Muscle contracture is shortening of the muscle owing to either intrinsic or extrinsic causes. Intrinsic changes are structural and can result from inflammatory or traumatic processes. Trauma, inflammation, ischemia, and hemorrhage in injured patients can restructure muscle tissue components and result in fibrosis and the development of adhesions. Following hemorrhage into a muscle, fibrin deposition occurs. Within 2 to 3 days fibrin is replaced with reticular fibers that form a loose connective tissue network. If the affected muscle is kept immobile, the network becomes more dense and resistant to stretch.1 The position in which limbs are immobilized also contributes to the development of contractures. Muscle fibers lose up to 40% of the length of sarcomeres when immobilized in a shortened position. Therefore whenever possible joints should be kept in a neutral position to keep muscle fibers at equal length and tension to minimize contracture.2 Additional factors that affect the rate of contracture development include the precipitating cause, duration and degree of immobilization, and preexisting joint restrictions. Edema, ischemia, and bleeding accelerate the development of muscle and joint contracture. Immobile, injured patients therefore require efforts directed at prevention and treatment of contracture development following soft tissue musculoskeletal injuries (Table 37-1). Table 37-1 Treatment of Musculoskeletal Injuries The respiratory complications of prolonged immobility and those resulting from primary injuries are numerous and potentially catastrophic in critically injured patients. Injuries to the head, chest, and abdomen often result in reduced respiratory function because of pain, inability to move, altered consciousness, or damage to thoracic structures. Impaired consciousness from head injury may lead to altered breathing patterns, diminished ability to cough, and inability to change body position. Rib fractures, pneumothorax, pulmonary contusions, and painful soft tissue injuries to the chest and abdomen may result in a restrictive breathing pattern characterized by shallow, rapid ventilation. This type of breathing pattern causes a reduction in tidal volume, functional residual capacity, and lung compliance. Altered respiratory patterns in conjunction with immobility may lead to atelectasis, accumulation of respiratory secretions, and pneumonia. It is important for the clinician to note any injuries that may compromise respiratory function and devise a physical rehabilitation plan to address those concerns. Chest physical rehabilitation is a term that describes the use of techniques aimed at improving lung volumes or facilitating the removal of airway secretions.3 The goals of chest physical rehabilitation are to maintain bronchial hygiene, eliminate secretions from the airways, re-expand atelectatic lung segments, improve oxygenation, and reduce the incidence of pneumonia (Table 37-2). These goals can be achieved through techniques such as stimulating the animal to cough, frequent repositioning, postural drainage, percussion, vibration, and exercise. Each of these techniques is reviewed in detail. Table 37-2 Goals of Chest Physical Rehabilitation Coughing is the most important defense mechanism to eliminate retained secretions. A cough can eliminate secretions from the trachea to the level of the fourth-generation segmental bronchi.4 An effective cough is initiated by a deep inspiration, followed by closure of the glottis and contraction of the chest wall and abdominal musculature to generate high intrathoracic pressure. After high intrathoracic pressure is attained, the glottis opens and is followed by rapid expulsion of air during exhalation. Critically injured patients may not be able to initiate a cough because of impaired consciousness, pain, weakness, or injuries to the chest or abdominal wall. These animals can be assisted to cough by applying gentle pressure to the trachea at the level of the third tracheal ring. Placing an animal in sternal recumbency may also improve an animal’s ability to cough. Animals should be assisted to cough after postural drainage, percussion, and vibration and before changes are made in the patient’s position. Injured animals are often unable to move or change position within their cage. Alternating right, sternal, and left lateral recumbency every 4 hours is recommended for immobile patients. Frequent repositioning helps prevent atelectasis and pooling of secretions in dependent lung segments. Because position influences the distribution of blood flow to the lungs, changing body positions alters ventilation/perfusion (
Physical Rehabilitation for the Critically Injured Veterinary Patient

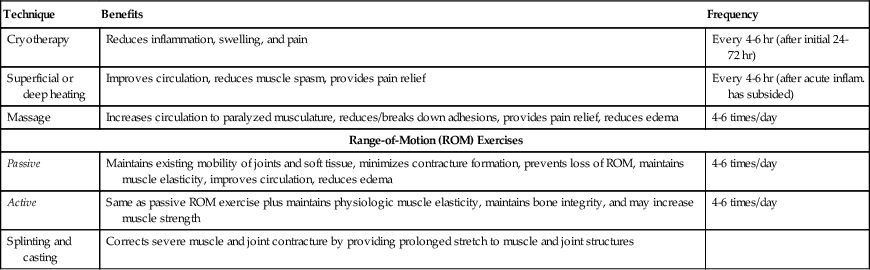
The Musculoskeletal System
Technique
Benefits
Frequency
Cryotherapy
Reduces inflammation, swelling, and pain
Every 4-6 hr (after initial 24-72 hr)
Superficial or deep heating
Improves circulation, reduces muscle spasm, provides pain relief
Every 4-6 hr (after acute inflam. has subsided)
Massage
Increases circulation to paralyzed musculature, reduces/breaks down adhesions, provides pain relief, reduces edema
4-6 times/day
Range-of-Motion (ROM) Exercises
Passive
Maintains existing mobility of joints and soft tissue, minimizes contracture formation, prevents loss of ROM, maintains muscle elasticity, improves circulation, reduces edema
4-6 times/day
Active
Same as passive ROM exercise plus maintains physiologic muscle elasticity, maintains bone integrity, and may increase muscle strength
4-6 times/day
Splinting and casting
Corrects severe muscle and joint contracture by providing prolonged stretch to muscle and joint structures
Respiratory System
Technique
Goals
Positioning
Reduce risk of atelectasis, improve ventilation/perfusion, improve gas exchange, reduce risk of pressure sores, minimize muscle and joint stiffness
Cough
Remove secretions from trachea to fourth-generation bronchi
Postural drainage
Increase mobilization and elimination of secretions from upper airways
Percussion
Dislodge bronchial secretions
Vibration
Move secretions into larger airways
Cough
Positioning
 ) relationships within the lungs. When a patient is positioned with the compromised lung segment in a dependent position, that lung receives increased blood flow, resulting in increased
) relationships within the lungs. When a patient is positioned with the compromised lung segment in a dependent position, that lung receives increased blood flow, resulting in increased  mismatch and impaired gas exchange.5 Therefore if pulmonary contusions or pneumonia are present, positioning the patient with the good lung down improves oxygenation by limiting
mismatch and impaired gas exchange.5 Therefore if pulmonary contusions or pneumonia are present, positioning the patient with the good lung down improves oxygenation by limiting  mismatch and improving gas exchange. Improved oxygenation and a reduction in the number of patients with postoperative fever have been documented in humans when side-to-side turning is used.6
mismatch and improving gas exchange. Improved oxygenation and a reduction in the number of patients with postoperative fever have been documented in humans when side-to-side turning is used.6
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


