The full motion that a joint may be moved through is termed the ROM. The structure of the joint and the volume, integrity, character, and flexibility of the soft tissues that surround the joint affect joint motion.1 ROM is commonly measured with a goniometer, and each joint has characteristic angles, such as flexion and extension of the stifle, and flexion, extension, abduction, adduction, and internal and external rotation of the hip (Appendix 3). Muscles also have a ROM, which is termed the functional excursion of muscles.1 This is the distance that a muscle is able to shorten after it has been maximally elongated. The functional excursion may be affected by the joint it crosses, particularly if joint motion is restricted. Some muscles, such as the biceps brachii and the rectus femoris muscles, cross two joints. In general, muscles that cross multiple joints may lose functional excursion easier than those that cross only one joint. ROM exercises are useful to diminish the effects of disuse and immobilization.2 To maintain ROM, the joints and muscles must be periodically moved through their available ranges. Movement may be passive, active assisted, or active. In each situation, a load is produced on the soft tissues that helps to maintain the articular cartilage, muscles, ligaments, and tendons in a healthy state. It is generally appropriate to initiate passive ROM as soon after injury or surgery as possible provided there are no contraindications. Progression through active assisted and active ROM follows, and when appropriate, some resistance to motion may be introduced for strengthening. The benefits of continuous passive ROM immediately after joint surgery were initially described by Salter and colleagues3 and include decreased pain and improved rate of recovery. The scar tissue deposited after an injury or surgery is laid down in a random fashion, and ROM helps this scar tissue to align along the lines of stress that the tissue normally undergoes. This results in a stronger scar and may help prevent future injury. However, it is critical that the therapist maintain a ROM that is comfortable to the patient and not injure tissues by exceeding their limits. Passive ROM is used whenever a patient is unable to move joints on its own, or if active motion across a joint may be deleterious to the patient, such as with a tenuous articular fracture repair. Passive ROM is sometimes used to help relax an anxious patient. The most common indications for passive ROM exercises are immediately after surgery (before active weight bearing) to help prevent joint contracture and soft tissue adaptive shortening, maintain mobility between soft tissue layers, reduce pain, enhance blood and lymphatic flow, and improve synovial fluid production and diffusion.2 In some canine conditions, active ROM is a prerequisite to a successful outcome. For example, it is critical that puppies with distal femoral physeal fractures have early passive and active ROM exercises to avoid fracture disease and tiedown of the quadriceps muscle group.4 Similarly, dogs with condylar fractures of the distal humerus must begin active ROM to prevent permanent joint stiffness. In one study of dogs following surgery for cranial cruciate ligament rupture, patients not receiving early passive and active ROM exercises had reduced stifle extension (Figure 25-1).5 This loss of motion appeared to be permanent in some dogs if extension was not achieved within 2 weeks. In contrast, those dogs receiving appropriate rehabilitation had return of near-normal stifle extension. There also appears to be an association of stifle extension with weight bearing, with improved weight bearing in dogs with near-normal stifle extension (Figure 25-2). However, the cause and effect of this relationship are unknown. The association of stifle ROM with function following surgery for cranial cruciate ligament disease in clinical patients has been further evaluated.6 In 412 dogs treated with tibial plateau leveling osteotomy (TPLO) for treatment of cranial cruciate ligament rupture, dogs were determined to have no loss of extension or flexion (n = 322), less than 10 degrees loss of extension or flexion (n = 78), or 10 degrees or more loss of extension or flexion (n = 12). Loss of extension or flexion greater than 10 degrees was associated with significantly greater lameness in comparison with no loss, or loss of extension or flexion less than 10 degrees. In addition, osteoarthritis of the stifle joint was significantly correlated with loss of extension, and loss of extension greater than 10 degrees was less tolerable and less amenable to physical rehabilitation than flexion loss. The authors concluded that loss of extension or flexion should be assessed in dogs with persistent lameness after TPLO so that early intervention can occur. An explanation for the restricted ROM in clinical cases may include physical restrictions, such as joint capsule fibrosis, soft tissue approximation, or bony impingement that may occur with osteophytes as a result of joint disease. Another possible explanation is an increase in intraarticular pressure with joint motion, resulting in stretch of the joint capsule and creation of pain. One study evaluated the intraarticular pressure and volume relationships in the knee joint of dogs.7 In general, infusion of fluid into the joint did not result in intraarticular pressure changes between 125-110 degrees of stifle motion. However, increasing flexion from 110 to 50 degrees resulted in an increase in pressure, which was greater with increased intraarticular volume. Increasing the intraarticular volume also resulted in decreased total ROM of the joint. The functional and structural consequences of remobilization of the shoulder joint after 12 weeks of immobilization were studied in 10 beagle dogs.8 It was found that after 12 weeks of immobilization, the passive ROM was markedly impaired, intraarticular pressure increased during movement, and the filling volume of the joint cavity was reduced. On histologic examination, the capsule showed hyperplasia of the synovial lining and vascular proliferation in the wall, but there was no increase of collagen in the capsular wall. Both the functional and structural changes were unaltered after 4 weeks of remobilization, but after 8 weeks they began to reverse, and they returned to normal after 12 weeks, indicating that functional and structural changes after immobilization of an uninjured shoulder joint are potentially reversible. The timing and degree of improvement may not be similar in patients with pathologic injury to the shoulder. Another study of dogs evaluated the effects of joint mobilization treatment on carpal joints of dogs.9 The right carpal joints of 12 dogs were immobilized for 6 weeks, which resulted in joint hypomobility. The treated group received mobilization therapy daily for 4 weeks following the immobilization period. In control and treated groups, passive ROM, peak angles of extension and flexion of the carpal joint, and the amount of time required in the gait cycle to reach these peak points were evaluated cinematographically during gait before immobilization and once weekly for 4 weeks after immobilization. The treated group had improved passive ROM and motion during gait. Continuous passive ROM has been assessed in several studies to evaluate its use in the management of cartilage defects. Salter and colleagues10 demonstrated that young rabbits with a full-thickness defect in the articular cartilage managed with continuous passive motion had healing of 52% of the defects with hyaline-type cartilage. Similar results were obtained in adult rabbits, in which 44% of the defects were repaired with hyaline cartilage. Passive motion may also help to reduce cartilage destruction following infection of a joint.11,12 The optimal daily dose of passive ROM and the total duration of treatment are unknown. However, one study of rabbits found that at least 8 hours of passive motion per day was necessary to achieve the level of healing obtained by Salter.13 The effect of active motion on cartilage healing is unknown in animals because of the difficulty in achieving consistent limb use after cartilage injury. Continuous passive motion has also been recommended to prevent contracture of periarticular tissues and to restore joint function. Immobilization results in shortening of fibrous tissues and loss of motion, depending on the position of immobilization. There is a loss of collagen mass after immobilization, and there is collagen cross-linking of periarticular connective tissues, which may lead to increased stiffness. Passive motion may reduce these changes and prevent joint stiffness. In one study, 16 hours or more of continuous motion prevented increased joint stiffness following articular cartilage damage.14 Longer durations of passive motion may be necessary to help maintain normal quantities and turnover of collagen and glycosaminoglycans (GAGs), as well as to help maintain the normal alignment of collagen fibers and prevent shortening and cross-linking. It has been suggested that continuous passive ROM may be somewhat antiinflammatory in patients with inflammatory joint disease. In one study, the effects of continuous passive ROM on early inflammatory events were evaluated in meniscal fibrocartilage of rabbits with antigen-induced arthritis.15 Rabbit knees injected with bovine serum albumin and Freund’s complete adjuvant were treated with 24 or 48 hours of continuous passive ROM or were immobilized. Within 24 hours, immobilized knees had marked degradation of GAGs in meniscal fibrocartilage. Inflammatory mediators, including matrix metalloproteinase 1, cyclooxygenase 2, and interleukin (IL) 1b, increased within 24 hours and continued to increase. Knees undergoing continuous passive ROM had reduced GAG degradation and inflammatory mediators during treatment, and increased synthesis of the antiinflammatory cytokine IL-10. These results suggest that continuous passive ROM suppresses the deleterious effects of inflammatory arthritis more than immobilization and provide information regarding the involved molecular events. The duration of daily passive motion treatment has varying effects. For example, relatively short daily passive motion may reduce stiffness immediately after treatment, but there may be greater long-term stiffness.14 In fact, shorter durations of passive motion may be detrimental.14,16 One study indicated more stiffness with 10 to 30 minutes of passive motion per day than if the joints were immobilized,14 whereas another indicated increased stiffness with less than 8 hours of daily passive motion.16 Although somewhat surprising, these results suggest that there may be increased trauma associated with breakdown of soft adhesions that form when motion is not occurring, and that very frequent motion is necessary to keep the tissues mobile. Both continuous motion and as little as 4 hours of daily passive motion help to preserve muscle mass in rabbits.14,17 In fact, 5% to 15% greater limb muscle mass may occur in rabbits with passive motion as compared with those that are immobilized. The effects of passive motion on bone loss are less clear. It is well documented that immobilization results in a decrease in bone mineral content; however, 16 or 24 hours of passive motion resulted in the loss of greater bone mineral than immobilization.14 It was suggested by these authors that the increased joint stiffness that resulted from less than 16 hours of motion may have increased the bending stresses and load on the bones, whereas greater duration of passive motion maintained normal joint stiffness and prevented the additional loading on the bones. In people, the use of active and passive knee motion in the immediate postoperative period and a treatment plan for early postoperative limitations in knee motion has proven highly effective in restoring motion after anterior cruciate ligament reconstruction.18 In one study of 207 knees, 91% regained full ROM. The remaining patients did not regain motion as rapidly and were placed in an early postoperative phased treatment program of serial extension casts, early gentle manipulation under anesthesia, or arthroscopic treatment of intraarticular adhesions and scar tissue. Most of these patients regained full ROM. Those patients who failed to follow the rehabilitation program had permanent and significant limitation of motion. The incidence of postoperative motion problems was related to the extent of the surgical procedure. Patients who had more extensive surgery, such as a concurrent meniscus repair or a medial collateral ligament repair, had a higher incidence of restricted motion. It is recommended that patients have a muzzle applied for the initial treatments, or if they are painful, resistant to treatment, or overly anxious. The patient should be placed in lateral recumbency with the affected limb up (Figure 25-3). Help may be required to restrain the animal and to help keep it quiet and relaxed. In all forms of ROM activities, therapists should be comfortable and use proper body mechanics to avoid injury to themselves. After the hands are in the correct position and the limb is supported, begin by slowly and gently flexing the treated joint (Figures 25-4 to 25-7). In general, the other joints of the limb should be allowed to remain in a neutral position (a position as if the animal were standing). Try not to move the other joints while working on the affected joint because some joints may be restricted by the position of the joints above or below the target joint. In some situations, the position of one joint may greatly affect the motion in another joint. In these cases, the other joints should be placed in a position that will allow as complete a ROM as possible to the target joint. For example, maximal hock flexion cannot be obtained while the stifle is maintained in an extended position. In this case, placing the stifle in a flexed position allows more complete flexion of the hock. Slowly continue to flex the joint until the patient shows initial signs of discomfort, such as tensing the limb, moving, turning the head toward the therapist, or trying to pull away, but do not cause undue discomfort, indicated by behaviors such as vocalizing or attempting to bite. It is also important to maintain normal ROM in the other joints of the affected limb. After completing ROM of the affected joint, keep the limb in a neutral position and slowly move the hands distally to the digits (or if already working on the digits, move proximally). Be certain to keep the injured joint supported. Performing ROM of the digits requires additional consideration because it is difficult to passively flex and extend a single joint at a time because of the proximity of the other joints of each digit. In addition, it is more efficient to perform ROM in all joints simultaneously (Figure 25-8). Place the fingers or palm on the dorsal surface of the digits and slowly flex the digits until the point of initial discomfort. Then place the fingers or palm on the pads of the patient’s foot and slowly extend the toes until the point of initial discomfort. After ROM is performed on the digits, ROM exercises are performed on the other joints.
Range-of-Motion and Stretching Exercises

Range of Motion
Passive Range of Motion
Range of Motion Studies
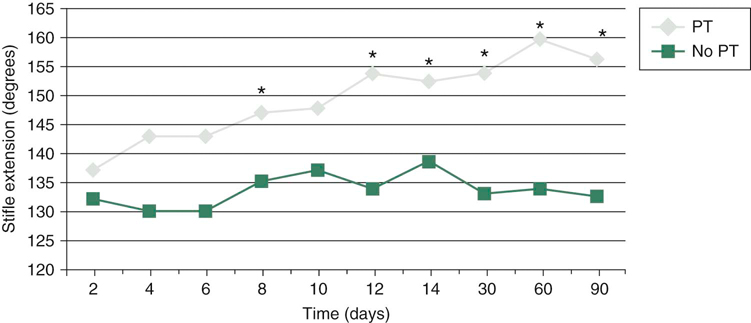
Figure 25-1 Effect of physical rehabilitation on stifle extension. Note the return of normal stifle extension by 2 weeks after surgery, in those dogs receiving rehabilitation and the loss of complete stifle extension in some dogs not receiving postsurgical rehabilitation. *P < 0.05.
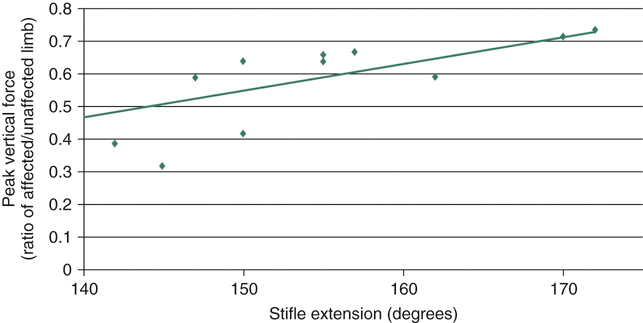
Figure 25-2 Correlation between stifle extension and peak vertical force. Relationship of comfortable angle of stifle extension to peak vertical force in dogs 10 weeks after cranial cruciate ligament transection and stifle stabilization. Dogs with normal stifle extension have greater weight bearing on the limb at a trot than those with limitation to stifle extension. Although a cause-and-effect relationship cannot be definitively identified from these data, there is a significant relationship. r = 0.78; P < 0.001.
Clinical Application of Range of Motion
Passive Range of Motion

Figure 25-3 Before performing range-of-motion or stretching exercises, the patient should be placed in lateral recumbency with the affected limb up.

Figure 25-4 A, Carpal flexion. While supporting the radius and ulna in one hand and the foot in the other, the carpus is gently flexed. B, Carpal extension. While supporting the radius and ulna in one hand and the foot in the other, the carpus is gently extended.
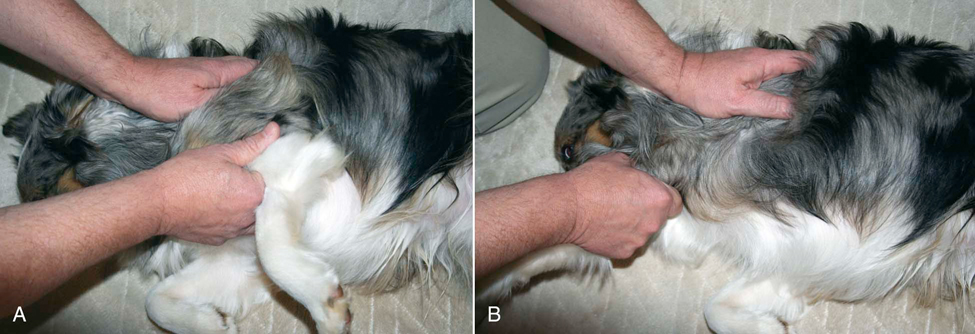
Figure 25-5 A, Shoulder flexion. While supporting the distal scapula in one hand and the humerus in the other, the shoulder is gently flexed. B, Shoulder extension. While supporting the distal scapula in one hand and the humerus in the other, the shoulder is gently extended.
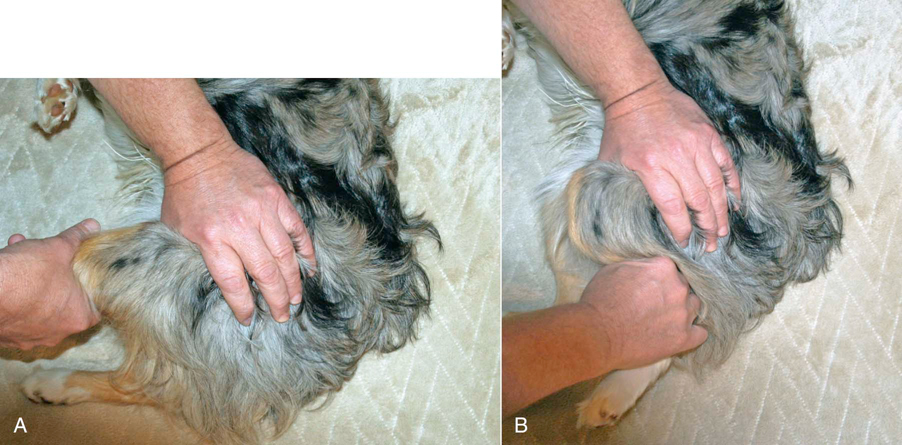
Figure 25-6 A, Stifle flexion. While supporting the distal femur in one hand and the tibia in the other, the stifle is gently flexed. B, Stifle extension. While supporting the distal femur in one hand and the tibia in the other, the stifle is gently extended.

Figure 25-7 A, Hip flexion. While supporting the femur in one hand and the pelvis in the other, the hip is gently flexed. B, Hip extension. While supporting the femur in one hand and the pelvis in the other, the hip is gently extended.
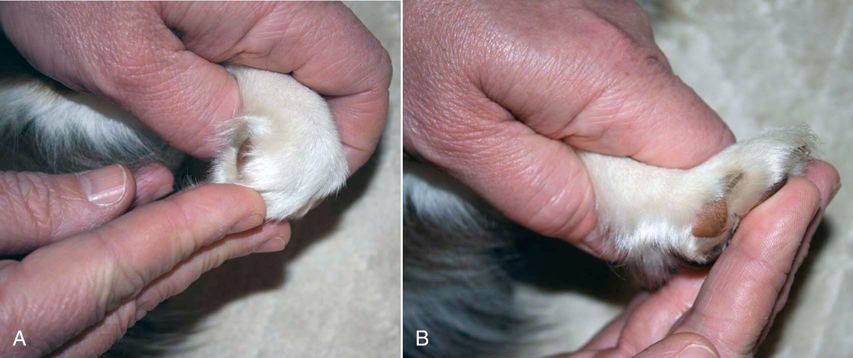
Figure 25-8 A, Digit flexion. While supporting the carpus in one hand and the digits in the other, the digits are gently flexed. B, Digit extension. While supporting the carpus in one hand and the digits in the other, the digits are gently extended.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


