CHAPTER 13 Semen Quality
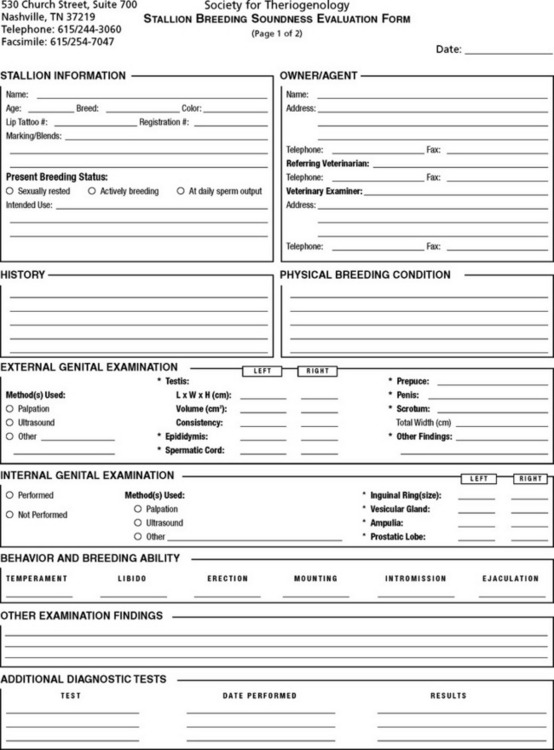
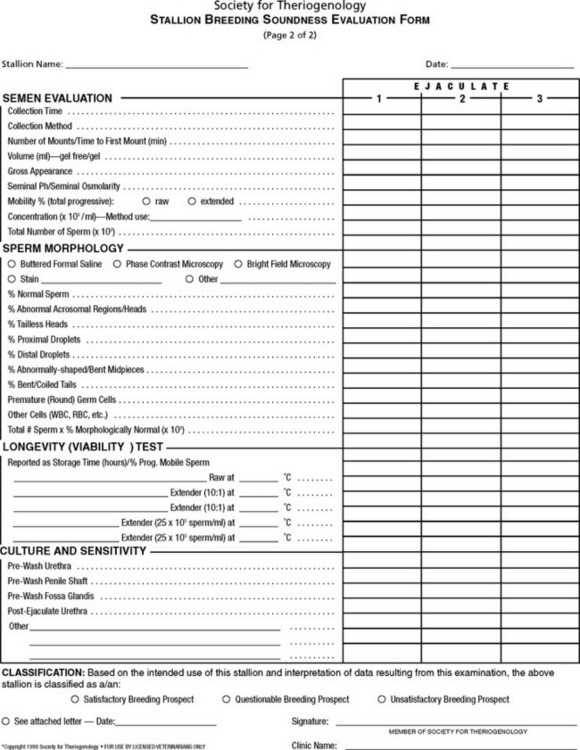
The Society for Theriogenology has established standards for a stallion’s breeding “satisfactoriness” or “soundness” (Fig. 13-1).1 To obtain a satisfactory rating on the examination for breeding soundness, the stallion must (1) be physically capable of mating; (2) possess good libido; (3) have normal external genitalia with scrotal or testicular dimension consistent with good sperm production; (4) test negative for infections and for venereal, bacterial, and viral pathogens; (5) have good semen quality; and (6) have at least 1 × 109 progressively motile, morphologically normal spermatozoa in the second of two ejaculates collected 1 hour apart, preceded by 1 week of sexual rest.2
The best semen samples to evaluate for breeding soundness are those that are representative of the stallion’s daily sperm output, that is, ejaculates collected after the extragonadal sperm reserve has been depleted.3 This usually requires 5 to 7 days of daily semen collection. Because this is both time consuming and labor intensive, however, most practitioners instead collect two samples 1 hour apart to evaluate stallion semen quality.
Conventional Methods
The gel fraction of the ejaculate can be removed either during the semen collection process by appropriate “in-line” filtration (eg, nylon micromesh filter) or after the sample has been collected in the laboratory. The entire ejaculate can be filtered through a sterile, prewarmed funnel that has one or two glass-wool cotton balls placed in the funnel neck to trap the gel from passing through the funnel. Alternatively, the gel in the ejaculate can be aspirated from the ejaculate using a sterile 60-ml syringe. Ejaculate volume (milliliters, gel-free portion) is usually measured in a prewarmed, sterile graduated cylinder (Fig. 13-2). Color and consistency of the ejaculate should be noted to allow estimation of the sperm number and detection of contaminants (eg, urine, blood, purulent exudate). Stallion semen should be an opaque-white color, and any deviation from this may indicate abnormality. Both urine (yellow color) and blood (red color) will damage spermatozoa if left in contact with the ejaculate for longer than 10 to 15 minutes.4
Concentration and pH
Sperm concentration is measured on the “neat” sample using a Neubauer hemacytometer (American Optical) (Box 13-1), a Makler chamber (Sefi Medical), or most often, photometric methods (Fig. 13-3). A photometric test evaluates optical density of the fluid sample, and therefore raw semen must be used to prevent false readings resulting from particles that may exist in common milk-based extenders.2,4 Cells other than mature spermatozoa (eg, red cells, neutrophils, round cells) may also falsely elevate the optical density reading. An accurate measurement (number of sperm per milliliter) is essential, since the evaluation of stallion semen quality and breeding soundness is based on available total sperm numbers in the ejaculate (gel-free volume × sperm concentration). This value is an estimate of total sperm number per ejaculate and is a crucial parameter in defining stallion semen quality and resultant breeding suitability (Table 13-1). Total sperm count can change depending on the season, frequency of ejaculation, testicular volume, incomplete ejaculation, extragonadal sperm reserves, and intrinsic reproductive tract disease or obstruction.
Box 13-1 Hemacytometer Method for Evaluating Concentration of Stallion Spermatozoa
Courtesy Oklahoma State University.
Unopette Method
Thoma Method
Large-Volume Method
Hemacytometer Preparation
Counting
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree