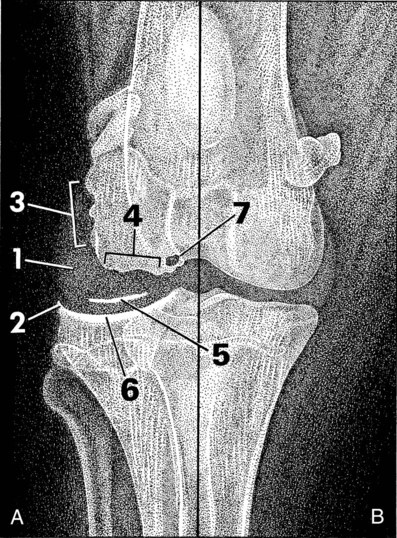
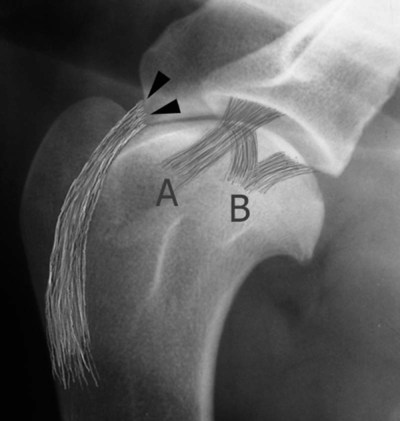
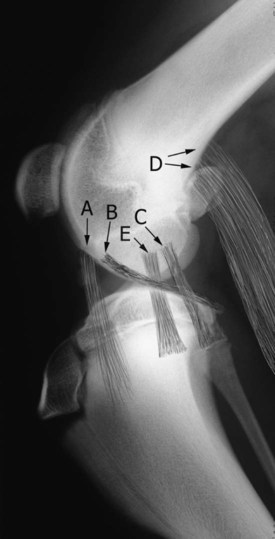
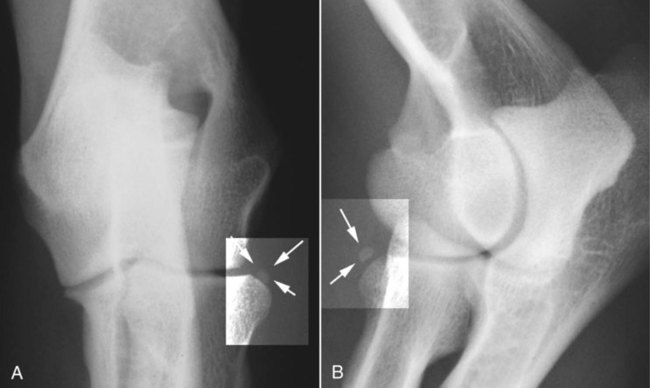
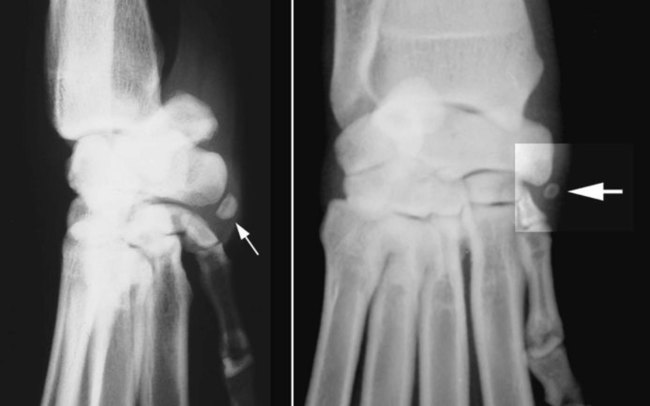
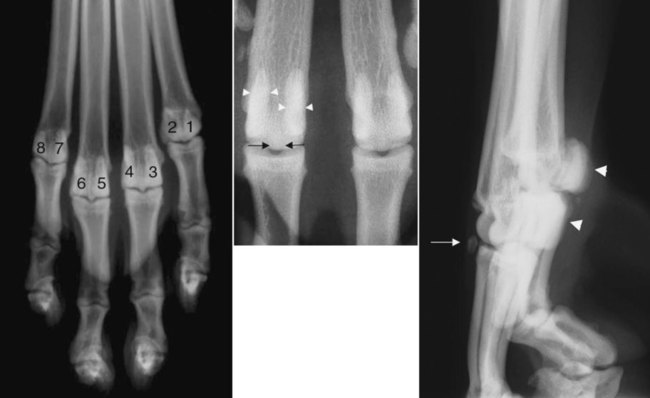
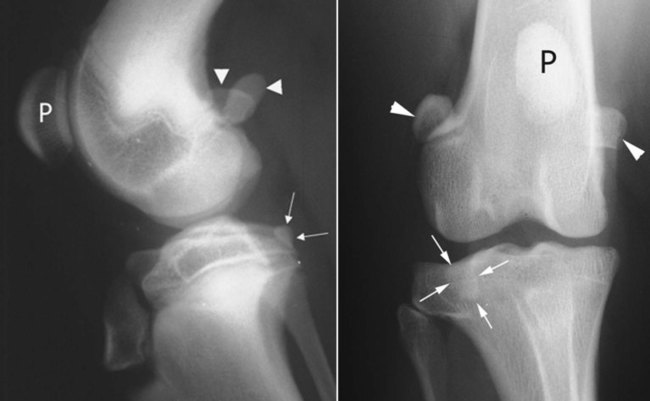
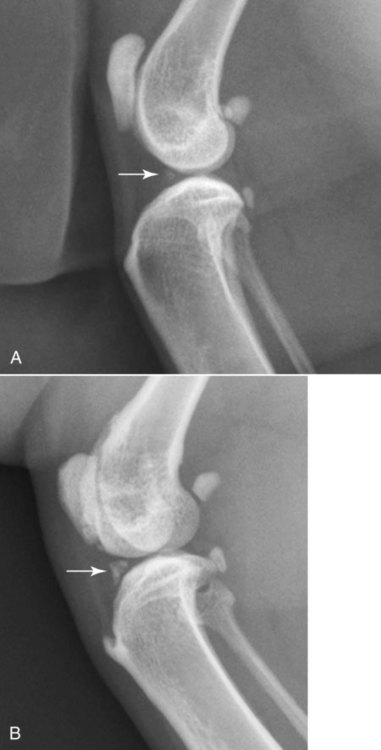
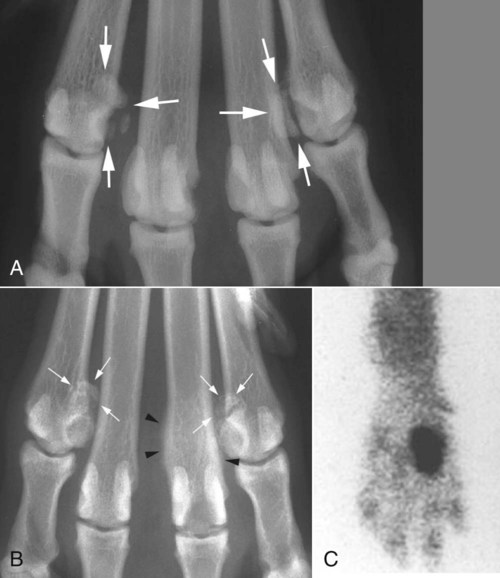
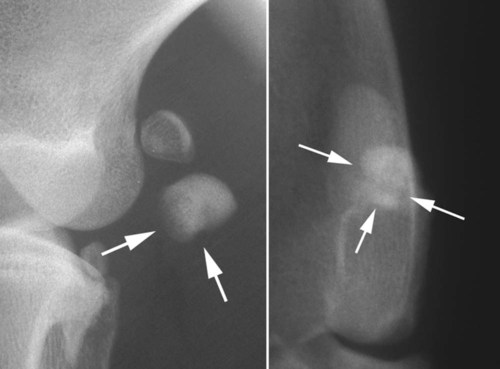
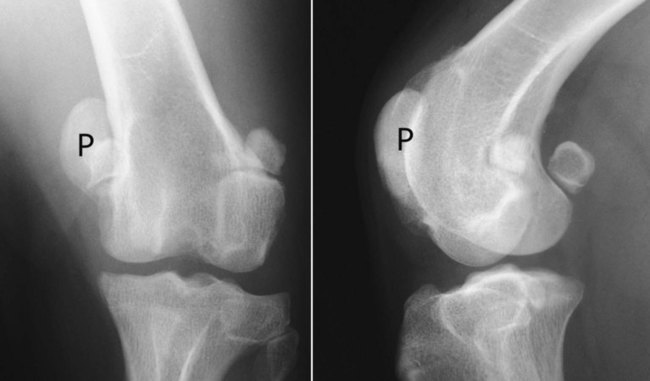
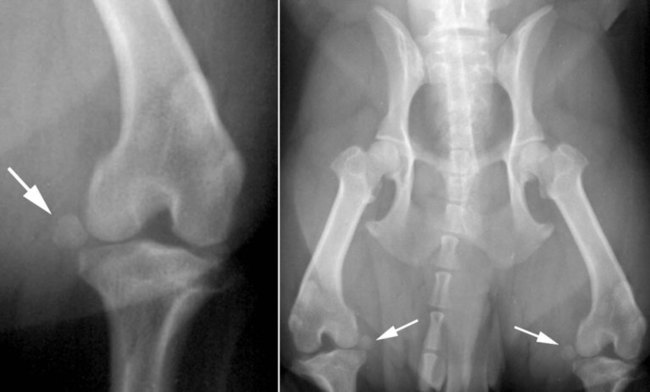
Most radiographic signs of joint disease are nonspecific (Box 18-1, Fig. 18-1). Also, animals with progressive joint disease may have different signs when examined during different phases of the disease. Sound knowledge of joint pathophysiologic characteristics is as important in the diagnosis of joint disease as is the ability to make and interpret radiographs of joints. In the stifle, the infrapatellar fat pad sign may be used to evaluate synovial volume. The normal infrapatellar fat pad is identified readily on lateral stifle radiographs as a relatively radiolucent triangular region immediately caudal to the patellar ligament (Fig. 18-2). When stifle synovial mass increases, either from increased synovial fluid or soft tissue, a combination of inflammatory response and effusion causes the fat pad to become less visible. The joint space is the region of soft tissue opacity between the subchondral bone of opposing weight-bearing surfaces of a joint. This space consists of two layers of articular cartilage separated by a microfilm of synovial fluid. In early joint disease, synovial effusion may cause widening of the joint space. As joint disease progresses, attrition of articular cartilage results in a thinning of the joint space (Fig. 18-3). These changes in joint space width are rarely diagnosed radiographically as a result of small animal patients not being radiographed while bearing weight and also because of inconsistency between the orientation of the primary x-ray beam and joint space. The subchondral bone is separated from the synovial fluid by an intact layer of articular cartilage. Any disease that changes the character of synovial fluid, causing the articular cartilage to erode, potentially threatens the integrity of subchondral bone.1,2 In inflammatory joint disease, inflammatory exudates may cause pronounced subchondral bone loss. Infectious arthritis may extend into subchondral bone. Subchondral bone loss appears initially as a ragged margin of subchondral bone, but it may extend to cause marked destruction of bone (Fig. 18-4). When bone loss affects smaller carpal and tarsal bones, these small cuboidal bones may be dramatically reduced in mass (see Fig. 18-4). Articular cartilage merges with the synovial membrane at the chondrosynovial junction. The highly vascular membrane is sensitive to inflammation. Synovial inflammation, or hypertrophy, may result in erosion of the bone adjacent to the synovium. Early inflammation causes the adjacent bone to appear ragged and spiculated. Longstanding or severe synovial inflammation or hypertrophy may cause pronounced bone erosion (Fig. 18-5). Mineralization may occur within the joint capsule, the synovial membrane, or synovial fluid as a consequence of chronic joint disease. Occasionally, large accumulations of articular or periarticular calcific material may be observed. Large osteochondromas have been reported within the joints of dogs3 and cats,4 and intrameniscal calcification and ossification have been observed in the stifle joints of cats.5 Pseudogout, or calcium pyrophosphate deposition disease, also causes mineralization of articular and periarticular soft tissues6,7 and has been reported in dogs. Small, well-defined articular and periarticular calcific opacities are occasionally observed in dogs and cats. Such mineralized fragments are sometimes called joint mice. Not all such fragments are free within the joint, although they may appear free radiographically; fragments may become adhered to the joint capsule. Articular calcified bodies usually fall into three fairly distinct categories: avulsed fragments of articular or periarticular bone, osteochondral components of a disintegrating joint surface, or small synovial osteochondromas (Table 18-1).8 They must be differentiated from sesamoid bones.9 Table • 18-1 Some Common Causes of Calcified Intraarticular Bodies In all joints, soft tissue periarticular mineralization may occur as a result of degenerative joint disease. When the normal spatial relation between the components of a joint is disturbed, some type of displacement has occurred. A good example is a luxated coxofemoral joint. Other less obvious incongruities, such as the cranial drawer sign in a stifle with a ruptured cranial cruciate ligament and minor elbow incongruity in dogs with elbow dysplasia, can be difficult to see radiographically.10,11 The proposed pathogenesis of osteophyte formation is that abnormal joint cartilage loading leads to cartilage wear, fibrillation, and loss of cartilage. The products of cartilage degradation mediate synovial hyperplasia and subsequent development of osteophytes.12 Initially, osteophytes consist of cartilage and later become radiographically visible when they are mineralized. They are seen as bony outgrowths at the periphery of articular cartilage. They occur as a component of degenerative joint disease (see Fig. 18-5). An enthesis is the point of insertion of a tendon, ligament, joint capsule, or fascia to bone. During embryogenesis ligaments or tendons are attached to cartilage, but subsequent metaplasia of fibroblasts at their attachment site results in formation of fibrocartilage. This extends into the tendon or ligament, and enchondral ossification proceeds within the remaining cartilage. Enthesitis is inflammation of the site of tendon or ligament attachment to bone. An enthesophyte is a bony spondylopathy that develops at an enthesis (Fig. 18-6).13 Because enthesophytes, osteophytes, and ankylosing spondylopathy appear radiographically similar, confusion in terminology often occurs when referring to these structures on a radiograph. To separate osteophytes around or within joints from enthesophytes, knowing the location of the common entheses is useful information (Figs. 18-7, 18-8, and 18-9). In complex joints such as the carpus and tarsus, a large number of intraarticular ligaments are present. Every diarthrodial joint has a joint capsule, and intraarticular and periarticular ligaments and joint capsules insert onto bone at their respective entheses. New bone formations arising in or around joints where no known entheses are present are usually referred to as osteophytes. Spontaneous or induced gas diffusion into a joint, termed the vacuum phenomenon, has been reported in both horses14 and dogs.15–19 It has also been observed within the intervertebral disc spaces of dogs that have a prolapsed disc. The presence of intraarticular gas is identified more easily during computed tomography examinations than during radiography.18 The theory is that noniatrogenic intraarticular gas represents diffusion of nitrogen from extracellular fluid into an adjacent joint space when negative pressure is present in the joint. This may occur naturally or be induced by applying traction to a joint. The vacuum phenomenon has many causes in dogs and cats (Box 18-2) and is observed when excessive distraction is applied to the coxofemoral joints during distraction radiography and has been reported in 20% of shoulder joint radiographs of dogs with osteochondritis dissecans (OCD) of the humeral head.16,17 Because traction is used during positioning of the shoulder for an OCD examination, gas diffusion is theorized to be induced by traction. Interestingly, gas diffusion was not a feature of normal (non-OCD) contralateral joints of dogs in this series.16 Positive clinical associations with intraarticular gas include degenerative disc disease, cervical vertebral instability, osteochondrosis, and degenerative joint disease (Fig. 18-10). Intraarticular gas diffuses slowly out of a joint over several hours after normal intraarticular pressure is reestablished. Sesamoid bones are present commonly adjacent to the elbow, stifle, tarsus, and the metacarpophalangeal and metatarsophalangeal joints. If sesamoid bones are not visualized on a radiograph, they may be absent or have not ossified at the time of radiography. The clavicle is present in up to 96% of large dogs and in all cats, but the sesamoids in the iliopubic cartilage were identified in only 11% of one group of greyhounds.20 In the same group of dogs, the elbow sesamoid, located in the tendon of origin of the supinator, had an incidence of 31%, the lateral plantar tarsometatarsal sesamoid 50%, and the intraarticular tarsometatarsal sesamoid 27%, whereas the popliteal sesamoid is ossified in 84% to 94% of dogs.21,22 Sesamoid bones are identified by their size, shape, and location (Figs. 18-11 to 18-18 [pp. 324-326], Table 18-2 [p. 327]). Occasionally, displaced sesamoids are regarded as a sign of muscular or tendinous injury. Although this may be true, and has been reported in conjunction with ruptured cruciate ligaments10 and trauma of the tendon of origin of the popliteus23,24 and gastrocnemius,25,26 variation in sesamoid location may also occur in the absence of a pathologic condition.27 Table • 18-2 Sesamoid Bones Visible on Radiographs of Joints of the Canine *Sesamoid bone located in the iliopubic cartilage may be seen cranial to the iliopubic eminence.20 A mineralized focus in the stifle joint is recognized commonly in domestic cats (Fig. 18-19, p. 327). Of stifle radiographs of 100 cats, 46 had meniscal mineralization detected in 1 or both stifles. Pain scores were not significantly different between stifles with meniscal mineralization and those without. Thirty-four of 57 cadaver stifles had meniscal mineralization, which was always located in the cranial horn of the medial meniscus. Percentage mineralization of the menisci was significantly correlated with the cartilage damage in the medial femoral and tibial condyles. Therefore, feline meniscal mineralization seems to indicate medial compartment degenerative joint disease.28 Although this mineralization has been thought of as a sesamoid bone, that is likely incorrect. Radiographs with added contrast medium, either air or water-soluble iodinated contrast medium, can be used to enhance visualization of intraarticular structures, such as the articular cartilage and synovium. A common use of contrast radiography was in the evaluation of the canine shoulder for evidence of osteochondrosis. Other applications include evaluation of capsular trauma, documentation of synovial hypertrophy, and identification of radiolucent-joint mice.29–33 Arthrography has been largely replaced by computed tomography and magnetic resonance imaging (MRI). A syndrome of metacarpophalangeal sesamoid bone fragmentation has been reported in several large breeds of dogs, but occurs most commonly in Rottweilers.33 The underlying cause appears to be osteonecrosis34 of selected sesamoids, although developmental, traumatic, and degenerative conditions are possible. Eight palmar/plantar sesamoids are present on the four main digits of each of the manus or pes, but sesamoid fragmentation affects mainly the second and seventh palmar sesamoids (Fig. 18-20, p. 328). The incidence has been reported to be as high as 44% in one group of Rottweilers.35 In another group of 55 Rottweilers, the radiographic incidence of sesamoid disease at 12 months of age was 73%, with an incidence of clinical signs attributable to sesamoid disease in 65% of affected dogs. Sesamoid disease was identified as the cause of forelimb lameness in 50% of young Rottweilers.36 Dorsopalmar radiographs usually allow identification of affected sesamoid bones, but oblique lateral projections with the digits separated by traction may provide additional information. Radiographically, fragmented sesamoid bones appear as a cluster of ossific fragments on the palmar aspect of the joint, adjacent to an unaffected paired sesamoid. The ossicles are usually multiple, with rounded margins that conform to a variety of shapes and sizes (see Fig. 18-20). In racing greyhounds, clearly defined transverse separation of sesamoid bones have been reported, leading to a belief that fracture is the cause of sesamoid fragmentation in this breed.37 Although less frequently than sesamoids in the manus, the fabellae are also prone to fragmentation (Fig. 18-21, p. 328). The most common example of sesamoid displacement is medial luxation of the patella (Fig. 18-22, p. 328). Patella luxation occurs most frequently in toy dogs and also in Devon Rex cats. Some breeds have an inherited predisposition to patella luxation. Other sesamoid bones are also prone to displacement. Distal displacement of the popliteal sesamoid or the fabellae has been cited as a sign that indicates rupture or trauma to their respective tendons, although this is not always true (Fig. 18-23, p. 329). Degenerative joint disease is a slowly progressive disease of synovial joints in which synovial effusion and cartilage degradation are key components. It is the most common joint abnormality seen in small animal practice and occurs most frequently in the weight-bearing joints of medium-sized to large dogs, although it may affect any synovial joint of both dogs and cats. The best example of canine degenerative joint disease occurs as a result of canine hip dysplasia. The incidence of hip dysplasia varies from breed to breed and in many large breeds exceeds 50%. The next most frequent locations of degenerative joint disease are the canine shoulder and stifle joints. Signs of shoulder degenerative joint disease were identified in 33% to 50% of groups of dogs surveyed either at necropsy or radiographically; 20% of dogs in another survey had evidence of stifle degenerative joint disease at necropsy.2,38,38 Degenerative joint disease may be a primary aging change (idiopathic) or as a result of a developmental or acquired disorder. Examples of canine developmental disorders include osteochondrosis, fragmented coronoid process, ununited anconeal process, hip dysplasia, patellar luxation, achondroplasia, and conformational disorders such as valgus and varus deformities of the carpus. Acquired disorders capable of causing degenerative joint disease in dogs include trauma, joint instability, epiphyseal aseptic necrosis, recurrent hemarthrosis, and acquired postural or conformational defects such as joint malalignment after fracture repair.40 The stifle joint is often used to study the progression of canine degenerative joint disease. The initial stages are asymptomatic, and radiographs are usually normal. The first change is mild nonsuppurative synovitis, accompanied by increased synovial mass. Focal articular cartilage degeneration follows. The joint space may be wider during this stage.41 Osteophytosis is the feature that is characterized by the greatest degree of change over time in the canine stifle with naturally occurring instability. When grading stifle degenerative joint disease, evaluating the changes in the number and size of periarticular osteophytes is more reliable than evaluating subchondral sclerosis, intraarticular mineralization, or synovial effusion, but signs of synovial effusion and compression of the infrapatellar fat pad are identifiable radiographic features that often accompany stifle instability. Early identification of osteophytes on trochlear ridges is facilitated by using specific radiographic projections, such as flexed mediolateral, craniomedial-caudolateral, and caudomedial-craniolateral radiographs.12,42–44 In the coxofemoral joint, synovial effusion may cause subluxation. The presence of subluxation is a powerful indicator of the risk of development of coxofemoral degenerative joint disease.45–49 There is a strong correlation between the unitless distraction index (DI), a quantifiable measure of subluxation, and subsequent development of degenerative joint disease. The likelihood of coxofemoral degenerative joint disease varies with breed and with the DI. Interestingly, the threshold DI, below which coxofemoral degenerative joint disease is unlikely to occur, is different for different breeds. The threshold DI for the German shepherd is 0.3, and it appears higher (0.4) for the Labrador retriever and Rottweiler. Radiographic changes of degenerative joint disease vary according to the stage of the disease. The most readily recognizable change is enthesophyte and osteophyte formation, which follows neovascularization of the chondrosynovial junction with resultant fibrocartilage formation. This fibrocartilage collar gradually ossifies with the formation of perichondral new bone (Fig. 18-24). Enthesophytes develop on non–weight-bearing surfaces and are eventually incorporated into adjacent ligamentous or capsular attachments.37,38 Thinning of the joint space is observed rarely (see Fig. 18-3). Pathologic alteration of subchondral bone may be detected as increased subchondral opacity of the weight-bearing surface (see Fig 18-3). Subchondral cyst formation, a feature of degenerative joint disease of the human femoral head, has also been observed in joints of small animals (see Fig. 18-5).2,50 Affected joints exhibit decreased range of movement, which results in increased loading of the diminished weight-bearing surface. The combination of increased load, diminished subchondral strength, and loss of shock-absorbing cartilage results in alteration in the shape of the subchondral bone table. This remodeling of subchondral bone is complemented by the addition of peripheral new bone in the form of perichondral osteophytes. Altered shape of the osseous components of affected joints is readily identified radiographically.50 The gamut of the radiographic changes seen in degenerative joint disease is outlined in Box 18-3. Primary causes of articular cartilage degeneration and consequent degenerative joint disease in cats include the storage disease mucopolysaccharidosis and osteochondral dysplasia of Scottish Fold cats. Established secondary causes of feline degenerative joint disease (Fig. 18-25) include developmental and traumatic conditions that alter joint stability as well as dietary (hypervitaminosis A) causes. Many infectious and immune-based arthropathies alter the integrity of articular cartilage, leading to a cascade of articular changes, with degenerative joint disease as the end result.51 Radiographic prevalence of signs of degenerative joint disease in cats older than 12 years of age is as high as 90%, which is far greater than the incidence of clinical signs of degenerative joint disease in older cats.
Radiographic Signs of Joint Disease in Dogs and Cats
Radiographic Signs of Joint Disease
Increased Synovial Volume
Altered Thickness of the Joint Space
Decreased Subchondral Bone Opacity and Bone Cyst
Altered Perichondral Bone Opacity
Articular Soft Tissue Mineralization
Intraarticular Calcified Bodies
JOINT
ETIOLOGY
Shoulder
Osteochondritis dissecans (OCD) of the head of the humerus
Mineralization of the bicipital tendon/sheath
Synovial osteochondroma
Separate centers of ossification on the glenoid rim
Elbow
Ununited anconeal process
Fragmented coronoid process
OCD of the humeral medial condyle
Hip
Avulsion epiphyseal fractures after femoral luxation
Avascular necrosis of the femoral head
Stifle
OCD of the femoral condyles
Avulsion fractures of the:
Origin of the long digital extensor tendon
Origin or insertion of the cruciate ligaments
Origin of the popliteus
Meniscal calcification
Synovial osteochondroma
Fragmented or fractured sesamoid bones
Tarsus
OCD of the talus
Joint Displacement or Incongruency
Osteophytes
Entheses and Enthesophytes

Intraarticular Gas
Sesamoid Bones
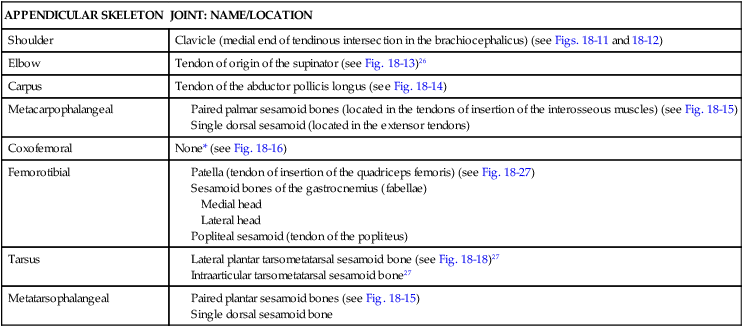
APPENDICULAR SKELETON
JOINT: NAME/LOCATION
Shoulder
Clavicle (medial end of tendinous intersection in the brachiocephalicus) (see Figs. 18-11 and 18-12)
Elbow
Tendon of origin of the supinator (see Fig. 18-13)26
Carpus
Tendon of the abductor pollicis longus (see Fig. 18-14)
Metacarpophalangeal
Coxofemoral
None* (see Fig. 18-16)
Femorotibial
Tarsus
Metatarsophalangeal

Meniscal Ossicles in Cats
Contrast Radiography of Joints
Sesamoid Disease
Degenerative Joint Disease
Radiographic Signs of Progression of Osteoarthritis in Dogs
Osteoarthritis in Cats
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiographic Signs of Joint Disease in Dogs and Cats