Harold C. MCKenzie III,
Severe Pneumonia and Acute Respiratory Distress Syndrome
Lower respiratory infections are a common problem in adult horses and foals, and can range from mild viral infections to severe, complicated bacterial infections. In general, bacterial lower respiratory infections have greater clinical impact because of the substantial risk for complications ranging from focal abscess formation to development of pleuropneumonia. The development of complicated pneumonia cannot always be prevented, but once present, it requires early and aggressive intervention to achieve acceptable outcomes. Severe pneumonia can present substantial therapeutic challenges to the clinician, requiring careful consideration of both patient factors and pharmacologic principles in the formulation of a therapeutic plan.
Inhaled or aspirated bacteria from the upper respiratory tract are the primary cause of bacterial pneumonia in adult horses, unlike the situation in neonates in which bacterial pneumonia is often of hematogenous origin. As a result, most adult respiratory infections develop initially on the surface of the respiratory mucosa and then progress to involve the pulmonary parenchyma. Pulmonary abscess formation can develop in situations in which physical and immunologic clearance of the infectious organisms is incapable of completely resolving the infection. Pleuropneumonia develops when inflammation-associated injury to the lung tissue secondary to bacterial bronchopneumonia breaks down the lung parenchyma and visceral pleura, allowing the infectious organisms access to the pleural space. When infection extends into this space, it is difficult to resolve because the immunologic response at this site is less effective, and the accumulation of inflammatory cells and serous fluid within the pleural space provides an expanding reservoir for infectious organisms. Severe pulmonary dysfunction can occur secondary to the overwhelming inflammatory response in the lung in association with severe infection or inflammatory insults, and can result in development of acute lung injury (ALI) or acute respiratory distress syndrome (ARDS). These syndromes necessitate aggressive, broad-based therapy and are associated with high morbidity and mortality rates.
Development of Disease
Horses appear to be at a somewhat heightened risk for developing lower respiratory disease for several reasons. First, horses and foals are typically managed in communal groups, allowing for the easy passage of viral and bacterial pathogens between individuals. Second, horses and foals are often transported for long distances, which results in impaired lower respiratory immune function and development of inflammation in the lower respiratory tract. The frequent introduction of new horses to the farm or stable environment also increases the likelihood of introducing pathogens into the local population of animals. Young foals are at higher risk for lower respiratory infections because of what appears to be innately poor cell-mediated immune responses early in life. Poor neonatal transfer of maternal immunoglobulins also plays a role in some cases.
The pulmonary inflammatory response normally acts to increase the ability to inactivate or eradicate infectious organisms or foreign material from the airways and alveoli, but this response also may have deleterious effects. Severe inflammation will result in alterations to airway and vascular tone that may impair the ability of the affected region of the lung to participate in gas exchange, or the accumulation of inflammatory debris and fluid may result in consolidation and the complete absence of gas exchange in the affected region. Normal compensatory responses can accommodate the loss of focal regions of gas exchange, but if the disease process is diffuse and severe, pulmonary function can be profoundly impaired, and the resulting hypoxemia and hypercapnia may be life threatening. For these reasons, the clinician must ensure that the treatment efforts not only address any primary pathogen but also support normalization of pulmonary function and resolution of pulmonary inflammation.
Diagnosis
The clinical signs of pneumonia may include fever, cough, nasal discharge, tachypnea, dyspnea, depression, inappetence, and pain on palpation of the thoracic wall (pleurodynia). The physical examination is key in determining the extent and severity of lower respiratory tract involvement, and this should include a rebreathing examination in most cases. The rebreathing exam greatly enhances the clinician’s ability to detect lower respiratory inflammation on auscultation, but should be avoided in patients that have severely increased respiratory effort at rest. Induction of a cough upon rebreathing is indicative of large airway inflammation or irritability. Abnormal breath sounds (e.g., crackles, wheezes, or rales) indicate lower respiratory tract inflammation, whereas the presence of very loud airway sounds or the absence of airway sounds may indicate consolidation of lung tissue or pleural effusion. Reluctance to move or signs of pleurodynia upon palpation or percussion of the chest wall may indicate pleural inflammation.
Clinicopathologic findings are important in evaluating the horse with lower respiratory tract disease because leukocytosis, neutrophilia, and neutrophilic left shift with or without hyperfibrinogenemia often accompanies progression of lower respiratory bacterial infections. Determination of serum amyloid A concentration may also be helpful in identifying pulmonary or systemic inflammation. Arterial blood gas analysis may reveal hypoxia and hypercapnia in patients with diffuse lower respiratory inflammation. Acute severe hypoxemia may be present, and in severe cases may be refractory to oxygen supplementation.
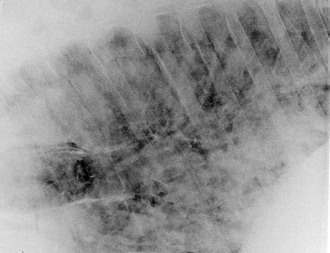
Imaging studies may aid in the staging and localization of lower respiratory infections, with ultrasonography being particularly useful in assessing the superficial pulmonary tissues and the pleural cavity. Ultrasonography may also have utility in monitoring foals for the early detection of pulmonary abscesses associated with rhodococcal pneumonia, and potentially allows for early institution of treatment (see Chapter 176). Thoracic radiographs are more challenging to obtain in adult horses but are easily performed in foals. Thoracic radiographs provide a more global assessment of pulmonary inflammation because they allow for evaluation of the lung tissue below the pleural surface. As a result, radiography is most useful in the detection of pathology deep within the lung, and can be critically important in the diagnosis of conditions such as pulmonary abscess formation, neoplasia, ARDS, and equine multinodular pulmonary fibrosis (EMPF) (Figure 60-1).
Although not usually required in the initial evaluation of patients with mild lower respiratory disease, airway cytology is critical in the assessment of severe or persistent lower respiratory infections. Airway cytology will provide a clearer indication of the character of pulmonary inflammation, especially regarding the predominant type of inflammatory cells and the presence and type of bacteria. For this reason, collection of a sterile tracheal aspirate is strongly indicated in patients that have undergone an unsuccessful course of antimicrobial therapy or those with evidence of severe lower respiratory infection. Tracheal aspirates are easily obtained in a sterile manner by either the percutaneous approach or the endoscopic approach, with a guarded endoscopic aspiration catheter used to obtain a fluid sample appropriate for culture.
Bronchoalveolar lavage (BAL) is less commonly used for the assessment of lower respiratory infections because of the potential for contamination during passage of the sampling tube through the upper respiratory tract, which renders culture results suspect. Despite this limitation, BAL can provide an important indication of small airway inflammation and involvement, and suspected focal pulmonary involvement is an indication for bronchoscopy and directed bronchial lavage. Thoracocentesis is indicated when pleural fluid accumulation has been confirmed with imaging (Figure 60-2). This procedure can have both diagnostic and therapeutic applications because it yields a sterile sample for cytology and culture while also removing fluid from the pleural cavity. Repeated airway cytology can also be useful in documenting changes in the status of lower respiratory inflammation and infection, but should not be required in most cases showing clinical resolution.

In horses with suspected diffuse lung disease, percutaneous lung biopsy may provide valuable diagnostic information. This information is not available from any other diagnostic tests short of postmortem sampling. The technique for percutaneous lung biopsy (Figure 60-3) is well described (see Suggested Readings), and is safe and effective when performed in appropriately sedated and restrained individuals. The diagnostic yield may be improved by sonographic identification of affected areas for sampling, but direct ultrasonographic guidance is not usually required. Use of an automated biopsy needle to perform this procedure appears to be safer and more effective than use of a manual biopsy needle.
Changes in clinical status often represent important indicators in the progression of lower respiratory infections, and these include persistence or worsening of fever, changes in the character of coughing, and signs of systemic inflammation. Deterioration in clinical status represents an indication for thorough reassessment, potentially to include physical examination, clinicopathologic evaluation, imaging studies, and collection of respiratory secretions for cytological assessment and culture.
Disease Syndromes
Although most viral lower respiratory infections are mild and self-limited in adult horses (e.g., equine influenza virus, equine herpesviruses types 1 [EHV-1] and 4 [EHV-4], equine arteritis virus, and equine rhinovirus), these infections may compromise the local pulmonary immune response and increase the risk for secondary bacterial pneumonia. This phenomenon is the result of damage to respiratory tissues, in combination with the accumulation of inflammatory debris and suppression of immune cell function in the lower respiratory tract. Secondary bacterial infections are a particular concern with influenza because of the adverse effects of this virus on the ciliated respiratory epithelium, which result in severe impairment of lower respiratory clearance. Some of these viral infections can be associated with severe clinical disease in foals. In neonatal foals, EHV-1 can cause severe and typically fatal pneumonia, with decreasing severity of disease associated with increasing age at the time of exposure. Although much less common, EHV-4 has also been implicated in some cases of severe neonatal pneumonia. Equine influenza virus has also been associated with severe pneumonia in neonatal foals, but again this is uncommon. Equine arteritis virus can cause rare fulminant infections in young foals, leading to interstitial pneumonia with a poor prognosis for survival.
Bacterial lower respiratory infections are the most common types of severe pneumonia, and these are typically caused by upper respiratory commensal organisms, most often Streptococcus equi subsp zooepidemicus. A wide variety of bacteria have been documented as pathogens in equine lower respiratory infections. With severe pneumonia, the clinician must be particularly concerned about the possibility of mixed bacterial infections of gram-positive and gram-negative aerobic bacteria, as well as anaerobes. Detection of pulmonary abscess or pleural effusion warrants suspicion of anaerobic involvement in adult patients. In foals, Rhodococcus equi infections may become severe and complicated, with extensive formation of pulmonary abscesses, and can progress to a syndrome of severe interstitial pneumonia with the potential for progressing to ALI and ARDS.
Fungal pneumonia is rare in the horse, and is often associated with immune compromise caused by either primary immunodeficiency or immunodeficiency arising secondary to severe systemic inflammation. Aspergillus organisms are the most common pathogens identified in fungal pneumonia, but several other organisms have been implicated in rare cases, including Cryptococcus gattii, Histoplasma capsulatum, Coccidioides immitis, and Candida albicans. Severe lower respiratory inflammation can also be associated with inhalation of inorganic materials (silicosis, lipoid pneumonia) and with apparently immune-mediated processes, including eosinophilic and interstitial pneumonias.
Interstitial pneumonia is a general descriptive term for any type of pulmonary pathology associated with pulmonary interstitial inflammation and fibrosis. Interstitial pneumonia has been described in foals and adult horses, and a broad range of etiologies appears to be possible. These include bacterial and viral agents, as well as toxins, neoplasia, and immunologic processes. Given the wide range of etiologies, it seems that there is a common pulmonary response to severe inflammatory insults, regardless of initiating cause. In foals, this syndrome has most commonly been associated with bacterial and viral etiologies, and affected animals present with severe respiratory distress and profound hypoxemia that is often refractory to oxygen supplementation. Most of these cases fall into the category of acute lung injury or, in the worst case, ARDS. Efforts should be made to identify and address the primary etiology while also providing respiratory support and addressing the severe pulmonary inflammation. Interstitial pneumonia is rare in adult horses, with the most well-described presentation being that of equine multinodular pulmonary fibrosis (EMPF; see Chapter 36). Horses with EMPF typically have weight loss, tachycardia, tachypnea, leukocytosis, neutrophilia, and hyperfibrinogenemia. Lower respiratory tract cytology demonstrates airway neutrophilia, but without evidence of bacterial infection. Thoracic radiographs demonstrate a diffuse, miliary to nodular pattern of increased density, whereas thoracic ultrasound will only demonstrate abnormalities when lesions are present near the pleural surface. Definitive diagnosis can only be made histologically, by obtaining either a lung biopsy specimen or postmortem samples of the lung tissue. Because EHV-5 appears to be associated with EMPF, polymerase chain reaction testing of lung tissue or BAL fluid is indicated. The prognosis for survival is guarded in any case of interstitial pneumonia, but with an aggressive treatment regimen that includes steroidal antiinflammatory drugs and appropriate respiratory support, it is possible for some horses to survive.
Acute lung injury and ARDS represent the most severe forms of lower respiratory inflammation and dysfunction. The first report of this type of disease syndrome in equids used the term interstitial pneumonia, rather than ALI or ARDS, but the clinical presentation that was reported appears very consistent with later studies that introduced the ALI and ARDS terminology. Affected animals present with respiratory distress and severe diffuse pulmonary infiltrates on radiography. Blood gas analysis in affected animals reveals profound hypoxemia and hypercapnia. The severity of the hypoxemia can be further defined by calculating the ratio of arterial oxygen tension to fractional inspired oxygen concentration (PaO2/FiO2). This calculation is performed by dividing the PaO2 in mm Hg by the FiO2 (0.21 in ambient air at sea level); and in normal horses breathing room air, one would expect to see a ratio of approximately 475 (PaO2 of 100/FiO2 of 0.21). On the basis of definitions used by consensus in human medicine, ALI is characterized by the following abnormalities: acute, severe hypoxemia (PaO2/FiO2 ratios from 200 to 300), diffuse infiltrates on thoracic radiographs, and the absence of signs of congestive heart failure. Cases of ARDS are characterized by FiO2/PaO2 ratios of less than 200 and diffuse infiltrates of thoracic radiographs, also in the absence of signs of congestive heart failure. It is important to realize the importance of these low PaO2/FiO2 ratios because a horse with a ratio of less than 200 will have a PaO2 of less than 42 mm Hg when breathing room air, which is likely incompatible with life without the support of mechanical ventilation, whereas a horse with a ratio of 300 will have a PaO2 of 63 mm Hg, which represents severe hypoxemia and a requirement for supplemental oxygen. A fundamental difference between equids and humans is that all human patients with ARDS will receive mechanical ventilation, but this intervention is only practical for foals in well-equipped neonatal intensive care units and is not practical for adult horses.