Chapter 11 Resorption of teeth is common in domestic cats. Tooth resorption has also been shown to occur in feral ( Verstraete et al. 1996; Clarke and Cameron 1997) and wild cats (Berger et al. 1996; Levin 1996). It has also been reported in dogs (Arnbjerg 1996) and in the chinchilla (Crossley et al. 1997). This chapter, however, will deal exclusively with tooth resorption in cats. Resorptive lesions (RLs) occur as a result of an external root resorption, where the hard tissues of the root surfaces are destroyed by the activity of multinucleated cells called odontoclasts. The destroyed root surface is replaced by cementum-like or bone-like tissue. The process starts in cementum and progresses to involve the dentine, where it spreads along the dentine tubules and eventually comes to involve the dentine of the crown as well as the root. The peripulpal dentine is relatively resistant to resorption and the pulp thus only becomes involved late in the disease. The process extends through the crown dentine, eventually reaching the enamel. The enamel is either resorbed or it fractures off and a cavity becomes clinically evident (Figs 11.1, 11.2A). Fig. 11.1 Clinical appearance of feline resorptive lesions Fig. 11.2 Clinical and radiographic appearance of resorptive lesions In the absence of routine radiography, the lesions are first noted clinically when they become evident in the crown, often as cavities at the cemento-enamel junction (CEJ). Figure 11.2B depicts the radiographic appearance of the clinical lesion seen in Figure 11.2A. The first clinical manifestation of a RL is thus a late-stage lesion. In many cases, the progressive dentine destruction with RLs weakens and undermines the crown to such an extent that minor trauma, e.g. during chewing, causes the crown to fracture off, leaving the root in the alveolar bone. The resorbing root remnants are usually covered by intact gingiva (Fig. 11.3). However, in some cases the overlying gingiva may be inflamed (Fig. 11.4). Fig. 11.3 Missing tooth with gingival overgrowth Fig. 11.4 Missing tooth with gingival inflammation Hard tissues (bone, cementum, dentine) are normally protected from resorption by their surface layer of cells (Lindskog and Hammarström 1980; Verstraete et al. 1998). Root resorption is classified as: External root resorption may follow any damage to the protective periodontal ligament (PDL) and cementoblast layer. It thus starts on the external root surface and progresses within the tooth. External root resorption (Andreasen 1988) is classified as: Surface resorption is self-limiting and reversible. It is thought that minor trauma caused by unintentional biting on hard objects, bruxism, etc. can cause localized damage to the PDL and cementoblast layer and trigger this type of resorption. The denuded root surface attracts clastic cells, which will resorb the cementum for as long as osteoclast-activating factors are released at the site of injury – usually a few days. When the resorption stops, cells from the PDL will proliferate and populate the resorbed area resulting in deposition of reparative dental tissue (Lindskog et al. 1983, 1987). The majority of human teeth show signs of active or healed surface resorptions. Replacement resorption results in replacement of the dental hard tissue by bone. The etiology of replacement resorption appears to be related to the absence of a vital PDL cover on the root surface (Andreasen 1985). It is assumed that damaged PDL is repopulated with progenitor cells from adjacent bone marrow. These cells establish themselves on the resorbed root surface and bone will thus be formed directly upon the dental hard tissues (Andreasen and Kristerson 1981). This results in fusion between bone and tooth, i.e. ankylosis. Replacement resorption can thus be seen as a form of healing: the bone has accepted the dental hard tissue as part of itself and the tooth becomes involved in the normal skeletal turnover, i.e. during subsequent remodeling of bone both dental hard tissue and bone will be resorbed (Hammarström et al. 1989). In PIRR, the osteoclast-activating factors, which keep the resorptive process going, are provided by an inflammatory lesion in the adjacent periodontal tissues (Andreasen 1985; Gold and Hasselgren 1992; Ne et al. 1999). PIRR occurs immediately apical to the marginal tissues and is thus often situated cervically. It has therefore also been termed cervical root resorption. EIRR, on the other hand, receives its stimulus for continued resorption from an infected necrotic pulp (Andreasen 1985). This type of root resorption is a complication that can follow dental trauma. It begins as a surface resorption due to damage to the periodontal ligament and cementoblast layer in conjunction with the traumatic injury. However, the pulp is also damaged by the trauma and becomes necrotic. As the surface resorption approaches the dentine, necrotic and possible infected pulp matter is released into the PDL from the thus exposed dentine tubules. The pulp products will then maintain an inflammatory process in the adjacent periodontal tissues that in turn will trigger the continuance of the resorption. The RLs seen so commonly in cats are external and either fit into the PIRR category or fit into the replacement resorption category. In other words, the RLs seen in cats are either inflammatory or non-inflammatory (replacement) in origin. In the literature, with the exception of one study (DuPont and DeBowes 2002) a distinction is not made between RLs of inflammatory origin and those that are truly idiopathic. This makes it difficult to draw meaningful conclusions. Prevalence rates ranging from 28.5% to 67.0% have been reported and the incidence increases with increasing age (Coles 1990; van Wessum et al. 1992; Verstraete et al. 1996; Lund et al. 1998; Lommer and Verstraete 2000; Ingham et al. 2001). Differences in breed susceptibility have also been suggested in some studies, but differences in the mean age among different breed groups make comparisons of significance suspect. The large variation in prevalence rates can be explained by the different populations of cats studied (random vs dental vs mixed) and by the different methods used to diagnose RLs (clinical vs radiographic). The incidence was generally higher in the studies where the cats examined were presented for dental examination or treatment than in the studies looking at random or mixed (i.e. presented for dental or other problem) populations of cats. However, in an Australian study looking at a mixed population of cats, 52% of cats were affected with a mean of 3.2 lesions per affected cat (Coles 1990). All types of teeth in the feline dentition may be affected by RLs, but lesions seem more common in certain teeth (Ingham et al. 2001). The manifest lesions can often be diagnosed clinically by visual and tactile examination. As already mentioned, they commonly present as a cavity at the CEJ of the tooth. Studies which included radiography (Lindskog and Hammarström 1980; Verstraete et al. 1998; Ingham et al. 2001) have demonstrated that the resorption can occur anywhere on the root surfaces, i.e. not only at the CEJ. Clinical methods will only detect lesions that involve the crown, while radiography will also detect lesions confined to the root. Thus, the prevalence of RLs in studies that include radiography is higher. In a study (Ingham et al. 2001) which investigated the incidence of RLs in a clinically healthy population of 228 cats (mean age was 4.92 years), using a combination of clinical examination and radiography, it was found that the overall prevalence rate was 29%. The mandibular 3rd premolars (307, 407) were the most commonly affected teeth and the pattern of RL development was symmetrical in most cats. The risk of having RLs was found to increase with increasing age and cats with clinically missing teeth were more likely to have RLs. Neutering, sex, age at neutering or mean whole mouth gingivitis index did not affect the prevalence of RLs. While the ongoing or established resorptive process has been detailed (Hopewell-Smith 1930; Okuda and Harvey 1992; Shigeyana et al. 1996), the etiology of many RLs is not clear. As previously described, it seems likely that at least two different types of resorption with different etiologies are currently diagnosed as the same condition. This is supported by the findings of a study (DuPont and DeBowes 2002) investigating the radiographic appearance of cat teeth with RLs. In the study 543 teeth with RLs were examined radiographically and two types of roots were identified. Type 1 roots had a normal root radiodensity and an intact PDL space (Fig. 11.5), whereas Type 2 roots were radiolucent and lacked a clear PDL space (Fig. 11.6). Of the 543 teeth that were examined, 268 (49.4%) were Type 1 and 275 (50.6%) were Type 2. Periodontitis was present in 72% of teeth with Type 1 roots, but only in 15.6% of teeth with Type 2 roots. Based on these findings it seems possible that Type 1 resorption is inflammatory and associated with periodontal disease while Type 2 roots are truly idiopathic.
Resorptive lesions
Introduction

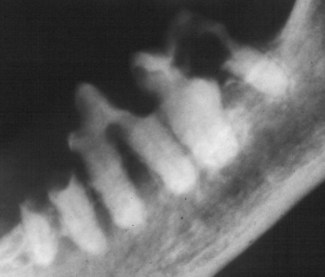
The lesions are first noticed clinically when they become evident in the crown, often as a cavity at the cemento-enamel junction. The process has extended into the crown dentine and come to involve the enamel, which has either resorbed or fractured off to reveal a small cavity filled with granulation-like tissue, at the buccal aspect of the gingival margin of the upper canine. Contrary to common belief, this is a late-stage lesion.

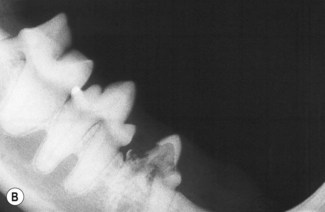
(A) Clinical appearance. The lower right 3rd premolar tooth has an extensive cavity at the cemento-enamel junction. The destroyed dentine and enamel have been replaced by connective tissue. Again, this is a late-stage lesion. (B) Radiographic appearance. The radiographic appearance of the right 3rd mandibular premolar tooth depicted in (A). Both roots show evidence of extensive resorption, i.e. loss of distinct periodontal ligament space, replacement of tooth substance by bone-like material, and most of the crown dentine is destroyed. This tooth requires treatment.

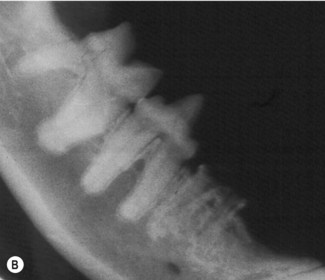
(A) Clinical appearance. The right mandibular 3rd premolar is absent on clinical examination. The overlying gingiva is not inflamed. (B) Radiographic appearance. The roots are retained in the alveolar bone. The roots are showing evidence of ongoing resorption. The only treatment required is clinical and radiographic monitoring, i.e. there is no indication to extract the retained roots.

In this patient, the progressive dentine destruction has weakened and undermined the crown of the right maxillary canine tooth to such an extent that minor trauma, e.g. during chewing, has caused it to fracture, leaving the root in the alveolar bone. The gingiva overlying the retained root remnant is inflamed. The retained root remnant needs to be extracted.
Resorption of hard tissue
Epidemiology
Etiology and pathogenesis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine