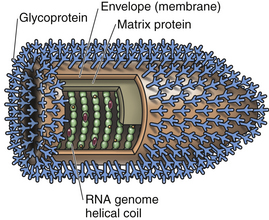
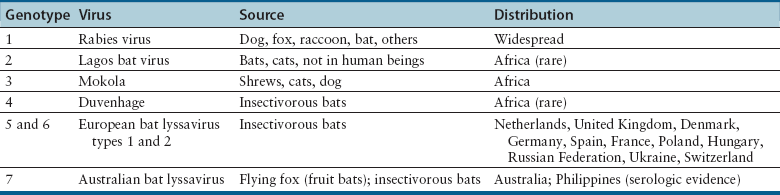
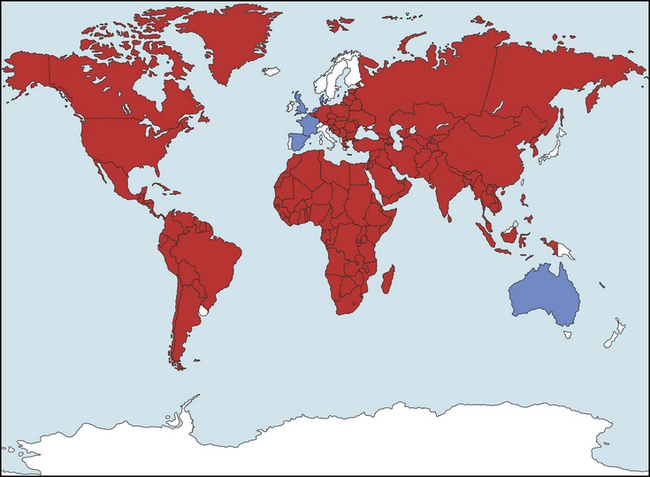
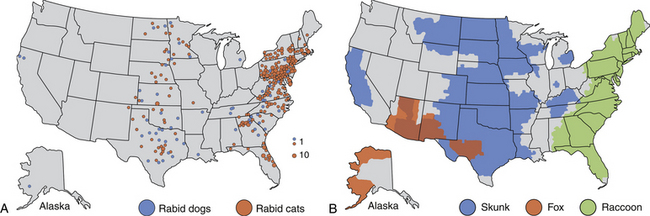
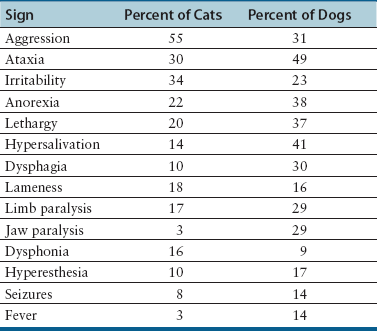
Chapter 13 Rabies is a deadly, zoonotic, neurologic disease caused by a bullet-shaped, enveloped RNA virus that belongs to the genus Lyssavirus (from Lyssa, the Greek goddess of madness, rage, and frenzy) (Figure 13-1). The virus is fragile in the environment, and readily inactivated by a variety of disinfectants, soaps, ultraviolet light, and heat. It can survive up to 3 to 4 days in carcasses at 20°C, and longer with refrigeration.2,3 Freezing tissues at temperatures less than −20°C may prolong survival of the virus for years. There are seven lyssavirus genotypes (Table 13-1). Classical rabies virus belongs to genotype 1. The remaining six lyssavirus genotypes primarily infect bats and less frequently cause fatal human encephalitis, which is clinically indistinguishable from classical rabies.4 Thus, although Taiwan, Australia, New Zealand, Iceland, the United Kingdom, Japan, most of western Europe, Fiji, Hawaii, and Guam are designated terrestrial rabies-free, lyssaviruses capable of causing fatal encephalitis in humans exist in some of these regions, including Australia, Western Europe, and the United Kingdom (Figure 13-2). The remaining information in this chapter pertains only to genotype 1 rabies virus infections. FIGURE 13-2 Global distribution of lyssaviruses. Distribution of rabies virus (red). Areas where rabies-related viruses only, and not classic rabies genotype 1, are documented are classified by the WHO as “rabies free” (dark blue). White areas are free of rabies and rabies-related viruses. (Redrawn from Warrell MJ, Warrell DA. Rabies and other lyssavirus diseases. Lancet 2004;363:959-969.) Infection with rabies virus most commonly occurs as a result of inoculation of virus-containing saliva into a bite wound, in the large majority of the cases after a dog bite. Other routes of transmission reported in species other than dogs and cats are rare and include corneal or solid-organ transplantation in human patients5; aerosol transmission, such as that occurring within caves containing large numbers of bats6,7; and transmission after ingestion of infected tissues or milk.6,8 All warm-blooded animals are susceptible to rabies, although dogs, wild carnivores, and bats are considered the main natural reservoirs of rabies virus. In general, wolves, foxes, coyotes, jackals, dogs, cattle, raccoons, skunks, bats, and mongooses are highly susceptible to infection. Moderately susceptible hosts include cats, ferrets, primates, sheep, goats, and horses. Marsupials, including opossums, have a low degree of susceptibility. Some bird species can be experimentally infected but do not develop clinical signs and are unlikely hosts.9 Not every bite from a rabid animal leads to rabies virus infection, and infection may not always culminate in death, unless clinical signs develop. Factors influencing the outcome after a bite from a rabid animal include the proximity of the bite site to the central nervous system (CNS), the degree of innervation of the bite site, the age of the host (young animals are more susceptible), the amount of virus inoculated, and the neuroinvasiveness of the rabies virus variant involved. If left untreated, up to 60% of humans bitten by a rabid dog on the head or neck develop rabies, compared with up to 40% of those bitten on the hand, and 10% of those bitten on the trunk or leg.10 Rabies viruses that circulate within a certain geographic region are adapted to specific dominant reservoir hosts (e.g., bat rabies virus variants or raccoon rabies virus variants). All rabies virus variants can infect and cause disease in animals other than their reservoir hosts (spillover hosts). In all host species, rabies is usually an acute fatal illness, although some animals, such as bats and skunks, have a more prolonged course of illness than others, such as foxes, coyotes, or raccoons. The possibility of a subclinical carrier state, especially in bats, has been suggested based on the detection of rabies virus antibody and, rarely, the virus itself in some reservoir host species that are not showing signs of illness.4 Over the past 50 years, owing to mandatory vaccination and control programs, domestic animal rabies in the United States has decreased in prevalence, whereas wildlife rabies has increased. The dog rabies virus variant was considered eradicated from the United States at the beginning of the 21st century. Currently, cats are more commonly reported with rabies in the United States (about 300 cases/year) than dogs (fewer than 100 cases/year), most likely reflecting rabies vaccination practices (Figure 13-3, A). No feline rabies virus variant has been described. The geographic distribution of feline and canine rabies follows that of regions where wildlife rabies is endemic. Most cats and dogs are infected with the rabies virus variant that is associated with the major wildlife reservoir host in their respective geographic location (see Figure 13-3, B). Rabid cats are most often reported from the northeastern United States, mid-Atlantic, and south-Atlantic states, with lesser numbers from the north and south central states. The eastern distribution of feline rabies follows the distribution of raccoon rabies.11,12 Rarely, cats are infected from bats. Rabies in dogs and cats is most commonly reported from the north central, south central, and Atlantic states (see Figure 13-3, A). Dogs may be infected with rabies virus variants from skunks or raccoons. Infected dogs have also been imported into the United States from other countries where canine rabies variants are endemic.13,14 In Europe, the major wildlife reservoir species have been foxes and raccoon dogs, and in South Africa, jackals and mongooses predominate. In western Europe, fox rabies has largely been eliminated as a result of mass vaccination campaigns. Spillover occurs from wildlife reservoir hosts to domestic animal species, which subsequently contact humans. Nevertheless, the vast majority of human cases in North America result from contact with infected bats, which are present in all states except Hawaii (see Public Health Aspects). Rabies in rodents and lagomorphs is rare, possibly because they are always killed by the bite of a rabid animal. In the United States, most reports have been from woodchucks in raccoon endemic areas.15 A few cases of rabies in pet ferrets, rabbits, and a pet guinea pig have been described.16 FIGURE 13-3 A, Reported cases of rabies that involve cats and dogs, by county, 2010. Histogram represents numbers of counties in each category for total number of cats and dogs submitted for testing. Note the overlap with the distribution of wildlife reservoir hosts in B. B, Distribution of major rabies virus variants among mesocarnivore reservoirs in the United States. (A and B modified from Blanton JD, Palmer D, Dyer J, et al. Rabies surveillance in the United States during 2010. J Am Vet Med Assoc 2011;239:773-783.) Although rabies occurs in cats and dogs of any age, it is most frequently reported in young dogs and cats, with a median age of 1 year for both cats and dogs in one study; 75% of animals were 3 years of age or younger.17 Rabies can occur in puppies and kittens that have not yet reached the age at which routine rabies vaccination is approved, which is an emerging issue as a result of illegal importation of pet dogs from Mexico through California and Texas. Male dogs may be slightly more predisposed, and most dogs and cats with rabies have not been neutered and live in rural environments, frequently being unrestrained at night.11,17 In the United States, some degree of seasonality occurs for rabies in dogs and cats, which correlates with seasonal increases in rabid raccoons and skunks.11,17 For the majority of cats and dogs with rabies, a history of known contact with wild animals or a wound is lacking. After inoculation into the subcutaneous tissues and muscle, rabies virus replicates locally within muscle cells and then attaches to peripheral nerve endings. Local replication around the bite site can continue for months before the virus enters peripheral sensory and motor nerve endings, with the nicotinic acetylcholine receptor being the main receptor for the virus. The virus then travels in a retrograde fashion up nerve axons at a rate of 3 mm/hr.6 Once the virus is within the CNS, there is massive viral replication, with cell-to-cell transmission of the virus across synaptic junctions. The spinal cord, medulla oblongata, periaqueductal gray matter, limbic system, and cerebellum are particularly affected. The virus also moves outwards from the CNS in somatic and autonomic nerves and is deposited in a variety of tissues, including cardiac and skeletal muscle, the eye, the kidney, pancreas, nerves around hair follicles, and the salivary glands. Production of new virions through budding from the plasma membranes occurs primarily within the salivary glands, which results in the shedding of virus that can be transmitted to other hosts. Thus, the presence of virus in the saliva indicates that the CNS has been infected. In some animals, death occurs before the saliva becomes infected. Virus is shed by some dogs for up to 13 days before the onset of clinical signs.18 Clinical signs probably result from impaired neuronal function6 and occur after an incubation period that ranges from just over a week to 6 months. Most dogs and cats develop disease 1 to 2 months after exposure. In general, the closer the bite site is to the CNS, the shorter the incubation period. The incubation period is also influenced by the host species, age, degree of innervation of the bite site, neuroinvasiveness of the rabies virus variant, and the amount of virus inoculated. Although 90% of humans develop disease within 6 months of exposure, incubation periods of 6 years or more have been reported.19–21 The clinical presentations of rabies virus infection have been divided into excitatory (“furious”) and paralytic (“dumb”) forms. Three phases have been described in the progression of the disease, the prodromal, furious, and paralytic phases, but the stages are variable and may overlap, and signs may be atypical (Table 13-2). Infrequently, there is a history of a wound, or wounds are still present at the time neurologic signs occur. Unfortunately, rabies is infrequently suspected as the possible diagnosis at the time rabid animals are examined by veterinarians.11,17 TABLE 13-2 Major Clinical Findings in 183 Cats and 119 Dogs with Rabies in the United States From Eng TR, Fishbein DB. Epidemiologic factors, clinical findings, and vaccination status of rabies in cats and dogs in the United States in 1988. National Study Group on Rabies. J Am Vet Med Assoc 1990;197:201-209. When it occurs, the prodromal phase lasts 2 to 3 days in dogs and 1 to 2 days in cats, and is characterized by a variable fever, licking or chewing at the bite site, and behavioral changes. Dogs and cats may become lethargic, anorexic, apprehensive, restless, or reclusive, and vomiting may occur.11 Some animals become more docile or affectionate. Pupillary dilation, sometimes with decreased pupillary light reflexes, may occur. The furious phase occurs in approximately two thirds of affected cats and dogs22 and lasts 0 to 7 days. Clinical signs result from forebrain involvement and include irritability, anxiousness or excitability, hyperesthesia, hypersalivation, vocalization, roaming, and aggression. Affected animals may try to eat foreign objects, which may become lodged within the gastrointestinal tract, or they may attack their surroundings or moving objects. Some animals develop ataxia, vestibular signs, and grand mal seizures. Tremors; staring, or a wild, spooky, or blank look in the eyes; increased vocalization; and compulsive running can occur cats, which also often develop aggressive behavior.11,17,23 The paralytic phase develops 1 to 10 days after the onset of clinical signs and is characterized by flaccid paralysis, which is ascending and often initially involves the bitten extremity. Neurologic examination reveals flaccid paralysis with absent segmental reflexes. Laryngeal paralysis may lead to a change in the sound or pitch of a dog’s bark or cat’s meow. Hypersalivation results from paralysis of the pharyngeal muscles, and a “dropped jaw” can occur as a result of masticatory muscle paralysis, especially in dogs, which may appear to owners as if they are choking. If euthanasia is not performed, coma and death usually occurs within a week of the onset of signs, with a few animals dying as long as 10 days after the onset of illness. Death is associated with multiorgan failure, especially cardiac and respiratory failure. Recovery from rabies is extremely rare. Experimentally, some dogs have recovered from clinical rabies days to months after being infected with certain rabies virus strains.24,25 Rabies should be suspected in dogs and cats evaluated for sudden onset of behavioral changes and flaccid paralysis, especially in rabies-endemic regions, or in animals imported from rabies-endemic countries. Although a particularly high degree of suspicion is warranted for animals that lack a vaccination history for rabies, the disease has been reported in partially and completely vaccinated dogs and cats,11,17,23 so a history of rabies vaccination should not be used to dismiss suspicion for rabies. No specific or characteristic hematological or biochemical changes have been reported in dogs and cats with rabies. Mild anemia was reported in one dog.26 Analysis of the cerebrospinal fluid (CSF) may be unremarkable or show an increase in CSF protein concentration and mild to marked CSF pleocytosis. Small lymphocytes account for most of the differential cell count.26 Electromyography in one dog revealed abnormalities consistent with impaired neuromuscular transmission, including moderate fibrillations, positive sharp waves, and an absent M wave.26 Changes suggestive of denervation have also been described in humans with rabies.27
Rabies
Etiologic Agent and Epidemiology
Clinical Features
Diagnosis
Laboratory Abnormalities
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree