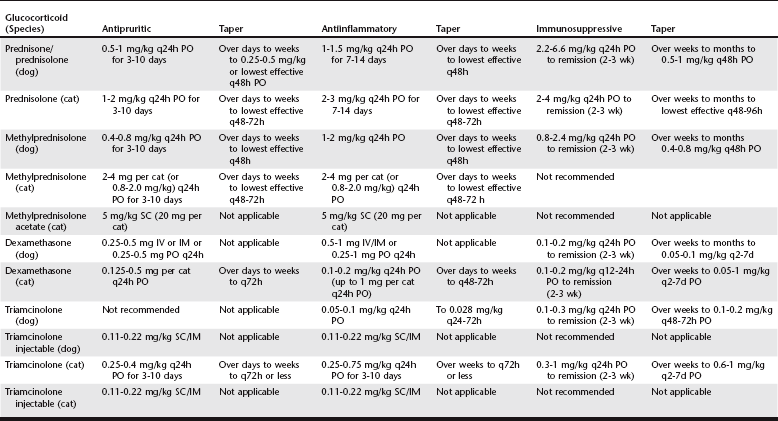
Chapter 94 Table 94-1 is a guideline to dosages of synthetic GCs commonly used in veterinary dermatology. Although sources often suggest twice-daily administration, the author prescribes oral GCs once daily in dogs and cats. It may be common to use injectable GCs in primary care practice, but the author rarely recommends this route because it does not allow for dosage adjustments or withdrawal in the event of severe adverse effects. Injectable GCs should be used only after careful consideration and when a patient shows no response to oral GCs. TABLE 94-1 Canine and Feline Dosages of Glucocorticoids Commonly Used in Veterinary Dermatology PO, Orally; IM, intramuscularly; IV, intravenously; SC, subcutaneously.
Systemic Glucocorticoids in Dermatology
Use of Glucocorticoids
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


