Chapter 14 Psychomotor Training and Virtual Reality
Surgical education∗ is essential for ensuring the safe and judicious use of new technology. Training in surgery involves cognitive knowledge, making accurate intraoperative decisions, and the acquisition of technical skills. This chapter will focus on skills development. Fitts and Posner defined a three-stage model for motor skill acquisition1: cognitive, meaning the surgeon understands the task; integrative, meaning the surgeon can perform the mechanics of the task; and automated, meaning that the surgeon performs the task with speed, efficiency, and precision. Achieving a high level of expertise is a goal of every good surgeon because this will result in delivering the best postoperative result for the patient.2
In human medicine, there has been an evolution in surgical training from the Halsteadean-apprenticeship model of “see one, do one, teach one” to a proficiency-based† curriculum.3 A number of factors have been responsible for this movement, and many of them apply to the field of veterinary medicine.4,5 With introduction of new technology, residents and students need to learn not only how to perform the traditional approaches but also how to perform them using the new technology. Recently, the American College of Veterinary Surgeons introduced a requirement for resident credentialing that involves performing a number of minimally invasive techniques. With somewhat limited exposure to minimally invasive surgery cases, the high costs of laboratory or operating room–based training, and ethical concerns regarding the use of animals or practice on client-owned animals, there is a definite need for computer-based educational programs and simulation technology to make psychomotor skills training more efficient and effective.
In human medicine, to meet these challenges for not only surgical residents but also for experienced surgeons who wish to learn new techniques, a number of surgeons and educators worked at developing skills training programs for minimally invasive surgery. Recognizing that “cut, sew, and tie remain the staples of surgical craft”6 and that the laparoscopic environment offered significant barriers to performing procedures7 (Table 14-1), the early pioneers first defined the skills that are needed in laparoscopic surgery. These needs were met by modeling exercises that can be carried out in a relatively low-cost box-type trainer. Several groups then developed systems for training, and among them, the McGill Inanimate System for Training and Evaluation of Laparoscopic Skills (MISTELS)8 and the Rosser Top-Gun training programs were two of the prominent programs.9 Skill development exercises focused on two-hand coordination, laparoscopic suturing, and gentle tissue handling in a three-dimensional (3D) environment visualized on a two-dimensional (2D) monitor.
Table 14-1 Psychomotor Challenges in Minimally Invasive Surgery
| Unique challenge | Implications for surgeon |
|---|---|
| Loss of 3D vision and fewer depth perception clues | 2D interpretation of 3D structures; must rely on shadows, light, tissue deformation, instrument angulation to determine depth |
| Diminished tactile feedback | Impaired judgment of forces applied or tissue consistency |
| Movements constrained | Depend on trocar position for triangulation at the surgical site |
| Ergonomic considerations: operator discomfort and fatigue, long instruments with unfamiliar handles | Select table height and port placement to keep shoulder and elbows in alignment; select proper instrument length |
| Fulcrum effect Paradoxic movements | Understand pivotal effect of body wall creating inverted movements (the hand moves right, the instrument tip moves left only when the camera is pointing toward the monitor) |
| Enhanced tremor: hand movements are magnified on monitor | Requires more intense focus on fine dexterity tasks |
| Reduced field of view, new anatomic viewpoint | Requires cooperation of surgical team to operate the camera to avoid iatrogenic injury and facilitate a smooth operation |
2D, Two-dimensional; 3D, three-dimensional.
Modified from Pellen MGCP, Horgan LF, Barton JR, et al: Construct validity of the ProMIS laparoscopic simulator, Surg Endosc 23:130-139, 2009.
Surgeon educators not only wanted to offer an environment for training but also desired to evaluate students’ performance in a more objective manner. An assessment methodology called Objective Structured Assessment of Technical Skills (OSATS), developed by Dr. Reznick at the University of Toronto and Dr. Fried at McGill University in Montreal, was introduced to improve an instructors’ evaluation of operative performance of surgical residents in open surgery.10 It was then later applied to laparoscopic procedures. In this assessment, instructors developed checklists of surgical tasks for each procedure and observed and graded students based on completion of the checklist. In addition, a global rating scale of operative performance based on tissue handling, knowledge and handling of instruments, time and motion analysis, flow of operation and use of assistants, and specific procedural knowledge was used to rate operative performance.11 Recently, a model for objective skills assessment has been proposed for cardiovascular surgeons that identifies a progression of skills in performing vascular anastomoses.12
Educators then developed metrics to quantify individual performance. The metrics were based on time for completion of each task, number of errors, and measures of surgical dexterity. To automate data recording and remove observer bias for evaluation of surgical dexterity, the Imperial College Surgical Assessment Device (ICSAD) and the Advanced Dundee Endoscopic Psychomotor Trainer (ADEPT) use tracking software to track the motion of the surgeons’ hands so that path length for the surgical instrument and the instrument movements can be recorded.13 In some cases, surgeons evaluate a final product with a measured end point such as the leakage pressure of a ligated vessel or intestinal anastomosis or the tensile strength of tied knots.14,15
The new assessment tools were then evaluated for validity and reliability.16 Construct validity was shown, and the training and assessment methods were demonstrated capable of differentiating novice, intermediate, and expert surgeons. External validity was proven, and the scoring system could be utilized by various test sites with similar results. Predictive and concurrent validity demonstrated a relationship between scores in the test system and technical skills measured in the operating room. The reliability (i.e., the consistency) of the tests was shown by demonstrating interrater and test–retest reliability. Ultimately, systems need to demonstrate an ability to separate competent from incompetent performance from a technical skills perspective; however, the concept faces a number of challenges.13
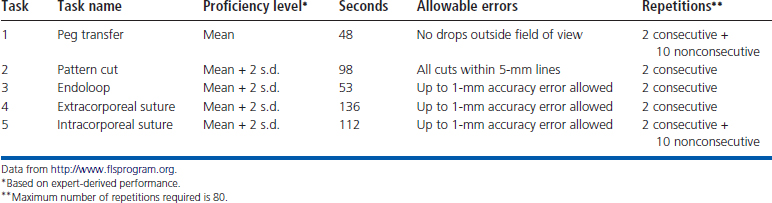
Today, the most commonly used system in training human laparoscopic surgeons is the SAGES Fundamentals of Laparoscopic Surgery (FLS).17 The program begins with web-based introduction and instruction, followed by practice in a box trainer to establish proficiency in five tasks: transferring pegs, cutting a pattern, placing an Endoloop, and performing extracorporeal and intracorporeal suturing. There are established proficiency levels for each task based on time, accuracy of cutting, dropping of pegs outside the field of view, accuracy of suture placement, and ability to perform the tasks consecutively (Table 14-2).
Table 14-2 Proficiency Levels and Training Protocol for the Fundamentals of Laparoscopic Surgery Curriculum
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


