Chapter 15 Surgery of the Calf Musculoskeletal System
Numerous musculoskeletal system diseases in farm animals exist—ranging from the more rare congenital abnormality (malformation, angular or flexural deformity) to acquired diseases such as septic arthritis and fractures. This section will describe diseases seen mainly in calves, such as angular and flexural deformity as well as other congenital abnormalities. The readers are directed to Chapter 11 for the principles of diagnosing and managing fractures).
15.1 Polydactyly
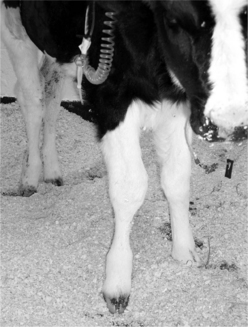
The clinical diagnosis is straightforward. The front limbs are generally affected. Radiographic examination helps determine the extent of the abnormalities (Figure 15.1-1). Surgical removal is done with the animal under general anesthesia with the abnormal digit uppermost. Consideration of placement of surgical incisions should allow sufficient skin for closure. In addition to skeleton being removed (Figure 15.1-2A and B), the flexor tendons associated with a deformity must also be removed. One should carefully dissect the flexor tendons to ensure that the remaining flexor tendons are left as a functional unit.
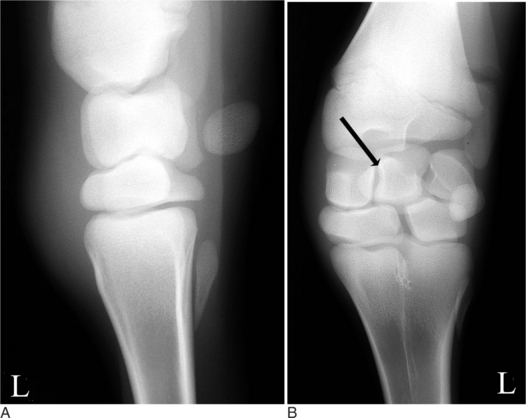
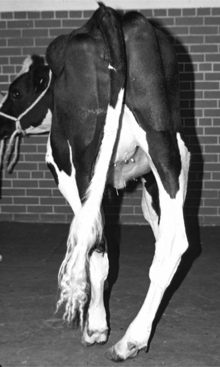
Figure 15.1-2 Postoperative radiographs of calf in Figure 15.1-1 after removal of the supranumary phalangeal, sesamoid, metacarpal, and distal carpal bones. A, lateral view. B, Dorsopalmar view; note remaining proximal carpal bone (arrow).
(Courtesy of Dr. Markus Wilke; Cornell University.)
15.2 Flexural Deformities
Calves present with flexural deformity (i.e., contracted tendons) either as a congenital or acquired problem. Congenital flexural deformities are seen within 1 or 2 weeks of birth. Flexural deformity ranges in severity from mild knuckling at the fetlock to being unable to walk, stand, and nurse. The etiology of congenital flexural deformity in cattle is generally unknown, but cattle seen with additional congenital abnormalities may have a heritable condition and should be removed from the breeding pool. Other congenital abnormalities sometimes seen simultaneously with flexural deformity are cleft palate, dwarfism, and arthrogryposis. Lupine ingestion by the dam between 30 and 70 days of gestation may result in arthrogryposis. In addition to congenital flexural deformity, acquired flexural deformity is seen secondary to reduced weight bearing associated with a primary painful orthopedic disease.
Clinical Presentation
Usually, calves present with mild metacarpophalangeal (MP) or carpal flexural deformity. The condition is mild and usually bilateral. In a more severe presentation, the calves have constant knuckling of the fetlocks; the carpus sometimes is also involved (Figure 15.2-1). Rarely, the metatarsophalangeal joints are affected. Owners report that calves are born with this condition or develop it within a few days to a week of birth. The deformity may be so severe that calves are unable to stand, so failure of passive immunity transfer may be a complicating factor. Abnormal hoof wear is present as a result of irregular weight bearing. Depending on the housing situation and disease chronicity, affected calves that must compete for feed may have poor body condition.

Figure 15.2-1 Newborn calf with bilateral carpal and metacarpophalangeal deformities.
(Courtesy of Dr. Mary Smith; Cornell University.)
Acquired flexural deformity seen in older calves is generally unilateral and secondary to a severe orthopedic injury where the animal cannot bear any or only minimal weight on the affected limb (Figure 15.2-2). A dropped fetlock and varus deformity at the carpus of the contralateral limb is evidence of excessive weight bearing.
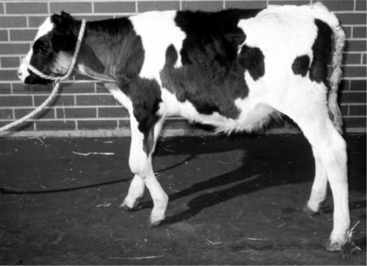
Figure 15.2-2 Heifer calf with unilateral carpal flexural deformity secondary to a primary carpal orthopedic disease. Note enlarged carpus.
Diagnosis
The diagnosis can be easily made when the abnormally flexed position of the limb with the deformity centered on the affected joint is observed (see Figure 15.2-1). One should use palpation in an attempt to identify a cause for the deformity, such as a swollen joint, ruptured extensor tendon, or other orthopedic lesions (see Figure 15.2-2). This is especially true in acquired flexural deformities of calves. One should flex and extend the affected limb to identify a painful process that may be contributing to the deformity. The veterinarian should also evaluate how much of the deformity can be corrected by manually extending the limb. Although radiographs illustrate the deformity of the axial skeleton well, they rarely add to the diagnosis. Radiographs only help identify the extremely rare orthopedic malformations (i.e., deformed joints that cause a deformity).
Management
Mild cases of flexural deformity respond well when patients are placed in housing with good footing. In addition, rather than spending extended periods standing, daily walking exercise is preferable. Treatment for more affected calves depends on whether the leg can be straightened manually so that the calf can walk. Medical treatment is indicated when no predisposing orthopedic anomaly is present and the limb can be manually extended so the toe’s ventral aspect can touch the ground. A splint should be placed on the palmar aspect of the limb, starting at the heel (leaving the claws out) and extending to the proximal metacarpal (or metatarsal) III bone (for MP flexural deformity) or proximal radius (for carpal flexural deformity). The splint is changed every 2 to 3 days. Alternatively, a cast may be placed and removed/changed 2 to 3 weeks later (Figure 15.2-3). Although oxytetracycline IV (3 g in 250 ml of physiological saline) can be given to relax the muscles for more rapid correction of the limb, it should be avoided whenever possible in calves. Tetracycline is very nephrotoxic in calves, so a single treatment may result in significant renal damage.
To correct a MP flexural deformity, a 7.5-cm incision is made over the lateral (or medial) aspect of the deep digital flexor tendon at the level of the midcannon bone. The fascia surrounding the flexor tendon is incised in the same plane, with care taken not to injure the lateral (or medial) palmar (or plantar) digital artery, vein, or nerve. The superficial digital flexor tendons and the connecting branches from the suspensory ligament are identified and elevated with curved hemostats. The superficial digital flexor tendons should be carefully elevated and isolated to prevent injury to the contralateral vessels. The superficial digital flexor tendons and the connecting branches from the suspensory ligament are transected after they are isolated. The surgeon then extends the fetlock to evaluate the degree of correction achieved. The goal is to obtain sufficient correction so that the hoof contacts the ground without the fetlock knuckling. Exercise and the calf’s body weight will place the joint in a normal position when the calf is walking if the knuckling is corrected. If the deformity is not sufficiently corrected after the superficial digital flexor muscle is transected, the tendons of the deep digital flexor muscle are isolated and transected as described previously. If the deformity is still not sufficiently corrected, the suspensory ligament is identified immediately caudal to MC (or MT) III, isolated with a curved hemostat, and transected. The peritendinous fascia and subcutaneous tissues are closed separately with nonabsorbable sutures in a simple continuous pattern. The skin is closed with an acceptable pattern.
Anderson DE, St Jean G. Diagnosis and management of tendon disorders in cattle. Vet Clin North Am Food Anim Pract. 1996;12:85-116.
Dyce KM, Sack WO, Wensing CJG. The forelimb of ruminants. In: Dyce KM, Sack WO, Wensing CJG, editors. Textbook of veterinary anatomy. Philadelphia: WB Saunders, 1996.
Van Huffel X, De Moor A. Congenital multiple arthrogryposis of the forelimb in calves. Comp Cont Ed Pract Vet. 1987;9:F333-F339.
Verschooten F, De Moor A, Desmet P, et al. Surgical treatment of congenital arthrogryposis of the carpal joint associated with contraction of the flexor tendons in calves. Vet Rec. 1969;85:140-171.
15.3 Angular Deformities
Etiology
Growth plate differential growth commonly seen in horses is rarely seen in farm animals. More accurately stated, angular deformity is a common event in cattle in that most calves have a mild carpal valgus deformity of approximately 7 degrees (Figure 15.3-1), which is within the normal range for most farm animals and does not require treatment. Orthopedic injuries such as fracture and its healing process, collateral ligament tear, physeal infection (Figure 15.3-2), or physeal fracture commonly cause secondary angular deformity.

Figure 15.3-2 Septic physitis in a ewe with angular deformity. Note the lytic area at the physis (arrows)
(Courtesy of Dr. Anthony Pease; Cornell University.)
Clinical Presentation
Animals presented for evaluation of angular deformities are easy to recognize. For an accurate diagnosis, one should align himself or herself with the claws and evaluate whether all the long bones are in line (see Figure 15.3-1). This perspective is important because differentiating an angular deformity from a rotational deformity is difficult when one is observing the animal from the front or back. Standing directly in the center front of the claws eliminates the rotational deformity as a confounding factor.
Further examination should focus on the area where the limb loses linearity. Physical examination can assess whether pain or other signs of an orthopedic injury—including the following—are present: increased laxity, swelling and its characteristics, degree of lameness, and presence of muscle atrophy. Although valgus deformity is relatively common (it may be normal for cattle), varus deformity is abnormal (Figure 15.3-3). If varus deformity is found unilaterally, the contralateral limb should be examined for a significant orthopedic injury as a cause for excessive weight bearing in the deformed limb/joint. Obtaining radiographic evaluation is important in investigation of orthopedic injuries, which are often important causal factors in angular deformity in farm animals.
Diagnosis
The diagnosis is made based on the clinical signs, but an exact etiology may not be determined unless radiographic examination is done. A dorsopalmar view is needed for examination of the anatomical location of the deformity and its measurement (Figure 15.3-4). Like the visual examination, the dorsopalmar view must be taken with the radiographic beam in line with the claws. To estimate the degree of angular deformity, a long cassette is needed so that more accurate lines overlying the center of the longitudinal axis can be drawn. The area of divergence (pivot point) of these lines confirms the angular deformity site, and the radiographic abnormality helps identify the causes (see Figure 15.3-4). Further radiographic views may be needed, depending on the nature of the injury or problem.
Management
MEDICAL MANAGEMENT
Trimming the claws of a young calf creates growth plate response to stress applied opposite the deformity, so self correction occurs. The trimming and other hoof manipulation is based on the principle that the hoof will turn in the direction of the longer claw or toward the side of the wider wall (Figure 15.3-5). To correct a valgus deformity, the lateral claw is trimmed so that it is shorter than the medial claw. To correct a varus deformity, the medial claw is trimmed so that it is shorter than the lateral claw. Acrylic can also be applied. Acrylic is applied over the lateral aspect of the lateral claw of a varus deformity to make the claw wider with more lateral contact with the ground. The lateral claw must not extend more than 1 cm; otherwise the stress on the lamina may cause inflammation and pain. The procedure is reversed for a valgus deformity (extend the medial wall of the medial claw). Finally, a shoe may be glued onto the claw to extend the lateral or medial claw.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree