Chapter 23 23.3 Assessment of the wounded horse 23.4 Detailed assessment of the wound 23.6 Methods of wound management 23.7 Primary (first intention) healing 23.8 Delayed primary closure (third intention healing) 23.9 Delayed secondary closure 23.10 Second intention healing 1. Incision. A wound produced by sharp objects, such as, intentionally with a scalpel or accidentally by glass, sheet metal, etc. The skin edges are cleanly cut with little tissue damage, and such injuries cause little pain. 2. Laceration. This is the most common type of wound and is characterized by irregular skin edges and extensive damage to underlying tissue. Such injuries cause considerable pain from bruising of tissues. When tissue has been lost, the laceration is termed an avulsion, and a laceration that extends into tendons, ligaments, synovial structures, or body cavities is referred to as a complicated wound. 3. Puncture. A wound produced by a sharp object that perforates tissue. These injuries may be complicated by the presence of dirt, manure, and other debris carried into the depths of the wound. There is considerable risk that a cavity, such as a joint, tendon sheath, bursa, abdomen, or thorax, may be perforated. Such wounds are easily trivialized; however, size belies severity. The entire thickness of skin has not been separated. 1. Abrasion (also referred to as a “graze”). Abrasions are friction injuries to the superficial surface of skin or mucous membrane and are characterized by oozing of serum and minimal haemorrhage; due to exposure of nerve endings these injuries result in considerable pain. Example: the donor site of a split-thickness skin graft. 2. Contusion. The result of bleeding and tissue destruction within and under intact skin without actual division of skin. 3. Burn. Exposure of skin to excessive heat (or cold or corrosive substances). Examples: Thermal burn, friction burn, chemical burn, freeze burn, and sunburn. Burns result in the coagulation of tissue proteins. • The general state of the horse should be assessed. • A history should be obtained and a thorough physical examination performed. • To assess the horse and evaluate the wound, the horse must be cooperative. Twitch, sedation, and regional, local or even general anaesthesia may be necessary. • Tetanus vaccination status should be determined. Appropriate protection should be instituted. 1. Administer tetanus toxoid if the horse is on a vaccination programme for tetanus and has not been vaccinated in the previous 6 months. 2. Idiopathic acute hepatic disease in horses (i.e. Theiler’s disease) (see Chapter 3) may be associated with administration of tetanus antitoxin. A lactating mare may be most at risk of developing Theiler’s disease after administration of antitoxin. Initial assessment and care of the wound have the single most decisive influence on healing. Knowledge of anatomy in the region of the wound is crucial in assessing the severity of injury. Consideration must be given to the location of the wound (Figure 23.1). 1. Injuries to the extremities frequently involve important underlying structures, such as nerves, major blood vessels, ligaments, bones, or joints. 2. To avoid contaminating an open body cavity or synovial structure, digital palpation of the wound should be delayed until the wound is cleansed and should never be performed without sterile gloves. 3. Nerves lie in close proximity to arteries and veins, and therefore, trying to clamp a bleeding vessel in a standing horse can be dangerous and is best avoided. 4. The wound should be evaluated for the degree of contamination and for the presence of foreign bodies. When invasion of a synovial structure is suspected: • A sterile, balanced electrolyte solution or a radiocontrast medium can be injected into the joint at a site remote from the injury (so-called synovial pressure test) (Figure 23.2). • Solution exiting the wound indicates that the joint has been penetrated. If possible, synovial fluid should be examined cytologically. Examine the horse for factors that prevent or impair healing. These include the following: 2. Contamination/presence of foreign body/sequestrum (Figures 23.3, 23.4). Figure 23.5 Non-healing wound over the dorsal tarsus – associated with excessive movement of the site. 8. General/systemic health disorder of the horse. 9. Tumour transformation (sarcoid) (Figure 23.6) (see Chapter 13). 10. Cutaneous habronemiasis (see Chapter 13). Also known as ‘summer sore’ or ‘granular dermatitis’, a granulomatous, mildly pruritic disease caused by cutaneous migration and encystment of the larvae of the equine stomach worms (Habronema musca, Habronema majus and Draschia megastoma). Larvae passed in the faeces are ingested by fly maggots, and after the maggots pupate, the larvae are deposited on wounds from the feeding flies. The condition appears in spring and summer, when flies are prevalent, and usually disappears with onset of cold weather. Cutaneous habronemiasis is characterized by exuberant granulation tissue that contains numerous, small, yellow, hard, caseous granules composed of eosinophils, nuclear remnants, and larvae. Affected horses may have a circulating eosinophilia. Lesions are resolved by eliminating the larvae with ivermectin or an organophosphate or by reducing the horse’s hypersensitivity to them with corticosteroids. 11. Pythiosis (see Chapter 13). This disease is caused by invasion of a protistal organism, Pythium insidiosum (formerly Hyphomyces destruens). The condition is characterized by a rapidly enlarging granuloma that contains sinuses filled with purulent, serosanguineous fluid and yellow granules, commonly referred to as ‘kunkers’ or ‘leeches’. Affected horses can be successfully treated with a vaccine made from P. insidiosum. Ancillary treatment includes systemic administration of sodium iodide and then organic iodide (ethylenediamine dihydroiodide). 12. Ehlers–Danlos syndrome (hyperelastosis cutis). A heritable dysplasia of connective tissue. Affected skin is hyperextensible, fragile, and prone to wounding with slight trauma. Malignancy that develops long after the original injury is described as chronic, or latent. Malignancy that develops soon after the original injury is described as acute. Latent malignancy is more common than acute malignancy. The most common type of malignancy induced by injury is the carcinoma, and the most common type of injury producing the malignancy is a burn. In general, the older the patient at the time of injury, the shorter the interval from injury to the onset of neoplasia. Cause may be persistent irritation from chronic infection and trauma to the poorly vascularized wound. Healing after each insult becomes more difficult, and regenerated epithelium becomes increasingly inferior. The prognosis for survival of horses with burn-induced neoplasia is poor because of a marked propensity for the neoplasm to metastasize. • Wounds elicit a consistent and orderly response by the body that restores continuity to injured tissue. Wounds move predictably down a common pathway of healing, and knowledge of the predictable events of healing can be used to decide steps in wound management. These phases are found in both sutured and unsutured wounds. • The sequence of events progresses through four overlapping phases. (a) Fibroblasts and capillaries appear in the wound by day 3. (b) Fibroblasts use the fibrin clot as a matrix and replace it with new matrix. (c) Fibroblasts lay down collagen and other components of connective tissue. (d) Granulation tissue is necessary for wound contraction and migration of epithelium. (e) Fibroblasts may proliferate in wounds of horses even after the wound has been filled with granulation tissue, but fibroblasts cease to proliferate in wounds of ponies when the wound is filled with granulation tissue. 1. The wound must be vascular. Suturing a wound caused by a sharp object is more likely to be successful than is suturing of a wound caused by blunt trauma. 2. Sutured wounds must have minimal tension. 3. Wound must be clean and non-infected. Infection is the main cause of dehiscence. Factors that affect the concentration required to cause infection: • Foreign bodies, such as sutures and drains or bone sequestrae, in contaminated wounds dramatically lower the concentration of bacteria necessary to cause infection. • Clean, insoluble material, such as glass, gravel, or metal cause less tissue reaction than do porous, contaminated, and organic material, such as grass, straw, and wood. • Soil increases the risk of infection. Infection-potentiating factors (IPF) are found in soil. The IPF have a high negative charge that inactivates leukocytes, which are positively charged. Clay and organic soil contain the most IPF, whereas sand has few. • Necrotic tissue and dead space dramatically lower the concentration of bacteria necessary to cause infection. • The concentration of some bacteria, most notably β-haemolytic streptococci and pseudomonads, required to infect a wound is much less than 105 per gram of tissue. When deciding whether to close a wound, the time that has elapsed between wounding and treatment should be given only modest consideration. For example, wounds of the head have a long grace period because the blood supply to the head is excellent, causing bacteria in a wound of the head to multiply slowly to the concentration of 105 organisms per gram of tissue. Soft-tissue wounds of the head can often be closed safely often 24 hours or longer after wounding (Figure 23.7). Bacterial quantitative analysis can be used to determine the concentration of bacteria in a wound. If a wound contains more than 105 bacteria per gram of tissue, the wound should not be sutured. Quantitative analysis is usually impractical because: Qualitative analysis is usually used to determine readiness for closure. • Soap interferes with defense mechanisms of the wound and when applied to contaminated tissue increases the wound’s susceptibility to infection. The detergent may drive bacteria deeper into the tissue. • Soap applied to uncontaminated fresh wounds irritates tissue but does not significantly increase the wound’s susceptibility to infection. 1. The guiding principle in surgical debridement is that, when excised, living tissue bleeds, and devitalized tissue does not. 2. The simplest method of debridement is to create a surgically clean wound by totally excising the wound (i.e. en bloc debridement). This can rarely be done in horses because horses do not have abundant soft tissue. 3. Usual method is to excise all grossly nonviable or damaged tissue with a scalpel. Superficial fascia is often a edematous making it easy to excise with a scalpel or Metzenbaum scissors. Surgically debriding wounds overlying critical structures, such as nerves, tendon sheaths, and joint capsules, is difficult. 4. If the wound contains much devitalized tissue or debris, the wound should be left open for delayed primary closure or to heal by second intention. 5. Rather than excising a flap of skin that appears to have an inadequate blood supply to survive, subcutaneous tissue can be sharply excised from the dermis, and the flap sutured in place to act as a full-thickness “skin graft”. 6. Curettage of exposed cortical bone (i.e. bone without periosteum) may be helpful in preventing formation of an osseous sequestrum. • Mechanically disrupts bacterial adherence in addition to removing foreign material. • Can be achieved with a 19-gauge needle and a 35-mL syringe or with a spray bottle. • Common concern during lavage is that high-pressure lavage may disseminate foreign material and bacteria from the surface of the wound into the depths of the tissue, but this concern is not justified.
Principles of wound management
23.2 Classification of wounds
Closed wounds
23.3 Assessment of the wounded horse
23.4 Detailed assessment of the wound
Suspected synovial involvement
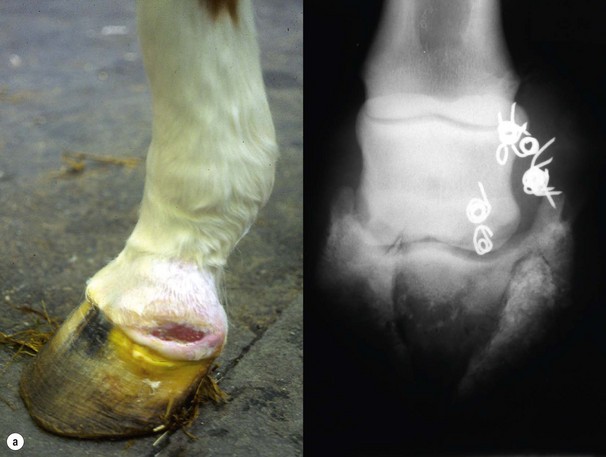
Factors that impair healing

23.5 Stages of wound healing
Repair phase (sometimes called the fibroblastic or proliferative phase)
23.7 Primary (first intention) healing
Criteria for primary closure
 β-haemolytic streptococci produce proteolytic enzymes, including streptokinase and staphylokinase, which are destructive to the wound.
β-haemolytic streptococci produce proteolytic enzymes, including streptokinase and staphylokinase, which are destructive to the wound.
 Pseudomonas spp. produce elastase, which specifically degrades elastin in the wound to which fibrin attaches.
Pseudomonas spp. produce elastase, which specifically degrades elastin in the wound to which fibrin attaches.
 Streptococcus spp. are nearly always susceptible to a topically applied penicillin or cephalosporin, and pseudomonads are susceptible to aminoglycides, polymixin B, and sulfamylon.
Streptococcus spp. are nearly always susceptible to a topically applied penicillin or cephalosporin, and pseudomonads are susceptible to aminoglycides, polymixin B, and sulfamylon.
Preparation of a wound for primary closure
Surgical debridement
Debridement by lavage