CHAPTER 46 Pulmonary Hypertension
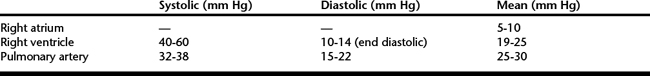
Pulmonary hypertension is characterized by high pulmonary artery pressure (PAP) that leads to impaired right ventricular performance and right-sided heart failure. Normal resting PAP in the adult horse is approximately 32 to 38 mm Hg in systole and 15 to 20 mm Hg in diastole, with a mean pressure of 25 to 30 mm Hg (Table 46-1). During exercise mean PAP correlates with speed of exercise and can reach 120 mm Hg in healthy Thoroughbreds running at maximal speed. There is no clear consensus as to what constitutes pulmonary hypertension in the horse, but systolic pressure greater than 40 mm Hg or mean pressure greater than 35 mm Hg in the resting horse would be in line with most published reports. Primary pulmonary hypertension is idiopathic, whereas secondary pulmonary hypertension results from any process that causes an increase in pulmonary vascular resistance, pulmonary venous pressure, or pulmonary blood flow. Primary idiopathic pulmonary hypertension is a diagnosis of exclusion and has not been characterized in the horse. Secondary pulmonary hypertension has been reported but not fully described in horses with left-sided heart failure resulting from mitral valve regurgitation, with recurrent airway obstruction and with congenital cardiac disease.
PULMONARY HYPERTENSION AND ACQUIRED HEART DISEASE
Pulmonary hypertension, when secondary to acquired cardiac disease, is usually the result of increased resistance to pulmonary venous drainage and subsequent pulmonary venous hypertension. Pulmonary venous hypertension occurs with diseases that increase left atrial or left ventricular end diastolic pressure or directly compress the pulmonary veins. Severe mitral valve regurgitation is the most common cardiac cause of pulmonary hypertension in the horse. Other acquired cardiac diseases affecting the left side of the heart, such as aortic regurgitation, left ventricular dysfunction, cardiomyopathy, constrictive pericarditis, and left atrial masses, can also cause pulmonary arterial hypertension. More direct obstruction of pulmonary venous drainage can occur in association with less common conditions, such as mediastinal masses and heart-base tumors. Aortocardiac fistula is an acquired cardiac defect that can cause pulmonary hypertension via volume overload similar to many congenital left-to-right shunts. Horses with pulmonary hypertension secondary to acquired heart disease are treated by managing the underlying cardiac disease with the use of appropriate heart failure medications, including positive inotropes, diuretics, and afterload reducers.