CHAPTER 186 Placental Evaluation for Assessment of Foal Problems and Maternal Reproductive Health
Placental incompetence is an important cause of abortion in the mare. Placental adequacy is vital to fetal viability. Normal development and function of the placenta are dependent on maternal health, reproductive competence, and freedom from infection or other diseases. Compromised placental function may result from deficiencies on either the maternal or fetal side of the uteroplacental interface. Systematic and comprehensive placental evaluation gives invaluable insights into the reproductive competency of the mare, the in utero environment of the fetus, and the perinatal health of the foal.
THE NORMAL PLACENTA
No physical attachment exists between the allantoamnion and allantochorion in the horse. The fetus, surrounded by the allantoamnion, floats freely in the allantoic fluid, allowing great mobility in early pregnancy until fetal growth limits movement. This arrangement predisposes the equine fetus to death as a result of umbilical cord torsion.
FACTORS AFFECTING PLACENTAL DEVELOPMENT AND FUNCTION
Placental
Restrictions on placental development and attachment can adversely affect fetal development, with foal weight statistically related to both allantochorionic surface area and allantochorionic weight. The most common cause of diminished placental function is twinning (Figure 186-1). Apposition of the placentas in utero results in a loss of endometrial surface contact, decreasing nutrient and waste exchange ability, leading to chronic deprivation of both fetuses. In twin pregnancies, one fetus is usually confined to one uterine horn only, with the second fetus occupying the remaining horn and uterine body. Deprivation and subsequent death of the more confined fetus can cause placental separation and expulsion of both. Other causes of decreased maternal-fetal exchange include placental edema, chronic placentitis, and premature separation of placenta.
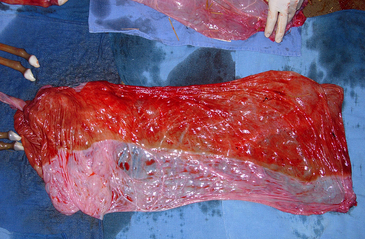
Figure 186-1 Loss of endometrial contact by the placenta, such as in this case of twinning, leads to large avillous areas of chorion. See Color Plate 26, following p. 832.
Fetoplacental infections cause up to one third of all abortions. Fetoplacental infections caused by bacteria, equine herpesvirus, fungi, or placentitis of unknown etiology were the most common causes determined in one retrospective study. In another review, pathogens identified most frequently were Streptococcus zooepidemicus, Leptospira spp., Escherichia coli, Pseudomonas aeruginosa, Streptococcus equisimilis, Enterobacter agglomerans, Klebsiella pneumoniae, α-hemolytic Streptococcus, nocardioform actinomycete, and fungi. Mixed bacterial infections were also found. In about one quarter of cases, no causative agent was found. Bacterial placentitis was observed to occur in either of two forms with regard to distribution (focal, diffuse) and time of onset (acute or chronic) (Figure 186-2).

Figure 186-2 Diffuse placentitis involving the caudal portion of the body of an equine placenta. See Color Plate 27, following p. 832.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


