3 Principles of cancer chemotherapy
A basic understanding of the mechanisms of action and particular uses of chemotherapy is vital if we are to give the best-quality, compassionate and safe care to our cancer patients. It is important to remember that people can suffer markedly during chemotherapy, so from the outset we have to explain that in veterinary medicine it is generally considered ethically unjustifiable to allow our patients to experience such side effects, so we will attempt to make our chemotherapy side-effect-free where possible (which should be the majority of cases). However, in order to achieve this aim we have to use lower dosages than those used in human medicine with the inevitable consequence that veterinary chemotherapy usually has a lower success rate in terms of remission rates and durations when compared to such treatment in humans.
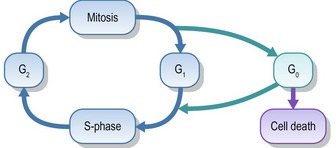
Tumours develop, therefore, because of an imbalance between normal cell growth/division and natural cell death. As a result, understanding the cell cycle is fundamental to understanding cancer biology. The cell cycle has four phases, as shown in Figure 3.1.
BASIC CONCEPTS OF TUMOUR GROWTH
Most tumours are detected late in the course of the disease, at which stage there are many millions of cells making up the tumour (e.g. a mass of approximately 1-cm diameter contains 109 cells whilst an average 20-cm mass contains 1012 cells). Tumour cell growth pattern generally follows ‘Gompertzian’ growth kinetics; that is, initially exponential cell division resulting in a rapid growth phase but as cell numbers increase the rate of cell division starts to tail off. This means that because large tumours contain a very high number of cells, only a small proportion of them will be dividing when compared to when the tumour was very small, and therefore there will be fewer cells that are susceptible to chemotherapy. Conversely, smaller tumours with a higher growth fraction theoretically have a greater potential response to chemotherapy because they contain a greater number of proliferating cells. This principle is illustrated graphically in Figure 3.2.
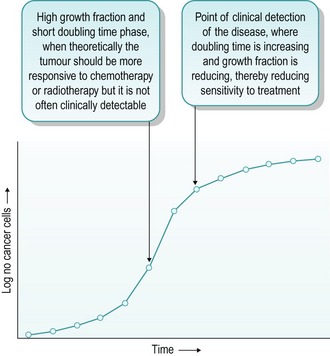
Figure 3.2 Rate of tumour cell growth relating to clinical detection and response to medical management
This graph also illustrates why surgical debaulking and follow-up chemotherapy or radiotherapy can theoretically be useful in tumours which display sensitivity to the follow-up treatment. By reducing the number of cancer cells in the mass, the growth curve can be shifted to the left, thereby generating a possible window of opportunity for the adjunctive treatments to be more effective than they would otherwise be without the surgery. Obviously, inherent tumour resistance, vascular supply and the type and grade of the tumour all impact on this principle so it is not possible to apply it to all conditions. However, the basic theory that chemotherapy and radiotherapy work most effectively on microscopic disease does generally apply, hence multimodal treatment should always be undertaken if possible.
INDICATIONS FOR CHEMOTHERAPY
DRUG DOSAGE AND TIMING
TOXICITY
Bone marrow toxicity
Alopecia
This is an uncommon complication but can be seen in dogs with constantly growing hair coats, such as Afghan hounds and old English sheepdogs. The author has also seen periorbital and facial alopecia in West Highland white terriers and Scottish terriers given doxorubicin (Figs 3.3, 3.4). Cats can lose their whiskers, especially with long-term vincristine therapy but more generalized alopecia is less common in cats than in dogs. If affected, the hair coat normally regrows on completion of the chemotherapy.
Gastrointestinal toxicity
The obvious clinical signs of gastrointestinal (GIT) toxicity are vomiting, anorexia and diarrhoea. The development of such signs is either secondary to direct damage to GIT epithelial cells or via efferent nervous stimulation of the chemoreceptor trigger zone or the higher vomiting centres. Anorexia is certainly a relatively common side effect after the administration of many chemotherapeutics, but this usually only lasts 24–36 hours. If there is a major concern regarding GIT toxicity then post-chemotherapy administration of antiemetics may be justified, and certainly, the author frequently recommends 5-day courses of an antiemetic (maropitant or metoclopramide) after a patient has received doxorubicin or carboplatin.
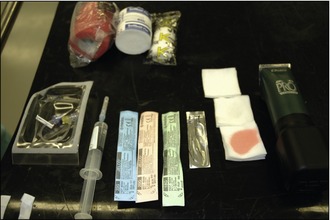
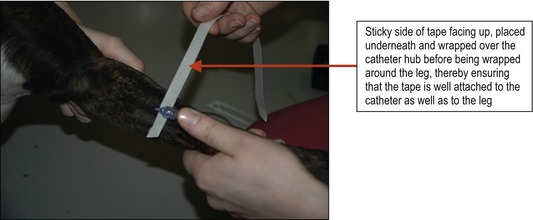
For this reason it is mandatory that all intravenous chemotherapeutic agents are administered through a well-placed intravenous catheter and never directly via a needle or butterfly catheter. Placement of the catheter must follow standard aseptic techniques and ensure that the catheter is securely fixed in place (Figs 3.5–3.12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree