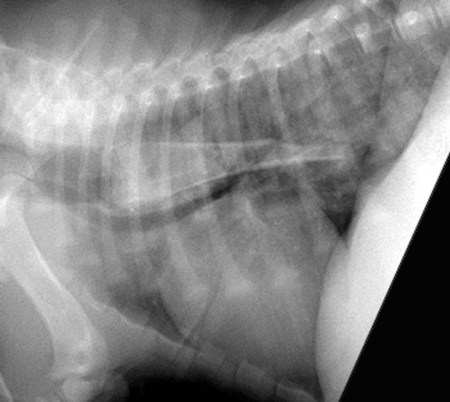
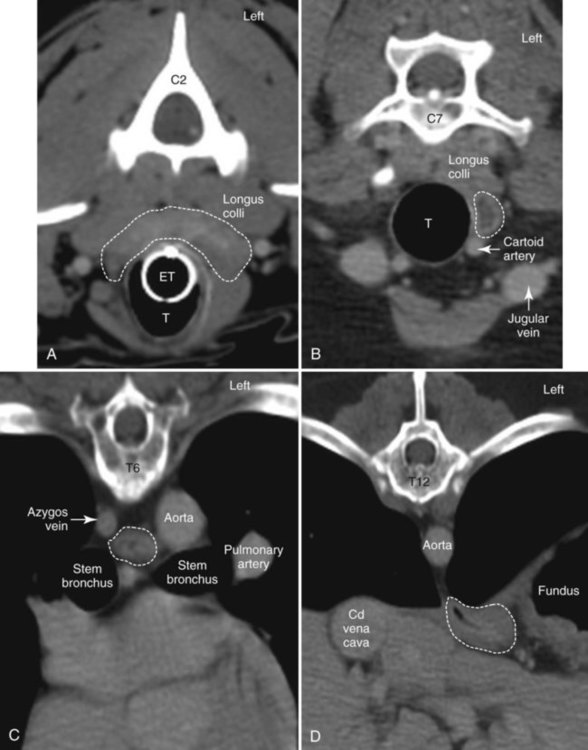
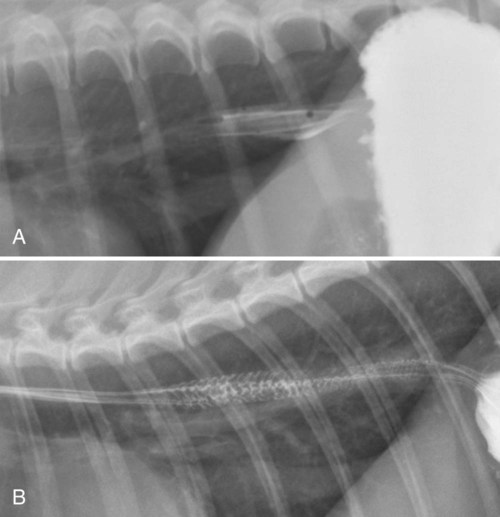
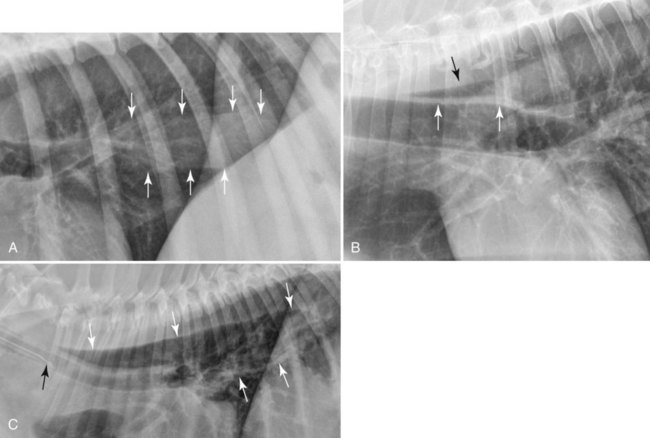
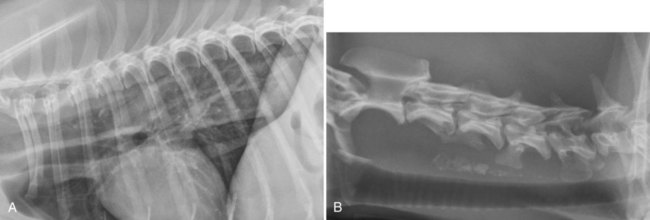
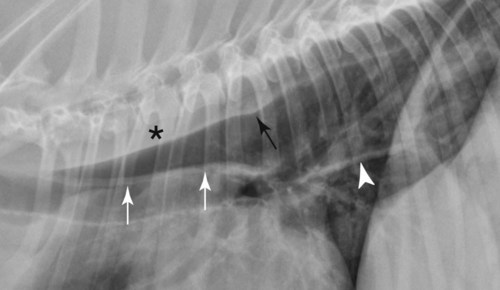
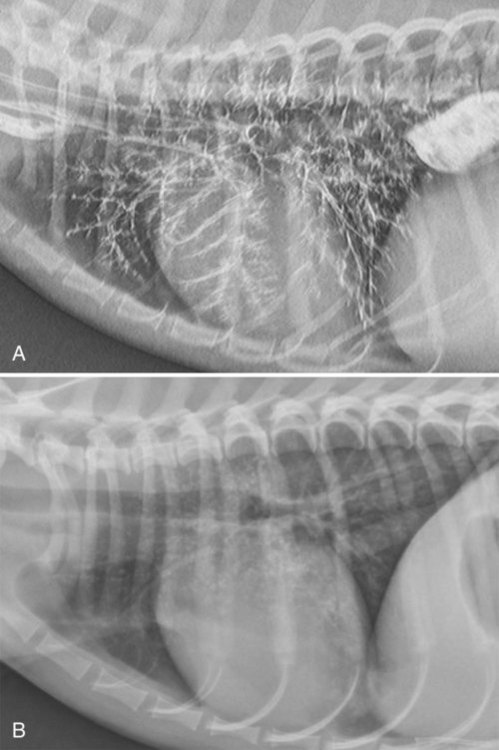
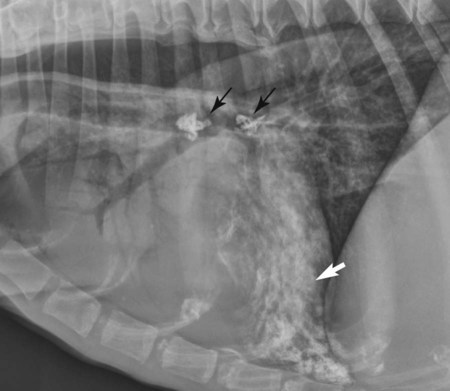
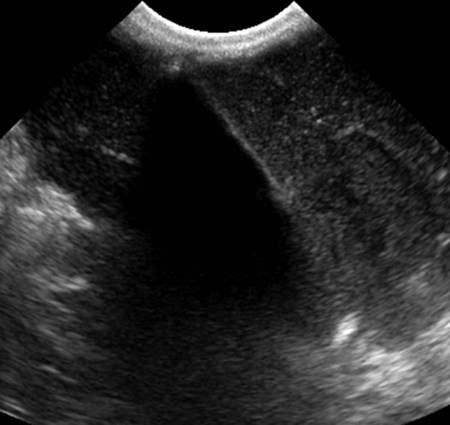
Clinical signs related directly to esophageal disease are gagging, retching, regurgitation, painful swallowing, and inability to swallow.1 Signs developing secondary to esophageal disease include pharyngeal and upper airway inflammation, nasal discharge, weight loss, pneumomediastinum, pneumothorax, pleural effusion, and aspiration pneumonia. Acute respiratory signs may also develop secondary to compression of the trachea by an esophageal mass. If the airway compression is severe, noncardiogenic edema can result; this is uncommon (Fig. 27-1). Survey radiographs of the thorax and cervical region, including the base of the tongue, are indicated in dogs and cats with clinical signs of esophageal disease. Survey radiographs and static barium esophagraphy provide structural information about the size and content of the esophagus and allow assessment of aspiration pneumonia and signs of esophageal perforation. Static contrast esophagraphy is helpful for characterizing the following conditions: esophageal mass, nonradiopaque foreign body, esophageal stricture, vascular ring anomaly, esophageal perforation, esophagitis, esophageal diverticulum, tracheo- or bronchoesophageal fistula, dysphagia, and hiatal hernia.2 Static contrast esophagraphy is not adequate for assessing dysphagia, where dynamic contrast studies performed with fluoroscopy are required. Dynamic studies are typically performed at specialty centers. Other than positive contrast radiography, other modalities are used only rarely to assess the esophagus. Scintigraphy can be used to quantify esophageal motility and transit time and diagnose gastroesophageal reflux.3 Computed tomography (CT) is helpful for further characterization of esophageal masses and their association with adjacent tissues and vessels for both diagnostic and presurgical purposes. Radiographic or CT angiography is required for the characterization of vascular ring anomalies and esophageal varices. Conventional transcutaneous ultrasonography is limited to evaluation of the cervical esophagus and, to some extent, the caudal esophageal sphincter and gastroesophageal junction. Endoscopic ultrasonography can be used to examine the thoracic portion of the esophagus.4 Indications include mural infiltration, fistula, diverticula, and periesophageal masses. Magnetic resonance imaging is not used for esophageal examination in animals but is used frequently to assess esophageal tumors in human beings. The esophagus begins cranially at the cricopharyngeal sphincter, also called the cranial esophageal sphincter, and continues to the esophageal hiatus at the diaphragm. The cricopharyngeal sphincter is formed by the cricopharyngeus and thyropharyngeus muscles. In the cranial aspect of the thorax, the esophagus is related closely to the longus colli and longus capitis muscles dorsally and to the trachea ventrally and to the right.5 In the neck, the cervical esophagus is located slightly to the left of the trachea, gradually becoming completely left-sided at the thoracic inlet (Fig. 27-2, A).5 The left common carotid artery, vagosympathetic trunk, internal jugular vein, and tracheal duct course through the angle between the esophagus and the longus capitis muscle. The right common carotid artery, vagosympathetic trunk, internal jugular vein, and tracheal duct are lateral to the trachea on the right side. The thoracic portion of the esophagus is in close proximity to the trachea. The esophagus is to the left of the trachea at the thoracic inlet (Fig. 27-2, B), but it gradually courses dorsally over the point of bifurcation of the trachea at the level of the fifth and sixth thoracic vertebrae (Fig. 27-2, C). At its dorsal location, it lies to the right of the aortic arch and is ventral to the longus colli muscles. Between the tracheal bifurcation and caudal esophageal sphincter, the esophagus lies in the median plane (Fig. 27-2, D). The vagal nerves run dorsocaudally across the sides of the esophagus and unite at the dorsal aspect of the esophagus a few centimeters cranial to the esophageal hiatus to form the vagal trunk, which passes through the hiatus with the esophagus. There are numerous longitudinal folds of the esophageal mucosa (Fig. 27-3, A). The wall consists of four layers: fibrous, muscular, submucosa, and mucosa. The muscular layer is composed of striated muscle in dogs along its entire length, and the entire length of the mucosa is characterized by longitudinal folds. In cats, the caudal third of the muscular layer is composed of smooth muscle, which is arranged obliquely creating a striated pattern on contrast esophagrams (Fig. 27-3, B). The caudal esophageal sphincter is formed by the focal thickening of the esophageal smooth muscle of the muscularis, confluence of the gastric folds oriented transversely, and the muscular sling created by the right crus of the diaphragm and the deep oblique smooth muscle of the lesser curvature of the stomach. Innervation of the esophagus is complex and involves 25 paired spinal ganglia from C2-L5. Neurologic control of swallowing is coordinated by cranial nerves V (trigeminal), VII (facial), IX (glossopharyngeal), X (vagus), and XII (hypoglossal), and their nuclei in the brain stem that, in turn, are controlled by areas of the reticular formation referred to as the swallowing center.6 The normal esophagus is usually empty and rarely evident on thoracic radiographs in cats and dogs because of its location within the mediastinum and silhouetting with adjacent muscles and mediastinal structures. On left lateral thoracic radiographs, the normal caudal thoracic esophagus sometimes contains a small amount of fluid and can be visualized as a faint tubular soft tissue opacity between the descending aorta and caudal vena cava (Fig. 27-4, A); this appearance is rare in right lateral radiographs. Gas can accumulate focally in the esophagus in animals that are excited, sedated, and dyspneic or under general anesthesia; this gas accumulation is usually minimal, and the most common location for this to occur is just cranial to the tracheal bifurcation (Fig. 27-4, B). Focal esophageal gas collections are dynamic and may appear differently or be absent in other radiographs acquired during the same study. General anesthesia or aerophagia may even lead to severe dilation of the esophagus, which can appear identical to pathologic megaesophagus (Fig. 27-4, C). Anesthesia-related megaesophagus will resolve spontaneously when the patient has recovered from anesthesia. Box 27-1 contains a list of radiographic signs that can be seen with esophageal disease. Gas in the esophageal lumen warrants further investigation in patients where it is thought to be pathologic and not a normal variant as described previously (see Fig. 27-4). It is important to examine the entire esophagus radiographically, meaning that radiographs of the cervical esophagus and pharynx are warranted in addition to thoracic radiographs (Fig. 27-5). There may be a tendency to confuse esophageal gas with pneumomediastinum, although there are some basic differences in the appearance of these conditions. With pneumomediastinum, there will be increased conspicuity of the adventitial surface of the esophagus and great vessels, as described in Chapter 30. With megaesophagus, the gas collection will be more contiguous, and a tracheal stripe sign will be present. The tracheal stripe sign is a soft tissue opaque band that is formed by the summation of the ventral aspect of the esophageal wall with the dorsal aspect of the tracheal wall, each outlined by gas in their respective lumen (Fig. 27-6; see Fig. 27-4). If the gas-filled esophagus is large enough, the ventral border of the longus colli muscle and the dorsal indentation created by the overlying azygos vein will be visible (see Fig. 27-6). When esophageal air is detected in animals with clinical signs of esophageal disease, an esophagram is indicated to rule out morphologic abnormalities such as a stricture or nonradiopaque foreign body. Normal variations such as kinks and bends in the cranial portion of the thoracic esophagus, sometimes referred to as redundant esophagus, can be identified in young dogs or short-necked brachycephalic breeds (Fig. 27-7). Contrast medium can accumulate temporarily in a redundant section and can appear as an outpouching as with an esophageal diverticula. Dynamic esophagraphy is needed to assess the significance of esophageal redundancy, as in some dogs the motility may be altered significantly in this region. Survey radiographs of the thorax and cervical region must always be performed immediately before a contrast esophagram. Static contrast studies provide structural information, whereas fluoroscopy is required to assess swallowing disorders and esophageal motility. Table 27-1 lists the types of contrast media that can be used for an esophagram, along with their advantages and disadvantages. Barium aspiration is a potential complication of performing esophageal contrast studies. Barium paste is contraindicated in animals at increased risk for aspiration because aspirated paste could cause airway obstruction. Aspiration of a small amount of liquid barium is usually insignificant. Pneumonia and lung granuloma formation are rare complications of barium aspiration. Aspirated barium is cleared from the airways by ciliary action, as well as coughing (Fig. 27-8). If barium enters the alveolar space, it may remain there permanently. Lymphatic uptake of aspirated barium will also be evident as amorphous mottled opacities in the region of the mediastinal and tracheobronchial lymph nodes, which may also be a permanent finding (Fig. 27-9). Table • 27-1 Contrast Media for the Esophagus Box 27-2 contains a list of contrast study techniques used for examination of the esophagus.7 The esophagram should be performed without sedation because most sedatives have an effect on esophageal motility and swallowing. Table 27-2 contains a description of the phases of swallowing and normal radiographic appearance of contrast studies. In general, there should be no retention of barium in the oral or pharyngeal cavity in static radiographs performed during swallowing. Some coating of the mucosa is normal. No contrast medium should be present in the pharynx, larynx, or trachea after swallowing. Table • 27-2 Phases of Swallowing, Control Mechanisms, and Radiographic Features in Normal Dogs Dysphagia can result from morphologic or functional etiologies. Morphologic causes include trauma, foreign body, an oral or pharyngeal mass, and regional lymphadenopathy. Lateral and ventrodorsal (VD) survey radiographs of the pharyngeal and cervical region and thorax are indicated to screen for radiopaque foreign bodies such as bones, needles, and fish hooks (Fig. 27-10). Soft tissue swelling and gas pockets can be seen with perforating pharyngeal trauma, abscesses, or a nonradiopaque foreign body such as a wooden stick. Ultrasonography is useful to determine the source of nonspecific pharyngeal swelling and nonradiopaque foreign bodies (Fig. 27-11). Evaluation of functional disorders of swallowing requires contrast fluoroscopy (Table 27-3). Videofluoroscopic contrast studies allow subtle events of the oral, pharyngeal, and cricopharyngeal phases of swallowing to be recorded and observed dynamically.a Frame rates of 30 to 60 per second are necessary to assess the rapid events of swallowing to make an accurate frame-by-frame analysis.6 The advantage of dynamic recordings is that subtle abnormalities associated with swallowing that would go unnoticed on static images can be detected. Cinescopy or digital fluoroscopy equipment will use slower acquisition rates of six images per second that also allow oral, pharyngeal (Fig. 27-12, A), cricopharyngeal (Fig. 27-12, B), and esophageal phases (Fig. 27-12, C) to be recorded, but subtle disease can go unnoticed as a result of the low frame rate. Table • 27-3 Types of Dysphagia, Causes, and Fluoroscopy Findings Bolus not formed or delayed formation Bolus not propelled caudally to pharynx
The Canine and Feline Esophagus
Relative Value of Radiography, Contrast Esophagraphy, Fluoroscopy, and Alternative Imaging Procedures
Anatomy and Physiologic Considerations
Normal Radiographic Appearance
Survey Radiographic Abnormalities
Contrast Esophagraphy Techniques
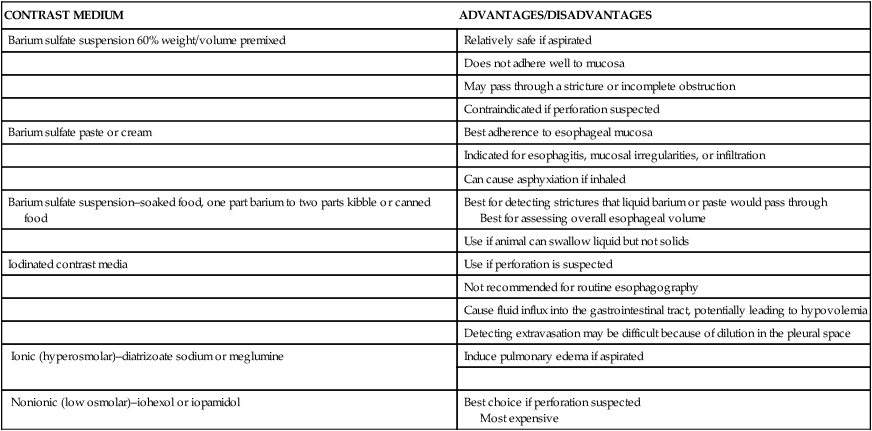
CONTRAST MEDIUM
ADVANTAGES/DISADVANTAGES
Barium sulfate suspension 60% weight/volume premixed
Relatively safe if aspirated
Does not adhere well to mucosa
May pass through a stricture or incomplete obstruction
Contraindicated if perforation suspected
Barium sulfate paste or cream
Best adherence to esophageal mucosa
Indicated for esophagitis, mucosal irregularities, or infiltration
Can cause asphyxiation if inhaled
Barium sulfate suspension–soaked food, one part barium to two parts kibble or canned food
Best for detecting strictures that liquid barium or paste would pass through
Best for assessing overall esophageal volume
Use if animal can swallow liquid but not solids
Iodinated contrast media
Use if perforation is suspected
Not recommended for routine esophagography
Cause fluid influx into the gastrointestinal tract, potentially leading to hypovolemia
Detecting extravasation may be difficult because of dilution in the pleural space
Ionic (hyperosmolar)–diatrizoate sodium or meglumine
Induce pulmonary edema if aspirated
Nonionic (low osmolar)–iohexol or iopamidol
Best choice if perforation suspected
Most expensive
PHASE
CONTROL MECHANISMS
RADIOGRAPHIC FEATURES
Oral
Hyoid apparatus
Formation of liquid or food bolus
Tongue
Reflex pharyngeal peristalsis starts
Facial nerve
Vagus nerve
Hypoglossal nerve
Pharyngeal
Pharyngeal musculature
Craniodorsal movement of the hyoid caused by pharyngeal contraction
Facial nerve
Vagus nerve
Bolus enters laryngopharynx
Glossopharyngeal nerve
Tongue stops backward and forward movement
Glottis closes entrance to trachea
Cricopharyngeal
Cricopharyngeal musculature
Relaxation of cricopharyngeal sphincter simultaneous with pharyngeal contraction
Vagus and glossopharyngeal nerves
Pharyngeal contraction propels bolus aborally
Esophageal
Mechanical stimulus of bolus
Esophageal musculature
Vagus nerve (sensory and motor)
Follows closure of cricopharyngeal sphincter.
Longitudinal folds appear as thin lines.
Primary peristalsis creates a bolus with a convex caudal border that is tapered cranially and is propelled aborally.
Secondary peristalsis initiated and occurs at 2–4 seconds.
Gastroesophageal
Diaphragmatic musculature, oblique implantation of the esophagus, cardia incisura, positive intraabdominal pressure, oblique smooth muscles of the lesser curvature
Slow passage through gastroesophageal junction
Small amount of reflux in normal; should induce a secondary wave
Dysphagia
TYPE
CAUSES
FLUOROSCOPIC FEATURES
Oral
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree