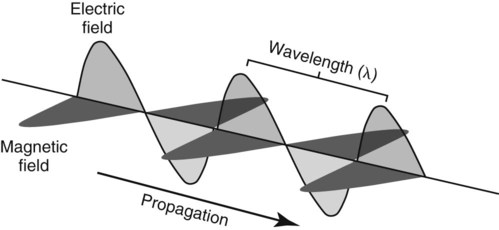
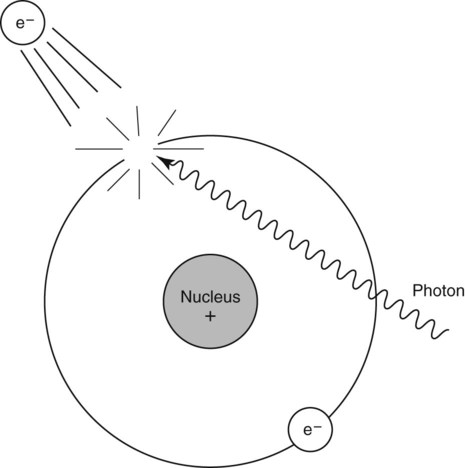
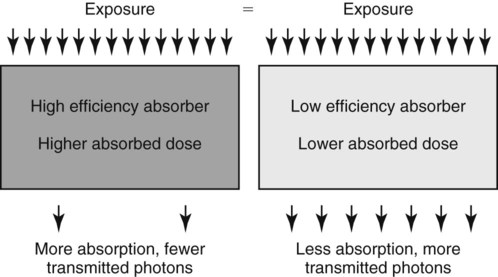
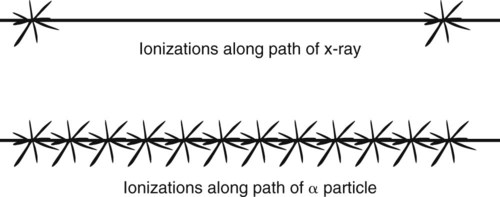
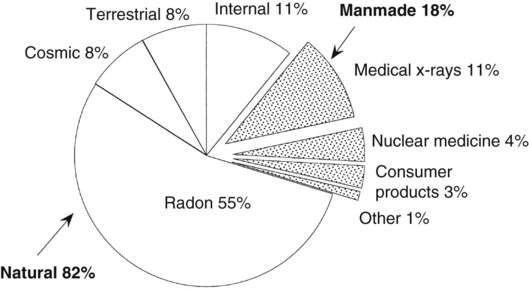
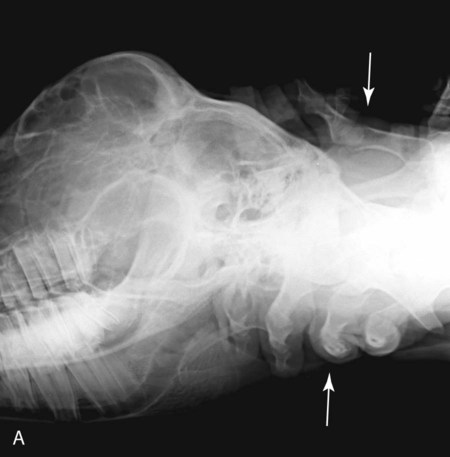
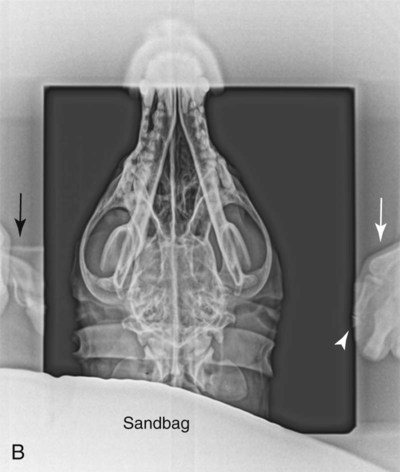
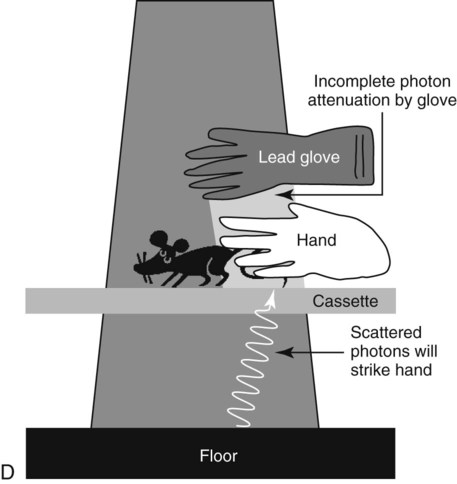
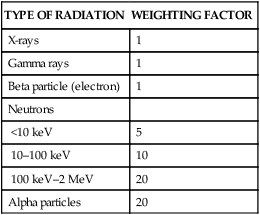
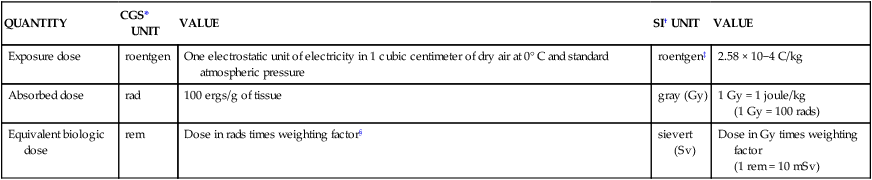
X-rays were discovered on November 8, 1895, by Wilhelm Conrad Roentgen, a German physicist.1 This new modality was put to use quickly for medical purposes, and many sophisticated medical applications were soon devised. For example, angiography was described in 1896, only 1 year after the initial discovery of x-rays. Roentgen’s finding revolutionized the diagnosis and treatment of disease, and in recognition he was awarded the first Nobel Prize for Physics in 1901. More than 110 years after their discovery, x-rays remain in widespread use for radiography and computed tomography in people and animals. X-rays and gamma rays are part of the spectrum of electromagnetic radiation. The only distinction between x-rays and gamma rays is their source; x-rays are produced by electron interactions outside the nucleus, and gamma rays are released from unstable nuclei having excess energy. There is a tendency to believe that gamma rays are more energetic than x-rays, but this is not true universally. The energy of a gamma ray depends on the amount of energy released by an unstable nucleus, and the energy of an x-ray depends on the energy of the electron that interacts with an atom. Familiar types of electromagnetic radiation other than x-rays and gamma rays include radio waves, radar, microwaves, and visible light (Table 1-1). Table • 1-1 Wavelength of Common Types of Electromagnetic Radiation Electromagnetic radiation is a combination of electric and magnetic fields that travel together, oscillating in orthogonal planes in sine-wave fashion (Fig. 1-1). Sine waves are characterized by two related parameters—frequency and wavelength. The velocity of electromagnetic radiation is constant, at the speed of light, and is the product of the frequency and wavelength: Some physical properties of electromagnetic radiation cannot be explained adequately by the theories of wave propagation illustrated in Figure 1-1. Therefore the photon concept was developed to explain the apparent particulate behavior of x-rays and gamma rays. A photon can be considered as a discrete bundle of electromagnetic radiation as opposed to a wave. This makes it easier to understand how x-rays create an image or cause radiation damage. In this book, the terms x-ray and photon are used interchangeably. Properties of x-rays and gamma rays are given in Box 1-1. The energy of electromagnetic radiation is described according to the formula: The unit of energy for electromagnetic radiation is the electron volt (eV). One electron volt is the energy gained by one electron as it is accelerated through a potential difference of 1 V. On an absolute scale, this is a very small amount of energy. However x-rays with energy of only 15 eV* can produce ionization of atoms or molecules. Ionization occurs when an electron is ejected from the atom, in this case by an x-ray. This creates an ion pair consisting of the negatively charged electron and the positively charged atom (Fig. 1-2). The ejected electrons can damage DNA, leading to (1) mutations, (2) abortion or fetal abnormalities, (3) susceptibility to disease and shortened life span, (4) carcinogenesis, and (5) cataracts.2 Radiation damage to DNA can be thought of as being amplified biologically because DNA controls cellular processes that extend into subsequent generations of daughter cells. Although only 15 eV of energy is required for ionization of biologic molecules, the energy of x-rays used for medical imaging is much higher, and each photon can lead to multiple ionizations as its energy is dissipated in the tissue. It is important to appreciate the relative risk of biologic injury produced by x-rays or gamma rays compared to other types of electromagnetic radiation. For example, the wavelength of visible light is 10,000 times longer than the wavelength of x-rays, and the wavelength of radio waves is even longer (see Table 1-1). Because the energy of electromagnetic radiation is inversely proportional to wavelength, the energy of light waves and radio waves is many orders of magnitude lower than the energy of x-rays. Thus light and radio waves do not produce tissue ionization or DNA damage. This is not to say that other forms of electromagnetic radiation cannot create injury, such as tissue heating from microwaves, just that they do not lead to molecular ionization. A goal in diagnostic radiology is to obtain maximum diagnostic information with minimal radiation exposure of the patient, radiology personnel, and general public. This is achievable readily in light of the guidelines for safe practice that have been developed, and the technology available to reduce exposure to personnel. However, because x-rays cannot be seen or felt, the idiom “out of sight out of mind” has never been more applicable, and it is easy to disregard the potential danger associated with occupational x-ray exposure (Fig. 1-3). As a result, many veterinarians have developed a cavalier attitude regarding the hazards associated with ionizing radiation and put themselves and their employees at risk, from both medical and financial perspectives. General principles of radiation protection that can form the basis of a safe workplace are discussed later. Any specific recommendations made in this chapter are subject to overrule by local, state, and/or federal regulations. Two related concepts are important to understand before radiation units are considered. First, radiation exposure and radiation absorption are not the same. Some tissues absorb radiation more effectively than others, meaning that the same exposure dose can result in different absorbed doses. Second, the biologic effect of the same absorbed dose can also be different, being a function of both radiation type and energy. A numeric weighting factor or quality factor has been derived to estimate the difference in biologic effectiveness of various types of radiation (Table 1-2). Table • 1-2 Radiation Weighting Factor (Quality Factor) for Various Radiation Types Radiation exposure, radiation absorption, and dose equivalent, because of differences in radiation quality, each have their own unit of measure that was defined originally in the centimeter-gram-second (CGS) system of measures. In 1977 the International System of Units (SI units) was developed in keeping with the trend toward universal adoption of the metric system3 (Table 1-3). In general, the system of SI units has been ignored in the United States,4,5 and CGS radiation units are still used widely, which can be a source of confusion. Table • 1-3 *CGS, centimeter-gram-second system of units. †International System of Units. ‡Although the use of roentgen is allowable under the SI system, it is not itself an SI unit, and continued use is strongly discouraged by the National Institute of Standards and Technology. §Weighting factor is a radiation type-specific quantity that compares the ionization density of various types of radiation; see Table 1-2. Radiation exposure is quantified by the amount of electrical charge resulting from the ionization of air produced by the radiation flux. Radiation exposure is expressed in the SI system as coulombs* per kilogram of air (C/kg) (see Table 1-3). This SI unit of exposure is cumbersome; thus the previous term of exposure, the roentgen, is still used. One roentgen equals a charge of 2.58 C/kg in air. The efficiency of x-ray absorption in different materials can vary widely. Therefore the absorbed radiation dose in tissues with different absorption efficiencies will be different when the tissues are exposed to the same amount of radiation (Fig. 1-4). The SI unit for absorbed dose is the gray (Gy). The gray is the amount of radiation leading to absorption of 1 joule*/kg of tissue. Before SI units were accepted, the unit of absorbed dose was the rad, which is equal to 100 ergs†/g (see Table 1-3). The term rad is obsolete, but it is so engrained in the radiology lexicon that it has not been replaced universally by the Gy, its SI counterpart. By using appropriate conversion factors, it can be shown that 1 Gy = 100 rad. As noted earlier, the same absorbed dose, in Gy, from different types of radiation may not produce the same biologic effect. For example, damage from particulate radiation, such as an alpha particle‡ is greater on a Gy-for-Gy basis than damage from the same dose of x-rays (see Table 1-2). This is related to differences in ionization density for different types of radiation. A large charged particle, such as an alpha particle, creates many ionizations that are close together compared to a small lightly charged particle, such as an electron, or an x-ray that has no charge or mass (Fig. 1-5). Neutrons have no charge, but they have a large mass, and they too have a greater ionization density than x-rays. This greater ionization density leads to more biologic damage. Therefore deposition of 1 Gy from an alpha particle or a neutron does more biologic damage than deposition of 1 Gy from an x-ray. The difference in biologic damage from the same absorbed dose of various radiation types is estimated by the weighting factor, as described above (see Table 1-2). In the SI system, the unit of dose equivalency is the sievert (Sv); the Sv is derived from the product of the absorbed dose in Gy and the weighting factor. Before SI units were accepted, the unit of dose equivalency was the radiation equivalent in man (rem; see Table 1-3). The rem was derived from the product of the absorbed dose in rads and the weighting factor. Because 1 Gy = 100 rads, 1 Sv = 100 rem. Principles of radiation safety are based on establishment of guidelines to prevent undesirable and unnecessary exposure to ionizing radiation. The premise of radiation protection is that some low level of radiation exposure to radiation workers is permissible and will not lead to observable abnormalities or disease. Adverse effects can be classified as either deterministic or stochastic. Deterministic effects have a threshold. In other words, below some dose there is no effect, but above the threshold dose the severity of the effect is dose related. Radiation-induced cataracts are an example of a deterministic effect. Conversely, stochastic (random) effects have no dose threshold, and the severity of the effect is independent of dose. Radiation-induced cancer is an example of a stochastic effect.6 The International Commission on Radiological Protection (ICRP) is the primary international body focusing on protection against ionizing radiation. The ICRP is a registered charity and thus not a governmental organization. The ICRP provides recommendations and guidance on protection against the risks associated with ionizing radiation. Their recommendations are published four times each year as the journal Annals of the ICRP. The whole-body limit set by the ICRP for avoiding stochastic effects is 20 millisievert (mSv) per year, averaged over 5 years, with the provision that any annual dose should not exceed 50 mSv.7 In the United States, the National Council on Radiation Protection (NCRP) was chartered by Congress in 1964. Some of the objectives of the NCRP are to develop recommendations about radiation protection and to cooperate with the ICRP. The whole-body limit set by the NCRP for avoiding stochastic effects is 50 mSv per year with a lifetime accumulation not to exceed 10 mSv × age in years.8 The NCRP also recommends that no occupational exposure occur until the age of 18 years. Interestingly, neither the ICRP nor the NCRP has any jurisdiction to enforce its recommendations. In the United States, the Nuclear Regulatory Commission (NRC) is the agency officially responsible for defining federal exposure standards. The NRC has adopted the annual occupational radiation dose to individual adults as recommended by the NCRP, a maximum of 50 mSv (5 rem) per year.9 However, the NRC has not established an upper limit for cumulative exposure. Previously, the NRC recommended that cumulative exposure be less than 5 rem (50 mSv)/year x (n −18), where n is the age of the individual. This recommendation has been overruled in favor of the as low as reasonably achievable (ALARA) principle, which is discussed later. In addition to occupational exposure of radiation workers, the entire population is exposed continually to very low levels of radiation, both natural and manmade. A breakdown of relative exposure of the U.S. public to radiation by various sources was published by the NCRP in 1987 (Fig. 1-6).10 The average U.S. citizen receives 3.6 mSv (360 millirem [mrem]) annually. Of this, more than 80% is attributable to inhalation of radon gas. The relative levels of different sources of exposure vary on the basis of geographic location. For example, because of the greater altitude, exposure to cosmic radiation is higher in Colorado than in North Carolina, and household radon exposure is greater in eastern Pennsylvania than in most other areas of the United States. Radiation workers in veterinary practices must be aware of the risks of radiation. They should be skilled in patient positioning for radiography, machine operation, and image processing so that repeat studies are minimized. Workers should be instructed on the proper use and care of radiation protection equipment, such as protective aprons and gloves, and in the concepts of the ALARA principle.11 As noted earlier, rather than focusing on any particular dose limit, the ALARA principle is aimed at limiting one’s radiation exposure as much as possible. The major variables used in adhering to ALARA are distance, time, and shielding. The most effective personal shielding for radiation workers is lead-impregnated aprons, gloves, thyroid shields, and eyeglasses. Protective aprons and gloves designed for use in the x-ray room are usually 0.5 mm Pb equivalent. These devices are only effective if used routinely. Wanton disregard for routine use of lead aprons and gloves leads to massive and unnecessary personnel overexposure. When rushing to acquire images, especially of an unruly patient, staff may be tempted to forgo the use of protective aprons and gloves completely to position the patient and to intentionally place the unshielded hands in the primary x-ray beam. This is, of course, unacceptable and exemplifies the ultimate in poor radiation safety practice (Fig. 1-7, A; see Fig. 1-3). More commonly, when lead gloves are not used, the radiographer attempts to keep the unshielded hands outside of the primary beam, thinking that the collimator eliminates radiation exposure in this area. This is not true. There is always adequate radiation outside the primary beam to capture an image of parts of the patient or radiographer in that area, and this also leads to unnecessary and excessive personnel exposure (Fig. 1-7, B). Additionally, the hand will frequently end up in the periphery of the primary beam, leading to even higher exposure. In fact, in Figure 1-7, B the tip of a finger of the hand (white arrowhead) is in the edge of the primary beam, but the fingertip is not visible because of overexposure. Another common mistake is the belief that because lead aprons and gloves are very heavy, they must provide considerable protection and can be used to shield body parts within the primary beam. This is also not true. Lead aprons and gloves are designed solely for protecting against scattered radiation and must never be placed in the primary beam because they do not attenuate high energy primary photons. It is commonplace for radiographers to hold a body part in the primary beam without gloves and then cover the hand with a lead glove or apron. This is not adequate protection, and the hand will receive unnecessary and excessive radiation dose (Fig. 1-7, C). The effects of scattered photons from the floor of the x-ray room are also usually ignored, but these are an important source of scattered radiation (Fig. 1-7, D). Lastly, radiation protection gloves with a slit in the palm are available. Extending the fingers through the slit facilitates positioning but reduces the amount of overlying protective lead material and leads to excessive extremity exposure whether the hand receives primary or secondary radiation. The following are some reasonable responsibilities of the radiation supervisor: 1. Establish and supervise the implementation of written operating procedures for all employees involved with radiography. 2. Periodically review procedures to ensure conformity with local regulations. 3. Instruct personnel in proper radiation protection practices. 4. Oversee conduction of required radiation surveys and keep records of such surveys and tests, including summaries of corrective measures recommended or instituted. 5. Routinely observe and periodically test interlock switches and warning signals. 6. Ensure that warning signs and signals are properly located. 7. Ensure that all equipment is maintained in top-notch working order. 8. Determine the cause of each known or suspected case of excessive abnormal exposure and take steps to prevent its recurrence. 9. Train staff in proper radiographic positioning and restraint procedures.
Radiation Protection and Physics of Diagnostic Radiology
Basic Properties of X-Rays
TYPE OF ELECTROMAGNETIC RADIATION
WAVELENGTH (CM)
Radio waves
30,000
Microwaves
10
Visible light
0.0001
X-rays
0.00000001
Radiation Protection
Radiation Units
TYPE OF RADIATION
WEIGHTING FACTOR
X-rays
1
Gamma rays
1
Beta particle (electron)
1
Neutrons
<10 keV
5
10–100 keV
10
100 keV–2 MeV
20
Alpha particles
20
QUANTITY
CGS* UNIT
VALUE
SI† UNIT
VALUE
Exposure dose
roentgen
One electrostatic unit of electricity in 1 cubic centimeter of dry air at 0° C and standard atmospheric pressure
roentgen‡
2.58 × 10−4 C/kg
Absorbed dose
rad
100 ergs/g of tissue
gray (Gy)
1 Gy = 1 joule/kg
(1 Gy = 100 rads)
Equivalent biologic dose
rem
Dose in rads times weighting factor§
sievert (Sv)
Dose in Gy times weighting factor
(1 rem = 10 mSv)
Exposure
Absorbed Dose
Dose Equivalent
Radiation Safety
Practical Considerations
Shielding
Radiation Supervisor
Radiation Protection and Physics of Diagnostic Radiology