Chapter 9 Tachypnea and Hypoxemia
INTRODUCTION
An increased respiratory rate or tachypnea is almost always evident in the patient with respiratory distress, but the causes of tachypnea are numerous and it may or may not reflect respiratory tract disease. When developing an appropriate therapeutic and diagnostic plan, it is essential to differentiate between tachypneic patients with and those without concurrent hypoxemia. Hypoxemia can be detected with pulse oximetry or arterial blood gas analysis (see Chapter 208, Blood Gas and Oximetry Monitoring).
WORK OF BREATHING
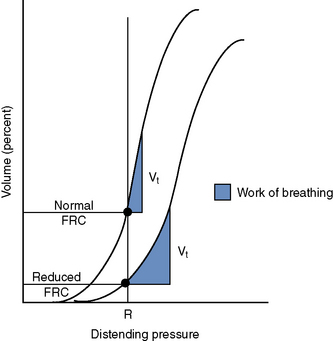
To understand how FRC is clinically significant we must understand compliance. Pulmonary compliance is reflected by the slope of the pressure-volume curve (Figure 9-1). The slope of this curve represents the volume change per unit pressure.1,5 When the slope of this curve is steep, a small change in pressure results in a large change in volume. This makes for efficient ventilation requiring minimal energy to effect gas movement. Diseases affecting pulmonary compliance can increase the work required for normal ventilation. Pulmonary atelectasis, pneumonia, pulmonary edema, fibrosis, and pleural space diseases (causing pulmonary collapse) are examples of conditions resulting in decreased pulmonary compliance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree