Chapter 13 Surgical Diseases of the Eye in Farm Animals
Vision is essential for food- or fiber-producing animals to safely exist in their environments and compete for food. Ocular diseases can result in con-siderable (up to extreme) discomfort to the patient with resultant poor weight gain, decreased milk production, behavioral problems, and poor performance.
Whenever possible, examination of the eyes should be performed in a quiet, dark room. Adequate restraint of the head is essential, and sedation of the patient may be necessary. In addition to an ophthalmoscope,* minimal specialized equipment† is necessary. Box 13-1 lists diagnostic and therapeutic equipment that fits easily inside a small, three-tiered fishing tackle box to make a compact and readily portable unit. In addition, lint-free cellulose sponges‡ are often helpful for fluid absorption but are expensive and only necessary when an eye is ruptured. Finally, a black cloth or cape for shrouding the head of the patient and examiner may be helpful if a darkened area for exam is not available but should be used with care to avoid startling patients.
BOX 13-1 SUGGESTED DIAGNOSTIC AND THERAPEUTIC OPHTHALMIC EQUIPMENT AND SUPPLIES
Portable Ophthalmology Essentials
Welch-Allyn 3.5 V rechargeable halogen direct ophthalmoscope with Finhoff transilluminator
Cobalt blue filter for transilluminator to enhance fluorescein stain fluorescence
20 Diopter or 2.2 D indirect ophthalmoscopy lens
Sterile cotton-tipped applicators and sterile gauze pads
Fluorescein stain strips—sterile
Allis, Bishop-Harmon, and Colibri tissue forceps
Small Metzenbaum or Stevens Tenotomy scissors
Small Derf needle holder or large Castroviejo
2-0 nylon on a straight needle
4-0 to 6-0 Vicryl on small cutting needle
Xylazine, detomidine, and butorphanol
Tropicamide 1%—short-acting mydriatic to dilate pupils
Proparacaine 0.5%—topical anesthetic
Sterile eye collyrium/eye irrigating solution in a spray bottle or sterile saline
#11, 12 and 15 BP scalpel blades (#12 is great for suture removal)
Glass slides (cleaned and in carriers)
20-g IV catheters for normograde nasolacrimal cannulation and for lavage of the palpebral fissure
Teat cannulae and tomcat catheters for retrograde nasolacrimal duct cannulation
30, 25, 20, and 18 g disposable needles
Tuberculin, 3-cc, 5-cc and two 12-cc syringes
Blood tubes—particularly red top (include 1 to 2 filled with formalin)
Culturettes®—preferably minitip
Examination and Medical Procedures
EYELID AKINESIA
In contrast to the powerful orbicularis muscle of the equine, ruminant species’ eyelids are much easier to open. However, any eyelid that is being held firmly shut by a patient should not be forced open for examination purposes unless the underlying disease process is known. Forceful attempts to open eyelids closed over a lacerated cornea may result in all the ocular contents being expelled into the examiner’s hand. In every instance, eyelids are most safely opened with the examiner’s hand(s) resting securely on the underlying orbit bones while the examiner’s fingers “walk” the lids open. Lids should not be forced open by direct application of pressure to the lid margins and thus to the underlying eyeball.
Eyelid akinesia is recommended as the safest way to open eyelids and is essential for standing ocular surgical procedures (nictitans, conjunctival or corneal surgery, etc.). Several methods are available to paralyze the upper eyelids, and akinesia should result within 5 minutes. In thinner-skinned animals (calves, sheep and goats), branches of the palpebral branch of the auriculopalpebral nerve may be palpated at any of a number of sites as branches cross the bony orbit rim dorsocaudal or dorsolateral to the eye along the zygomatic arch. One or more sites are cleansed, and topical anesthetic is injected subcutaneously (SQ, 1-5 ml/site) via a 20- to 25-gauge needle; the needle size and amount injected depend on the patient’s size. Nerve branches may not be palpable in adult cattle, but the palpebral nerves can be anesthetized as part of the Peterson Nerve Block (Figure 13-1). A 12-cm needle is inserted subcutaneously at the angle between the frontal and temporal processes of the zygomatic bone. This site is bounded by the zygomatic arch ventrally, the supraorbital process rostrally, and the coronoid process of the mandible caudally. The needle is directed caudally along the zygomatic arch and 10-20 cc of local anesthetic is infiltrated as the needle is advanced.
Complete lower lid akinesia can be difficult to achieve in ruminants, and although specific nerve blocks have been described, the author prefers to use a 20- to 22-gauge spinal needle (7-12 cm) inserted 1 cm ventral to the lateral canthus and directed medially through the lower eyelid to diffusely infiltrate local anesthetic throughout the lower eyelid. Before injection, topical anesthesia is applied to the ocular surface, and the lower eyelid is supported with finger pressure applied from inside as the needle is advanced, thus also protecting the globe.
TRANSPALPEBRAL OCULAR LAVAGE APPARATUS
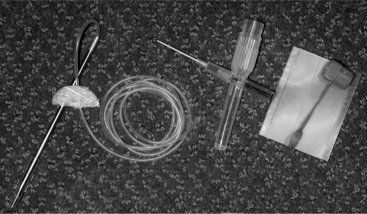
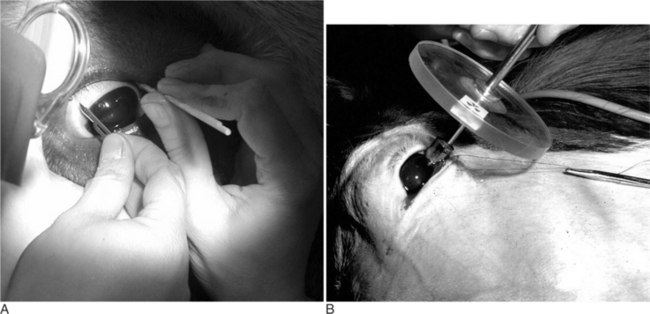
The transpalpebral catheter can be an extremely valuable adjunct to topical ocular therapy in ruminants, notably bulls that are otherwise unsafe to treat. The devices are readily available through commercial suppliers* or can be easily fabricated from polyethylene tubing (Figure 13-2). Medication infusion pumps can be attached to the catheters to help alleviate some handling of intractable patients, especially those with severe ocular disease that might need medication as often as every hour.
The patient is sedated, and the skin at the exit point of the catheter in the area of the dorsolateral orbit rim is cleansed. The upper eyelid is paralyzed as described above and 3 to 5 cc of local anesthetic are infiltrated subcutaneously at the planned exit site. The tubing is secured within a hubless needle or onto a wound drain insertion needle. The needle tip is securely cushioned in the tip of the surgeon’s index finger, and the needle with tubing inside is held in the same palm. The surgeon’s hand is turned so the index fingernail is toward the cornea and is inserted in the palpebral fissure. The finger with the needle then pushes dorsally until it is touching the inside of the orbit rim (through the palpebral conjunctiva). The opposite hand should simultaneously pull the upper lid out from the globe and over the inserting finger before the needle is advanced from the fingertip to ensure the needle tip does not “buttonhole” a conjunctival fold close to the lid margin, which could prevent proper blinking after the tube is secured. The lid is released, and the same hand is used to push the needle-tubing unit through the upper lid staying just rostral to the bony rim. The tubing is carefully pulled through with the needle until the footplate resistance is felt, taking care that the footplate remains inside the conjunctival sac and is not pulled into the subcutaneous tissues of the dorsal eyelid. At this point, the eyelid should be manipulated to ensure that it moves freely and is not caught on the tubing. Small pieces of waterproof adhesive tape (“butterflies”) are placed around the tube and sutured to the skin just adjacent to the exit point from the lid to prevent retrograde movement of the tubing and footplate into the conjunctival sac. Cyanoacrylate glue is applied over the tape and tube, further securing it to the skin (Figure 13-3). Additional adhesive tape butterflies are placed along the length of the tubing as needed.
Diagnosis of Globe and Orbit Diseases
CONGENITAL
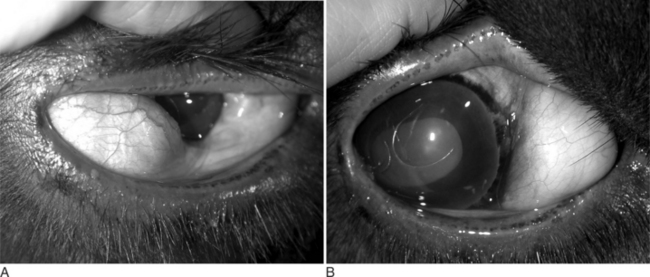
Common congenital abnormalities of the orbit and globe in ruminants include microphthalmos (a smaller-than-normal eye usually with multiple associated ocular defects) and strabismus (Figure 13-4). Patients with microphthalmos (Figure 13-5 A and B) have correspondingly small orbit bones that will not develop normally. Patients with microphthalmos may have associated cardiac, abdominal wall, or caudal spinal closure defects, and a careful physical examination is warranted. Culling may be indicated; a heritable component has been reported in some dairy breeds. Microphthalmos and a wide spectrum of blinding and nonblinding ocular anomalies such as cataracts (Figure 13-6) can occur with chronic vitamin A deficiency in pigs.
Unilateral or bilateral congenital strabismus of variable degree and direction may be seen in any species and may be seen associated with other physical and neurologic defects. Bilateral convergent strabismus (esotropia, Figure 13-7 A and B) with or without exophthalmos and nystagmus occurs in dairy cattle and may progress with age. Visual acuity is variable; the condition has been proven to be inherited in some dairy breeds and culling of affected animals may be indicated. If vision is impaired, affected animals may fail to thrive and have difficulty negotiating their environments.
EXOPHTHALMOS
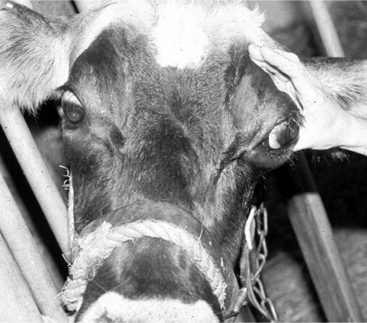
Exophthalmos in adult cattle is usually attributable to either inflammatory disease or neoplasia. A simple history and clinical presentation can often differentiate between these two broad categories. Inflammatory causes of exophthalmos (foreign body, cellulitis, sinusitis, infected tooth, myositis, etc.) are usually peracute to acute in onset, with the patient exhibiting marked pain when the affected eye is retropulsed into the orbit and when the jaw is opened (Figure 13-8). Affected animals are often febrile, depressed, and reluctant to eat. Abnormal ipsilateral nasal odor and discharge may be present with concurrent sinus involvement. In contrast, exophthalmos due to orbital neoplastic diseases is of slower onset, and the patient is rarely in discomfort except in cases of exposure damage to the cornea. Exophthalmos should be distinguished from glaucoma (rare in ruminants) and proptosis (protrusion of the eye from the orbit usually due to trauma). In a ruminant, an eye protruding from its orbit associated with trauma often carries a grave prognosis and is usually associated with other craniofacial injuries and possibly neurologic signs. A proptotic eye may require enucleation if it is ruptured or extensive extraocular muscle avulsion exists. Regardless of cause, an exposed eye requires immediate and frequent cleansing and moistening. The eye and periocular tissues can be moistened in an emergency with sterile saline, sterile eye wash or with any number of contact lens solutions until medical attention is available.
ORBITAL INFLAMMATION AND CELLULITIS
As stated previously, orbit inflammatory disease in cattle usually has peracute to acute onset and may be caused by foreign body penetration, puncture wounds, sinusitis, or extension of a severe infection in the eye (panophthalmitis). Puncture wounds and foreign bodies can enter the orbital space through the facial skin, palpebral fissure, or mouth; all of these areas should be examined carefully, if possible, during the physical examination. However, examination of the oral cavity may be difficult or impossible because of the pain from opening the mouth. Pain with jaw movement may be extremely severe and result in complete anorexia in some patients. The pain is only rarely attributed to temporomandibular joint disease and is more likely a result of movement by the coronoid process of the mandible compressing the retrobulbar tissues. Adjacent muscles of mastication may also be inflamed. Additional physical examination findings may include fever, anorexia, depression, mild-to-severe exophthalmos with possible exposure keratitis, periorbital swelling, and pain (Figure 13-9). Inspection and manipulation of wounds or draining tracts may reveal the presence of a foreign body. Abnormal ipsilateral nasal odor and discharge may be present with concurrent sinus involvement; sinus swelling may be evident and sinus resonance after percussion may be reduced or absent. Ultrasound and radiographic examinations are helpful in locating foreign objects and ruling out fractures, sinusitis, lumpy jaw, or a large mass such as a tumor. Fistulograms can be performed if draining tracts are present. A tissue aspirate for culture and cytology can be useful to confirm the presence of bacteria. Additional information regarding diagnosis and treatment of sinus disorders can be found in Chapter 9.
Treatment is directed at protecting the cornea, treating inflammation, and correcting the reason for cellulitis. The cornea is treated with sterile artificial tear ointments as often as needed to maintain corneal lubrication; if corneal ulcers are present, standard medical or surgical ulcer treatment is indicated according to the severity of the ulcer. Ophthalmology texts should be consulted for specifics.
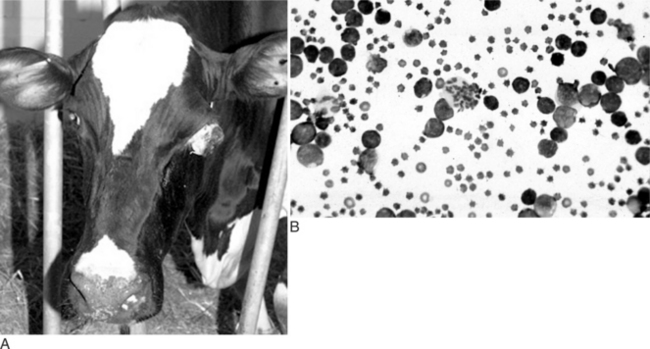
ORBITAL NEOPLASIA
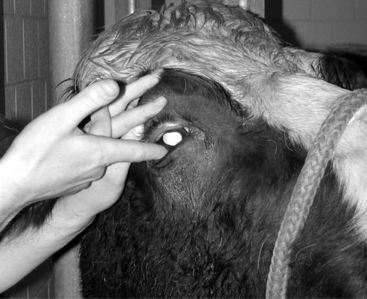
An adult dairy cow with unilateral or bilateral exophthalmos of subacute to chronic onset is most likely lymphosarcoma (Figure 13-10A and B). Other orbital neoplasias are rare but do occur, primary to the orbit or as extensions from adjacent tissues. Excessive orbital fat or orbital fat prolapse (Figure 13-11A and B) should be ruled out by palpation, cytologic sampling, or biopsy. If a biopsy is performed, the conjunctiva must be closed over fat or extensive orbit fat prolapse can occur. Digital palpation of the retrobulbar area through the palpebral fissure after application of topical anesthesia is a useful adjunct examination (Figure 13-12). Orbital fat is soft, fluctuant and nonpainful to palpation; inflammatory lesions usually are painful and firm while lymphosarcoma or other neoplasias are nonpainful but firm.
A complete physical examination should be performed—including careful cardiac auscultation and palpation of peripheral lymph nodes. Rectal examination is done with particular attention paid to uterine palpation and evaluation of regional lymph nodes. In some cases, the orbital mass or swelling may be felt adjacent or caudal to the globe by palpation posteriorly using a finger placed within the palpebral fissure after application of topical anesthesia. Fine needle aspiration of orbital tissues using a 20- to 22-g 7- to 12-cm needle with or without ultrasound guidance may be diagnostic (see Figure 13-10B). Serologic testing may be performed to assist in diagnosing lymphosarcoma.
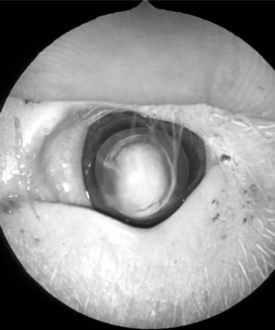
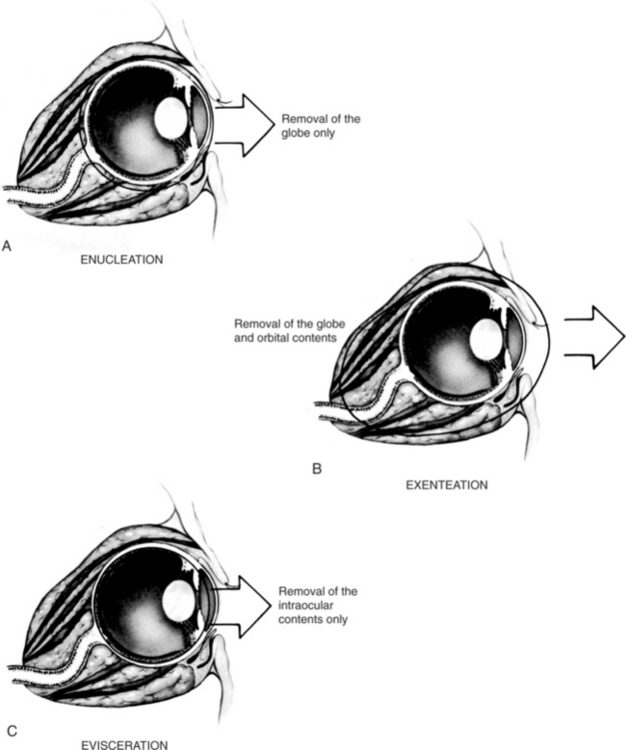
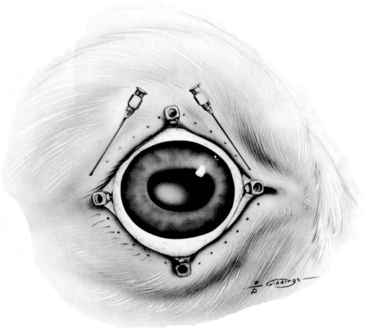
Moderate, progressive exophthalmos or a longer time to parturition may require protection of the globe(s) by permanent complete tarsorrhaphy (Figure 13-13). After sedation and application of local and topical anesthesia, the 2- to 3-mm–wide eyelid margin is trimmed off and discarded. Lids are closed with 3-0 to 4-0 absorbable sutures in the fibrous tissue layer of the eyelid (tarsal plate) and subcutaneous tissues with or without skin. If exophthalmos is severe, enucleation (Figure 13-14A) or orbit exenteration (Figure 13-14B) may be recommended. In rare instances in very valuable cattle, an evisceration may be performed before placing a prosthesis (Figure 13-14C).
General Surgical Techniques
PREPARATION OF PERIOCULAR TISSUES
Sterile artifical tear ointments are used to protect the cornea before preparation procedures. However, ointments should never be used perioperatively if an intraocular procedure is planned. If artificial tear ointments are not used during preparation, an anesthetized patient’s eyelids should be manually closed whenever they open, and sterile saline or collyrium should be applied frequently to the cornea to prevent corneal desiccation.
Removal of hair from any surgical field is standard presurgical protocol but requires particular care near the eye. Some surgeons do not remove any hair at all before intraocular surgery because of their concern that small pieces of hair may not be completely rinsed from the conjunctival fornices and may enter the open eye during surgery. Other surgeons clip only long or dirty periocular hairs with scissors but do not use electric clippers or razors out of concern for damage and irritation of the sensitive skin of the eyelids. Using care and sharp clipper blades, an experienced surgeon can clip periocular hair without trauma to the patient. Chemical depilatories must not be used near the eye; waxes may cause eyelid swelling and irritation and damage to the eye surface if carelessly applied.
BASIC OPHTHALMIC SURGICAL INSTRUMENTATION
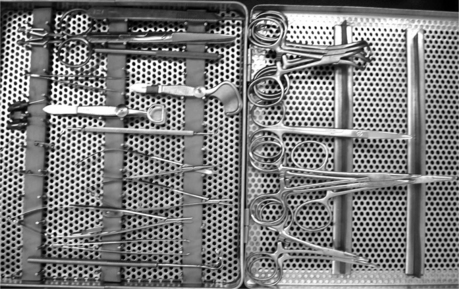
A basic ophthalmic instrument set (Figure 13-15) suitable for eyelid, conjunctival, and simple corneal surgery includes: small towel clamps such as Schaedel’s; Bard-Parker #9 blade handle; small Mayo scissors; general suture scissors; small stitch scissors (Westcott); forceps such as Adson or Brown-Adson suitable for eyelid surgery in large ruminants; Allis tissue forceps useful during entropion surgery; forceps such as fine Bishop-Harmon suitable for eyelid surgery in small ruminants; 4 Hartman curved mosquito hemostats; four 6″ Kelly hemostats; Derf or other small needle holder; large, curved utility scissors with serrated blade (enucleation in adult cattle); small curved and straight Metzenbaum scissors; small ophthalmic scissors such as a Stevens or Westcott tenotomy scissors, a small needle holder appropriate for 5-0 to 6-0 or smaller suture such as an 11 mm, nonlocking, curved Castroviejo needle holder; small tissue forceps suitable for cornea and conjunctiva, such as 0.4 mm Colibri-type 1 × 2 or delicate 1 × 2 Bishop-Harmon; double-ended Martinez corneal dissector; Snellen or Desmarres lid forceps with solid lower plate; simple eyelid speculum, such as a 20-mm Barraquer; Desmarres lid retractors (2); and nonlinting sponges.* A binocular magnifying loupe (see Figure 13-28A) is extremely useful for eye surgery in the field or hospital if better magnification systems are not available. Suture material appropriate for eye surgery should be available, including 4-0 silk for stay sutures and procedures such as tarsorrhaphies. Synthetic absorbable sutures, 4-0 to 7-0, with the smallest size needle available are suitable for corneal repair in smaller ruminants.
ANESTHESIA
If the surgery is to be done standing, adequate restraint with local and topical anesthesia is essential. The face is clipped and prepared for aseptic surgery. The cow is put in a chute or stanchion, and the head is tied snugly to the side. Local anesthesia has been described in a variety of ways. If a transpalpebral technique is used, local anesthetic should be deposited circumferentially 4 to 5 cm from the eyelid margins. To anesthetize the eye there are a few options. One possibility is to deposit 35 ml of 2% lidocaine in the retrobulbar cone using an 8.75 cm (3½ in) 18 gauge needle. Another way to provide analgesia to the retrobulbar area is with a Peterson nerve block (described under Eyelid Akinesia; see Figure 13-1). It is also possible to deposit anesthesia at 4 sites around the eye (Figure 13-16).
TRANSPALPEBRAL ENUCLEATION
After appropriate preparation and thorough nasolacrimal duct lavage, the eyelids are sutured together or clamped. A circumferential incision 1.5 cm away from the eyelid margin is made through the skin into the subcutaneous tissues of the eyelid but not through the conjunctiva. The lateral and medial canthal ligaments securing the eyelids to the orbit bones are transected. As traction is applied to the freed eyelids, dissection is continued caudally toward the orbit rim taking care to stay external to the conjunctival sac, which should remain closed. Close to the orbit rim the deep fascia forming the orbital septum is penetrated, and the extraocular muscles and tissues within the orbital cone can be visualized. In cases of panophthalmitis or when enucleation is necessary because of severe orbital cellulitis, the extraocular muscles and the other soft tissues within the periorbita should be excised as widely as possible or transpalpebral exenteration should be performed. Significant bleeding will occur in these cases. In other cases in which infection of the eye is not a concern, intraoperative bleeding is considerably lessened if each rectus muscle is transected at its tendon of insertion on the sclera. As each muscle is encountered, one blade of a Metzenbaum scissor is inserted between the muscle and sclera, and the scissor is pulled anterior toward the limbus before cutting, thus ensuring that the transaction occurs through muscle tendons, which bleed much less than the muscle belly. The dorsal and ventral oblique muscle insert deep to each respective rectus muscle and may have very short tendons of insertion. They are transected close to the sclera. After rectus and oblique muscle transection, the globe is grasped, and gentle traction is applied, thus making the retractor muscles that form a cone around the optic nerve easier to visualize. Traction on the globe should be minimal to decrease vagal nerve stimulation and avoid potential damage to the optic chiasm. With gentle medial traction on the globe, the surgeon should attempt to “strum” the optic nerve-retractor muscle cone using an approach from the dorsolateral side of the orbit. Once the location of the nerve has been confirmed, the same hand is used to position the blades of a large curved serrated utility scissor around the cone. The cone is rarely visualized directly because of variable amounts of orbital fat and hemorrhage; therefore digital palpation is important. One or two cuts of properly placed scissors will almost completely free the globe. It is held in one hand, and the remaining medial attachments severed. The entire third eyelid should be removed at this time. To prevent postoperative lacrimocele formation, it is recommended the lacrimal gland located in the periorbita of the dorsolateral orbit ventral to the orbit rim be surgically removed as well.
Meticulous hemostasis during enucleation is time-consuming, and in most cases not necessary. In the enucleation technique described above, no attempt is made to ligate the optic nerve and muscle cone because ligatures placed around the optic nerve and muscle cone are difficult to place, usually slip, result in tissue trauma in the process, may increase vagal stimulation, and can act as a foreign body inciting an inflammatory response. The orbit is packed with sponges and pressure is applied as closure commences, but all sponges are removed before the subcutaneous tissues are completely closed. An absorbable suture (no. 2-0) is used to close subcutaneous tissues; a nonabsorbable suture is used in the skin (Figure 13-17). A pressure bandage is applied for 24 hours and the pressure of the sutured incision combined with the bandage will almost always be adequate to stop hemorrhage. Drains are not necessary unless there is preexisting infection. Antibiotics should be given for 5 to 7 days after surgery.
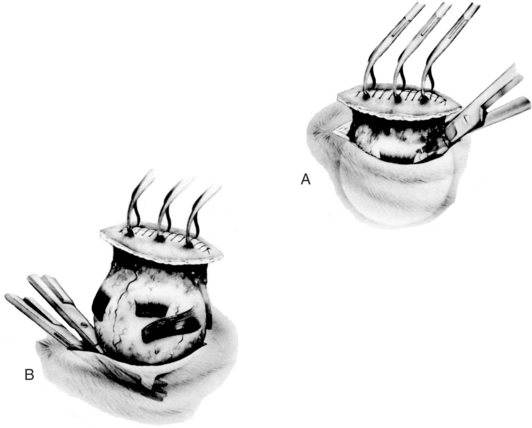
TRANSPALPEBRAL EXENTERATION
Exenteration means the globe and as much of the ocular contents as possible are removed. For exenteration surgery, the dissection is done outside the extra ocular eye muscles and conjunctiva, all of which are removed with the globe (Figure 13-18A). For extensive SCC in cattle, this may be the preferred procedure.
The same transpalpebral approach is recommended. The plane of dissection is against the bony orbit. All extraocular eye muscles are removed along with a substantial portion of the optic nerve (Figure 13-18B). If possible, a subcutaneous tissue layer is closed. A drain may be necessary for 48 to 72 hours. Skin is closed routinely.