Chapter 25 Pulmonary Contusions and Hemorrhage
• Pulmonary contusions occur commonly in patients following blunt chest trauma. The contusions consist of interstitial and alveolar hemorrhage, accompanied by parenchymal destruction that starts immediately following the impact but can worsen for 24 to 48 hours after injury.
• The lesions typically resolve within 3 to 10 days, unless complications such as pneumonia or acute respiratory distress syndrome ensue.
• Clinical signs may be acute and severe or may develop progressively over several hours following trauma.
• The diagnosis of pulmonary contusions is based on a history of trauma and the presence of respiratory signs, ranging from tachypnea to respiratory distress, in conjunction with compatible blood gas abnormalities and characteristic changes on thoracic radiographs.
• Treatment of patients with pulmonary contusions is supportive and consists of oxygen therapy, judicious fluid administration, and analgesia for concurrent thoracic wall injuries. Ventilatory support may be necessary in severe cases.
• Less common causes of pulmonary hemorrhage include coagulopathies, thromboembolic disease, infectious disease (viral, bacterial, and parasitic), exercise-induced hemorrhage, and neoplasia.
DIAGNOSIS
Imaging: Radiology and Computed Tomography
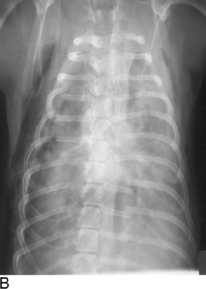
Radiographic changes in patients with pulmonary contusions consist of areas of patchy or diffuse interstitial or alveolar lung infiltrates that can be either localized or generalized (Figure 25-1). Radiographic changes may lag behind clinical signs by 12 to 24 hours and therefore “normal” radiographic findings may be seen in animals with pulmonary contusions. Patients with more severe radiographic changes initially may require a longer duration of oxygen supplementation and longer hospitalization times. However, the relationship between severity of the contusion based on radiographic changes and survival has not been established.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree