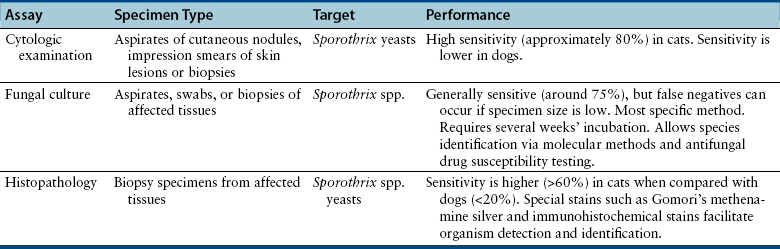
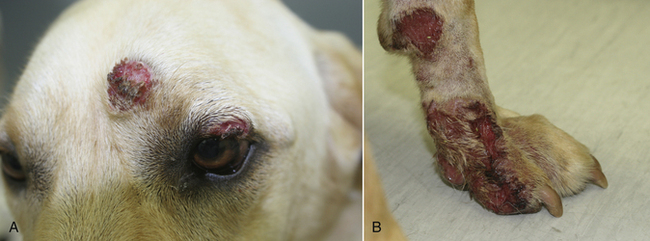
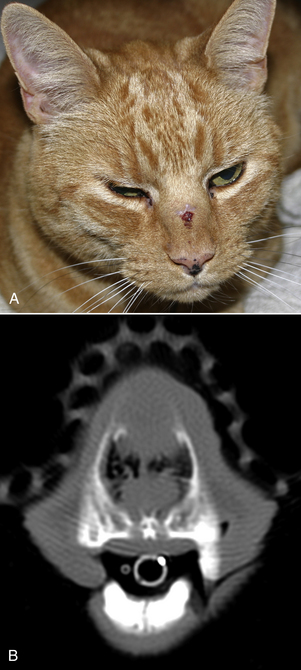
Chapter 64 Sporothrix species thrive in humid conditions (92% to 100%) and at mean temperatures between 25°C and 30°C. They prefer moist soil that is rich in decaying vegetation, as well as sphagnum moss, wood, thorns, or hay, where they grow as mycelia. The fungus is distributed worldwide in tropical and temperate zones but is most prevalent in tropical or subtropical regions of the Americas. Regions of endemicity include Mexico, Brazil, Uruguay, Peru, Japan, India, and South Africa; sporotrichosis is uncommon in Europe. Although all Sporothrix isolates have in the past been grouped into one species, multiple genotypes exist that vary in virulence and geographic distribution.2–4 As a result, an S. schenckii species complex has been identified, which includes at least six species: S. schenckii sensu stricto, Sporothrix brasiliensis, Sporothrix globosa, Sporothrix mexicana, Sporothrix albicans, and Sporothrix luriei.5–7 The epidemiology of the various members of the complex is as yet incompletely understood. S. globosa has a worldwide distribution, whereas S. brasiliensis appears to be limited to Brazil. S. schenckii, S. brasiliensis, and S. albicans have been isolated from cats, and S. schenckii and S. luriei have been isolated from dogs.8 Cats are more susceptible to sporotrichosis than dogs and are thought to facilitate spread of organisms in the environment.9 Contaminated claw or bite wounds, as well as autoinoculation during grooming, are thought to be important modes of transmission.10 Male cats are overrepresented in most studies (60% to 70% of affected cats), which may reflect the tendency of male cats to roam outdoors and be involved in aggressive interactions.10–13 In Rio de Janeiro, a large outbreak of sporotrichosis has occurred over the past decade, which has involved more than 1000 humans, 60 dogs, and 1500 cats.1 Of affected cats in this outbreak, Sporothrix spp. were isolated from 100% of 76 cutaneous lesions, 66% of 71 swab specimens from the nasal cavity, 41% of 79 oral swab specimens, and 40% of 38 nail fragments.14 The fungus was also isolated from 3 of 84 apparently healthy cats that were in contact with affected animals. Twenty percent of cats were positive for antibodies to FIV, 1% of cats were positive for FeLV antigen, and 1% of cats were positive for both FIV antibodies and FeLV antigen.10 More than 85% of affected cats were less than 4 years of age. Of isolates from affected humans in the outbreak, most were S. brasiliensis, but S. schenckii sensu stricto and S. globosa were also isolated.7 In dogs, sporotrichosis is relatively rare. Cutaneous introduction of the organism with plant foreign bodies has been suggested in some cases. In one dog, the portal of entry was thought to be an alligator bite wound.15 In the Brazilian outbreak, contact with cats appeared to be an important mode of transmission to dogs.16 No clear breed or sex predisposition has been identified, and dogs in the Brazilian outbreak ranged in age from 6 months to 12 years (median, 4 years). Mixed sporotrichosis and cryptococcosis was reported in a dog from Ontario.17 Transmission of Sporothrix primarily results from cutaneous inoculation of organisms in the environment, but can also result from inhalation of conidia. Direct contact with cats that have sporotrichosis (without an apparent break in the skin) can also result in transmission.10 Once within tissues, the organism converts into a yeast form. The yeast form has a cell wall that contains glucans, a glycoprotein fraction known as peptidorhamnomannan, and galactose-containing polysaccharides. The cell wall also contains melanin, which may protect the yeast from oxidative damage.1,9 Adhesins on the surface of the organism bind fibronectin, which appears to be important for virulence.18 Organisms that are thermotolerant (able to survive at temperatures closer to body temperature, or 37°C) may be more likely to cause invasive disease.9 Several clinical forms of sporotrichosis are recognized in human patients. The clinical form of disease that develops depends on host factors and the virulence of the infecting Sporothrix strain. A suggested classification system for human sporotrichosis categorizes the distribution of lesions into cutaneous, mucosal, or extracutaneous (Table 64-1). Cutaneous lesions are crusted, plaque-like, or nodular lesions that often ulcerate or drain serosanguineous fluid. They may be fixed (localized), track along the course of lymphatics (lymphocutaneous), or be multifocal (sometimes referred to as disseminated cutaneous disease) (Figures 64-1 and 64-2). More than 50% of human patients develop the lymphocutaneous form and the infection spreads proximally along lymphatics, with formation of multiple secondary nodules (also known as gummata) that may ulcerate. This form has not been clearly recognized in cats and appears to be uncommon to rare in dogs.16 Up to 80% of cats with sporotrichosis have multiple, widely distributed cutaneous lesions.10,13 These may develop as a result of autoinoculation during grooming, or they can be a manifestation of a disseminated (or generalized) systemic infection. TABLE 64-1 Proposed Classification Scheme for Clinical Forms of Sporotrichosis in Human Patients1 FIGURE 64-1 Cutaneous and mucosal sporotrichosis. FIGURE 64-2 Multifocal ulcerated cutaneous lesions on the head (A) and left thoracic limb (B) caused by Sporothrix spp. in a 2-year-old male neutered Labrador retriever. (Courtesy University of California, Davis, Veterinary Dermatology Service.) Extracutaneous disease follows inhalation of conidia or hematogenous spread of Sporothrix from sites of cutaneous inoculation. Transmission by inhalation is thought to occur in some cats, because pulmonary and nasal cavity disease with associated respiratory signs are common in cats.10–13,19 Respiratory signs include sneezing, cough, tachypnea, increased respiratory effort, stertor, and/or nasal discharge. Respiratory signs were present in 44% of 347 cats in the Brazilian outbreak10 and can also occur in dogs.13,16 Sneezing may occur before the onset of cutaneous lesions in cats, and some cats or dogs show only respiratory signs. Cats also can develop generalized disease, with involvement of multiple organ systems, which include the lungs, liver, spleen, kidneys, lymph nodes, and testicles.13,20 Co-infection with FIV does not appear to be a risk factor for dissemination.21 Isolation of Sporothrix species from the blood of 35% of 49 cats with focal or multifocal cutaneous involvement was reported.21 Clinical signs of systemic involvement include fever, generalized lymphadenomegaly, anorexia, dehydration, vomiting, and weight loss. These signs were each reported in fewer than 20% of cats with sporotrichosis; vomiting occurred in fewer than 5% of the cats.10 Weight loss, vomiting, or anorexia can also occur in dogs.13,16 Other rare forms of extracutaneous sporotrichosis described in humans include osteoarticular and meningeal sporotrichosis. Osteoarticular sporotrichosis occurs rarely in dogs and may manifest clinically as lameness and synovial effusion.12,22 In cats, cutaneous lesions are most often found on the head (especially the bridge of the nose and the nasal planum, eyelids, and/or pinnae) and have a similar appearance to those caused by Cryptococcus spp. (see Figure 64-1).10,12,23 Other common sites for skin lesions are the distal limbs, digits, and tail, but lesions can also be found elsewhere on the body. Swelling of the conjunctiva or lesions in the oral cavity or nasal cavity can be present in some affected cats (see Figure 64-1). Cutaneous or subcutaneous lesions are often firm nodules that sometimes enlarge to form soft cutaneous masses. Nodules can ulcerate and drain serosanguineous to purulent fluid, but are usually not painful or pruritic.12 In some cases, ulcerations and draining skin lesions are not associated with the formation of discrete nodules. Lesions range in diameter from a few millimeters to several centimeters. Extensive zones of necrosis with exposure of underlying muscle and bone have also been described.10 Regional lymphadenomegaly may be detected. Other less frequent physical examination findings in cats are fever, nasal discharge, decreased nasal airflow, tachypnea, increased respiratory effort, dehydration, and thin body condition. In dogs, lesions consist of single or multiple ulcers or nodules on the head, trunk, forelimbs, and/or digits (see Figure 64-2). Rarely, they course along lymphatics.12,13,16,24 The nasal planum was affected in 59% of 44 dogs in one study, and 21% of dogs had nasal mucosal involvement.16 Regional lymphadenomegaly is common. Diagnosis of sporotrichosis rests on identification of the organism by cytologic or histopathologic evaluation, or by fungal culture of lesions (Table 64-2). A high degree of suspicion is required for the disease in non-endemic regions. Sporotrichosis should be considered in any dog or cat with cutaneous lesions suggestive of cryptococcosis or other deep mycoses, and especially any cat with ulcerative or nodular lesions of the face. In many dogs and cats with sporotrichosis, the CBC is unremarkable. The most common abnormalities are mild anemia and leukocytosis due to a neutrophilia, sometimes with a mild left shift.10,24 Monocytosis, eosinophilia, lymphocytosis, or lymphopenia may also be present. Approximately 50% of dogs in the Brazilian outbreak were anemic, and around 20% had eosinophilia or neutrophilia.16 The most frequent serum biochemistry findings in cats and dogs with sporotrichosis are hyperglobulinemia and hypoalbuminemia.10,16 Rarely, increased liver enzyme activities are present in affected dogs.16 Findings on plain thoracic radiographs in cats with pulmonary sporotrichosis have not been described in detail. An interstitial infiltrate was described in one affected cat.20 Thoracic radiographs were performed on one dog and five cats seen at the author’s teaching hospital, but no radiographic abnormalities were present. Radiographs of bones that underlie skin lesions typically reveal only soft tissue swelling; rarely is underlying osteomyelitis detected. In the author’s hospital, computed tomography (CT) of the nasal cavity in a cat with a lesion on the bridge of the nose revealed an irregular rim-enhancing mass within the nasal cavity that invaded through the nasal bones to involve the subcutaneous tissues (Figure 64-3). Severely thickened turbinate mucosa, an intranasal soft tissue density mass, and focal osteolysis were reported on nasal CT in a dog with signs of nasal cavity disease due to sporotrichosis.25 FIGURE 64-3 Nasal sporotrichosis with communication to the overlying skin in a 14-year-old male neutered domestic shorthair. A, The cat had a 1-year history of sneezing and a 2-month history of a mass on the bridge of the nose. B, Computed tomography revealed a nasal cavity mass with nasal bone destruction and involvement of the subcutaneous tissues.
Sporotrichosis
Etiology and Epidemiology
Clinical Features
Group
Subcategory
Relevance to Cats and Dogs
Cutaneous
Fixed (or localized)
Lymphocutaneous
Multifocal (or disseminated)
All forms described in cats and dogs, but fixed or multifocal disease most common
Mucosal
Ocular
Nasal
Other
Occurs in cats and dogs
Extracutaneous
Pulmonary
Osteoarticular
Meningeal
Generalized (or disseminated)
Pulmonary and generalized disease is primarily described in cats. Pulmonary, generalized, and osteoarticular disease occur rarely in dogs.
Special forms
Spontaneous regression
Hypersensitivity (erythema nodosum, erythema multiforme)
Spontaneous regression has been described in cats and especially dogs

A, 2-year-old female spayed Bengal that had ulcerated lesions of the face, thoracic limb, and tail. B, Cutaneous and conjunctival sporotrichosis in a 1-year-old male neutered domestic shorthair. (Courtesy University of California, Davis, Veterinary Dermatology Service.)
Physical Examination Findings
Diagnosis
Laboratory Abnormalities
Serum Biochemical Tests
Diagnostic Imaging
Advanced Imaging
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sporotrichosis
Only gold members can continue reading. Log In or Register to continue