CHAPTER 34 Systemic Illness Caused by Corynebacterium pseudotuberculosis
Corynebacterium pseudotuberculosis is an uncommon but serious cause of systemic illness in horses. Mortality rates are as high as 40% in horses treated with antimicrobials, and systemic infections are fatal in horses that are not treated. Development of systemic disease involving the liver, lungs, kidneys, fetus, pericardium, mesentery, diaphragm, mediastinum, and uterus have been reported in horses from areas with endemic C. pseudotuberculosis disease. C. pseudotuberculosis infections are considered endemic in the western and southwestern regions of United States, especially California and Texas. In these regions, external subcutaneous abscess formation is the predominant form of disease. Recent outbreaks of C. pseudotuberculosis abscesses in Colorado, Wyoming, Utah, and Kentucky, where the disease was previously rare, suggests an expanding geographic distribution. Diagnosis of internal C. pseudotuberculosis infection can be difficult because of the insidious onset and nonspecific nature of clinical signs and clinicopathologic abnormalities. Although fewer than 10% of horses with C. pseudotuberculosis infection develop systemic disease, an increased index of suspicion is appropriate for systemically ill horses with a history of an external C. pseudotuberculosis abscess. Horses that reside on property where other horses have had external abscesses are considered at increased risk, and not all horses with systemic infections manifest external abscesses before becoming ill. Successful treatment and resolution of internal infection involves long-term antimicrobial treatment.
DIAGNOSIS
Clinical Signs
The most common clinical signs in horses with systemic C. pseudotuberculosis infections are nonspecific and include inappetence, lethargy, weight loss, respiratory signs and abdominal pain. Vital signs are variable depending on duration and severity of disease, organs affected and prior medical therapy. Horses tend to be mildly febrile, moderately tachycardic and mildly tachypneic. Most horses have a concurrent external C. pseudotuberculosis abscess and therefore also have ventral or limb edema. The presence of a concurrent external abscess may cause similar clinical signs, especially mild fever, and may therefore mask evidence of systemic infection and delay further diagnostic investigation.
Clinicopathologic Data
In one study, the most common clinicopathologic abnormalities were hyperproteinemia due to hyperglobulinemia and hyperfibrinogenemia and leukocytosis due to mature neutrophilia (Table 34-1). These findings are nonspecific for a chronic inflammatory or infectious process, and horses with external abscesses can have similar clinicopathologic findings. Most horses are not anemia, although some may have mild anemia of chronic disease. In some horses, mild anemia may be masked by dehydration. Low numbers of severely affected horses develop disseminated intravascular coagulation (DIC). Diagnosis of DIC is based on a combination of findings, including prolonged bleeding at venipuncture sites, petechial hemorrhages, thrombocytopenia, and abnormal coagulation test results (e.g., prothrombin time, partial thromboplastin time, fibrin degradation products, and antithrombin III activity). DIC develops secondary to many systemic disease conditions and septic processes and is generally associated with a poor prognosis.
Table 34-1 Representative Values of Abnormal Clinicopathologic Findings in Horses with Internal Corynebacterium pseudotuberculosis Infection
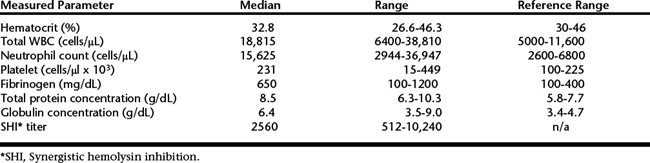
The serum synergistic hemolysin inhibition (SHI) test is a reliable aid in the diagnosis of systemic C. pseudotuberculosis infections. Horses with internal infection have reciprocal serum titers greater than 512 (see Table 34-1), although rare false-negative results may occur. Horses having only external abscesses may also have serum SHI titers of 512 or greater, but 40% will not have a high titer. The SHI test is useful in identifying C. pseudotuberculosis as the cause of systemic illness, but a complete clinical evaluation is necessary to establish evidence for an internal infection in horses with concurrent or recently resolved external abscesses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


