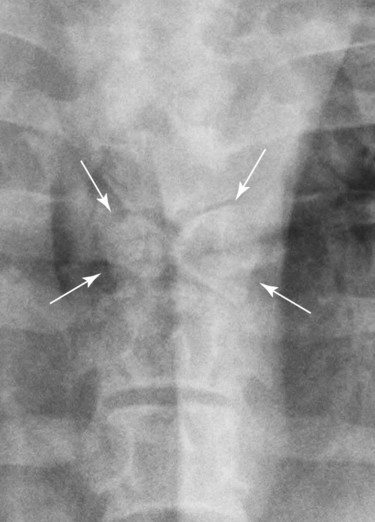
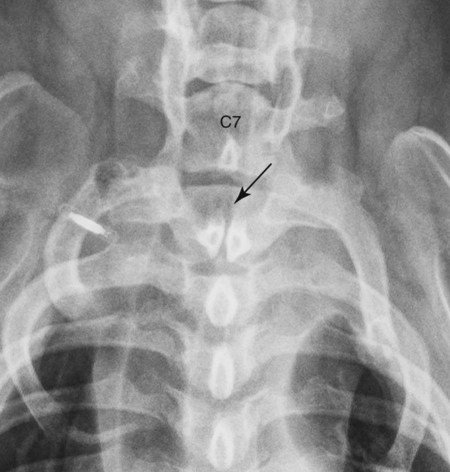
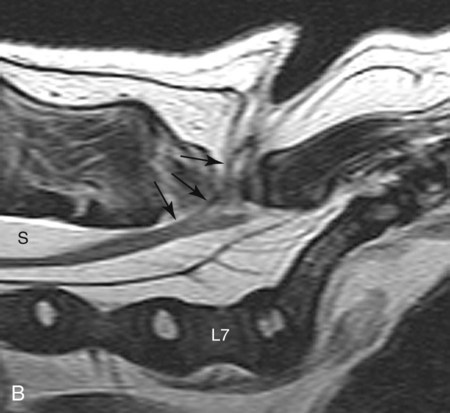
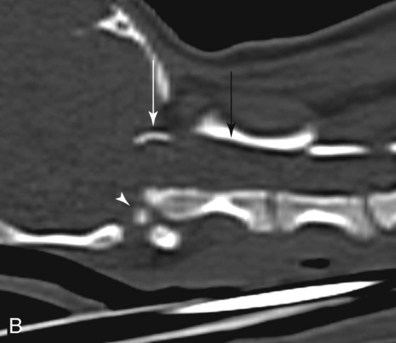
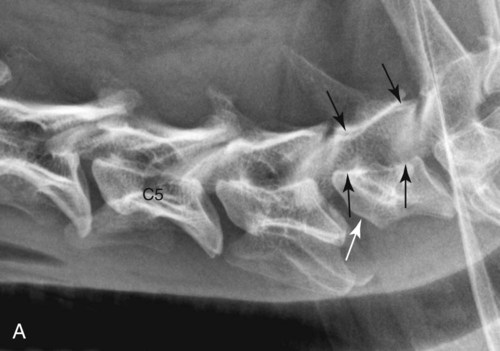
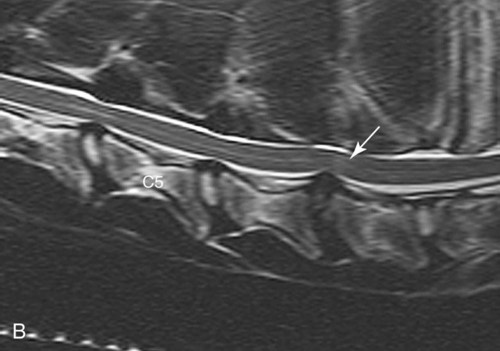
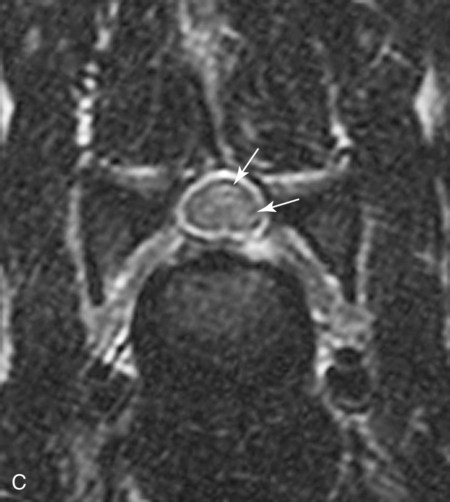
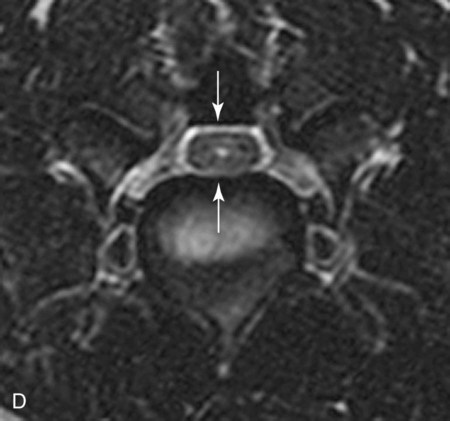
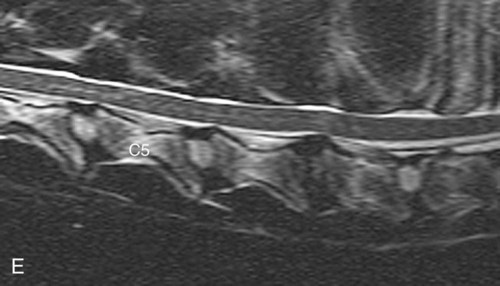
Spinal pain and spinal neuropathy are common problems in small animal practice. This leads to the vertebral column being one of the more frequently imaged anatomic regions. Computed tomography (CT) and magnetic resonance (MR) imaging are the modalities of choice for full characterization of abnormalities of the vertebrae and spinal cord in small animals. Many conditions including intervertebral disc disease; various myelopathies; and tumors of the spinal cord, meninges, and vertebral column cannot be characterized completely using radiography. However, judicious use of conventional radiography can provide valuable, cost-effective information regarding numerous diseases of the vertebral column, and survey radiographs should always be made before advanced imaging. Survey radiographs may or may not lead to identification of the cause of the pain or neuropathy, but, especially in older patients, they are rarely normal. Therefore, it is important to have not only an appreciation for the types of spinal abnormalities that can be diagnosed radiographically but also the significance of commonly encountered changes that may not be related directly to the clinical problem. Therefore, the concept that radiography is no longer useful for vertebral imaging is inaccurate. The focus of this chapter is on vertebral diseases that can be imaged effectively with conventional radiography and the significance of commonly encountered incidental findings. Radiographic abnormalities will be supplemented with CT and/or MR images where appropriate. Advanced imaging related specifically to the spinal cord is covered in Chapter 12. Radiographic technique plays a vital role in radiography of the vertebral column.1 Suboptimal information is obtained frequently when positioning is inaccurate, multiple centered images are not made, and images do not have adequate spatial resolution. Chemical restraint is necessary for accurate positioning and should be employed unless prohibited by the patient’s condition. Technical information relating to spinal radiography is discussed in detail in Chapter 7. A vertebra consists of the body, also referred to as a centrum, and the vertebral arch (Fig. 11-1).1,2 The vertebral arch is composed of paired right and left pedicles and laminae and the unpaired spinous process. The vertebral arch bounds the vertebral canal, which houses the spinal cord. The articular processes of the lamina form the synovial joints along the dorsum of the vertebral column (Fig. 11-2). The articular process joints are diarthrodial (synovial) joints, being composed of articular processes covered with articular cartilage, a synovial membrane, and synovial fluid. They provide dorsal mechanical stabilization of the vertebral column. Other than the first cervical vertebra, each vertebral body is narrowed centrally and has cranial and caudal endplates that unite with an interposed intervertebral disc. The anatomic structure of C1 (atlas) and C2 (axis) is complex and differs widely from the remainder of the vertebra (Fig. 11-3).1–5 C1 has a well-developed vertebral arch, but the body is rudimentary with no distinct vertebral body endplates or spinous process, and the cranial and caudal articular processes are convex. C1 articulates cranially with the occipital condyles, forming the atlantooccipital joint, and caudally with C2, forming the atlantoaxial joint. The wings of C1 are extensive transverse processes that project laterally and serve as attachments for numerous cervical muscles. The lateral and transverse foramina contain the paired vertebral arteries. C2 has an elongated vertebral body and a massive spinous process. The dens is a projection extending cranially from the vertebral body of C2 into the cranioventral aspect of the vertebral canal. The dens originates from the intercentrum of C1, but during development it attaches to C2 and lies within the vertebral foramen of C1. C2 has a small transverse process, two cranial articular processes that articulate with the fovea of the atlas and a caudal endplate. The sacrum is also much different morphologically than a prototypical vertebra. It is broad in the transverse plane, consists of three fused vertebrae and articulates cranially with the seventh lumbar vertebra, caudally with the first caudal vertebra, and laterally with the ilium, forming the sacroiliac joint.1,2 The spinous processes of the sacrum are fused, making up the median sacral crest, and the sacral wing has a large facet for the sacroiliac articulation. Multiple foramina are present dorsally and along the pelvic surface, allowing for passage of spinal nerves and blood vessels. There are 6 to 23 caudal vertebrae in the dog.6 Cranially, the caudal vertebrae are similar to the lumbar elements; caudal to Cd6, they become elongated and lack a vertebral arch. Y-Shaped hemal arches are present ventrally on Cd4-Cd6 and protect the median coccygeal artery, which lies ventral to the vertebral centra. Important soft tissue structures of the vertebral column include various ligaments, intervertebral discs, and the retinaculum of the articular process joints.7 Maintaining stability of the atlantoaxial joint is particularly important given the potential for the dens to damage the spinal cord if displaced dorsally. This stabilization is provided by the short, dorsal atlantoaxial ligament, the apical ligament of the dens with its alar branches, and the transverse ligament of the atlas (Fig. 11-4). The dorsal longitudinal ligament lies on the floor of the vertebral canal and extends from the dens to the sacrum (Fig. 11-5). The intercapital ligaments are short, transverse fibrous bands that lie ventral to the dorsal longitudinal ligament, joining contralateral rib heads between T2 and T11. These ligaments buttress the dorsal part of the annulus cranial to T11 and lead to a reduced incidence of disc herniation between T1 and T11.7,8 The ventral longitudinal ligament is smaller than the dorsal longitudinal ligament and spans the ventral surface of the vertebral column (see Fig. 11-5). The annulus fibrosus of each intervertebral disc has oblique fibers that course from one endplate to the next, serving as ligaments. A detailed description of the intervertebral disc can be found in the online fifth edition version of this chapter (http://evolve.elsevier.com/Thrall/vetrad). A summary of the most important anatomic considerations of the vertebrae relative to radiographic interpretation is provided in Box 11-1.9–10 Anomalies of the vertebral column are common and include congenital and developmental malformations.11–12 Many of these abnormalities are normal variants and have no clinical importance. A block vertebra is the result of fusion of two or more vertebral bodies; the vertebral arches may also be fused, or they may be unaffected (Figs. 11-6 and 11-7).1 The disc space between a block vertebra is often seen radiographically as a thin radiolucent line but may not be visible at all if the fusion is complete. Block vertebrae are most common in the cervical region, but they also occur in the lumbar spine. Biomechanically, block vertebrae may act as a fulcrum, leading to altered loading immediately adjacent to the fusion. This has been hypothesized to increase the risk of disc disease at adjacent sites (see Fig. 11-6) and has also been implicated in leading to atlantoaxial subluxation.13 The fused sacral vertebrae are a normal type of block vertebra. Hemivertebrae are the result of failure of the development and eventual ossification of part of a vertebra, usually the body.1,11,11 The shape of a hemivertebra depends on the area that fails to develop. A wedge-shaped vertebra is seen on the lateral projection when the ventral aspect of the vertebral body is developed incompletely (Fig. 11-8). When this occurs, the vertebral column often develops a kyphotic configuration that can lead to compression of the spinal cord. Not all hemivertebrae are significant clinically, and MR imaging is required to determine if hemivertebrae are the cause of a spinal neuropathy. A butterfly-shaped vertebra occurs when the mid-aspect of the body fails to develop.15 A butterfly vertebra is best seen on the ventrodorsal (VD) projection (Fig. 11-9). Decreased rib spacing on the VD projection is an important clue that hemivertebrae are present (Fig. 11-10). A hemivertebra should not be confused with a compression fracture; their multiplicity and occurrence in a brachycephalic breed are helpful in this distinction. Also, hemivertebrae have a smoothly marginated cortex, whereas vertebrae affected with a compression fracture have a disrupted margin. The bulldog, French bulldog, Boston terrier, and other screw-tail breeds are most affected with hemivertebrae.11,12 Vertebrae that have characteristics of two different anatomic divisions are known as transitional vertebrae.1,11,11 These anomalies usually involve the vertebral arch rather than the body and occur at cervicothoracic, thoracolumbar, and lumbosacral junctions. The main clinical significance of transitional vertebral anomalies relates to the use of the most caudal ribs as a landmark to identify a site of spinal decompressive surgery. If the most caudal ribs are asymmetric, then surgery can be performed at the incorrect site unless the asymmetry is recognized. Another significant feature of transitional anomalies is the increased incidence of lumbosacral disc disease and nerve root compression that occurs in dogs with a lumbosacral transitional malformation.17 This relates to the altered lumbosacral loading that leads to disc degeneration, instability, spondylosis, and nerve root compression. Transitional vertebral anomalies are also discussed and illustrated in Chapter 7. Spina bifida results from the lack of development of the vertebral arch and may be associated with neural tube defects—that is, meningocele or meningomyelocele.1 Typically, there is a cleft in the dorsal part of the vertebral arch and absence or splitting of the spinous process. If the defect in the arch is large, a meningocele or meningomyelocele may develop. The most common radiographic manifestation of spina bifida is a split spinous process (Fig. 11-11). There is rarely a neural tube defect in dogs with spina bifida occurring in the thoracic spine. At the lumbosacral junction, however, the morphologic derangements are often more severe with absent spinous process, laminar defect, and neural tube defect (Fig. 11-12). MR imaging is preferred for characterizing the presence and extent of any neural tube defect (see Fig. 11-12, B). Spina bifida is most common in bulldogs and Manx cats.12,18 In atlantoaxial subluxation, the axis (C2) is displaced dorsally with respect to the atlas (C1), causing compression of the spinal cord. Atlantoaxial subluxation can be a result of either congenital malformation or trauma.12,18,18 With congenital malformation, the dens is often absent,20 and there may be deficiencies in the ligaments that support the atlantoaxial joint and prevent flexion (see Fig. 11-4). The clinical signs may be acute with trauma or chronic with congenital malformation and can be characterized mainly by pain and cervical neuropathy. A variety of lesions may occur in association with atlantoaxial subluxation, and a working knowledge of the components of the atlantoaxial region is needed for radiographic interpretation.1,2 Atlantoaxial subluxation occurs frequently with malformation or rupture of the transverse ligament of the atlas. This ligament bridges the ventral aspect of the vertebral arch and stabilizes the dens, preventing the rostral aspect of the axis from impinging on the spinal cord (see Fig. 11-4, B). A short apical ligament connects the tip of the dens with the occiput along with the alar ligaments (see Fig. 11-4, B). A short, dorsal atlantoaxial ligament is also present dorsally (see Fig. 11-4, A). Atlantoaxial subluxation caused by congenital predisposition is most common in toy breed dogs, such as the Yorkshire terrier, but acquired atlantoaxial subluxation can occur in any breed. Atlantoaxial subluxation is best diagnosed radiographically on a lateral projection of the cranial aspect of the cervical spine. When subluxation is suspected, the patient should be handled carefully, especially when tetraparetic, and the head and neck should not be flexed because this could exacerbate spinal cord damage, especially if the dens is present. On a routine lateral radiograph, the dens is masked by the sheer mass of the atlas. Making a left 15- to 30-degree ventral–right dorsal radiograph will unmask the dens and help identify fractures and malformations of the dens. Even then small fractures may not be apparent. VD projections can also be made, but there is the risk of exacerbating the spinal cord compression, especially in anesthetized patients. The VD projection is not necessary to confirm a diagnosis of atlantoaxial subluxation. Radiographically, the lateral view is the most helpful. If subluxation is present, the axis is displaced dorsally, widening the distance between the vertebral arch of the atlas and the spinous process of the axis. More important, the normal linear relationship between the dorsal lamina of the atlas and the dorsal lamina of the axis becomes angular (Fig. 11-13). This angular relationship between the lamina of C1 and C2 is the most reliable radiographic sign of atlantoaxial subluxation. CT is useful for assessing the morphology of the atlantoaxial junction if surgical stabilization is going to be performed. The additional morphologic information provided in CT images by eliminating the effects of superimposition will be useful when stabilizing such small parts (see Fig. 11-13). Cervical spondylomyelopathy is included under anomalies because anomalous development of vertebrae or anomalous stabilization is likely to play a role in manifestation of clinical signs. Cervical spondylomyelopathy is also best considered a syndrome rather than a specific entity because it encompasses a constellation of pathologic changes that are not seen in every affected animal.18,21–25 Abnormalities include malformation of the vertebral body and articular processes, malarticulation, instability and malalignment, and stenosis of the vertebral canal. Secondary changes involving dorsal longitudinal ligament and ligamentum flavum hypertrophy and disc protrusion and/or herniation are also common. The end result and cause of clinical signs is static or dynamic cervical spinal cord compression. The pathophysiology of canine spondylopathy is complex and understood incompletely.21–23,26 There is debate as to whether vertebral changes are caused by strict malformation of the vertebrae or result from remodeling with underlying instability of the vertebral column being the primary lesion. In the latter theory, the soft tissues of the vertebral column are insufficient to maintain proper vertebral stability and alignment during postnatal development. Because of the uncertain etiology, there are multiple synonyms for this condition, including cervical spondylomyelopathy, cervical spondylopathy, cervical vertebral malformation-malarticulation, cervical vertebral stenotic myelopathy, and wobbler syndrome, with the latter arising from the fact that affected animals are often ataxic with a wobbling or swaying gait. No term is accepted universally.18,23 Cervical spondylomyelopathy will be used in this discussion. Cervical spondylomyelopathy is common in young Great Danes and mature Doberman pinschers, but there are many other large breeds that may be affected.21–23 There are often dissimilarities in the manifestation of cervical spondylomyelopathy in Doberman pinschers versus Great Danes. In the Doberman pinscher, vertebral canal stenosis, disc protrusion and/or herniation, and dorsal longitudinal ligament hypertrophy are common. Affected vertebrae sometimes have cranioventral flattening because of abnormal formation or remodeling. There can also be stenosis of the vertebral canal that results from underdevelopment of the pedicles (Fig. 11-14). This can result in the vertebral canal appearing cone shaped over the length of a vertebra, with it being narrower at the cranial aspect of the vertebra.21,23 Disc degeneration with protrusion and/or expulsion with concurrent and hypertrophy of the dorsal annulus fibrosis and the dorsal longitudinal ligament is also common in the Doberman pinscher.22–25 Cervical spondylomyelopathy in the Great Dane is often characterized primarily by articular process malformation and hyperostosis. As mentioned earlier, it is not clear whether this is a primary osseous malformation or whether these changes are secondary to cervical instability. Regardless, the hyperostotic articular processes commonly extend medially into the vertebral canal and cause spinal cord compression. Articular malformation and hyperostosis are usually visible radiographically, but MR imaging is preferred to assess the secondary changes, such as synovial cyst formation and spinal cord compression, more accurately (Fig. 11-15).
The Canine and Feline Vertebrae
Anatomic Considerations
Anomalies of the Vertebral Column
Block Vertebrae
Hemivertebrae
Transitional Vertebrae
Spina Bifida
Atlantoaxial Subluxation
Cervical Spondylomyelopathy
The Canine and Feline Vertebrae