Eileen S. Hackett
Penetrating Wounds of Synovial Structures
Penetrating wounds of synovial structures occur secondary to trauma and result in wounds that communicate with joints and tendon sheaths. In some reports, traumatic wounds involving synovial structures affect tendon sheaths at an equal or greater frequency than joints. Synovial penetration is an ever-present risk following trauma to the limbs of horses. A detailed knowledge of synovial structure is necessary to determine whether wounds communicate with a synovial structure.
Triage
Triage of horses with suspected synovial penetrating wounds is critical and begins with the initial client contact. Any wound on a limb or hoof should be evaluated immediately. Especially in the distal portions of the limbs, horses have minimal soft tissue protection overlying synovial and collateral structures. Clients should be instructed to clean the area around the wound and apply a bandage if possible to protect the site. If a horse has a nail penetrating the solar surface of the hoof that does not protrude to the point of interfering with standing, the nail may be left in place until prompt radiographic examination can be performed. Referral to a treatment hospital is generally indicated for complete preliminary evaluation and care of wounds with suspected synovial injury. Administration of systemic antimicrobials may be appropriate before referral, despite the potential to interfere with subsequent bacterial culture of synovial fluid. Depending on the extent of injury, such as that incurred with collateral ligament or flexure tendon injury, external coaptation may be required before referral.
Diagnostics
Horses with penetrating synovial wounds often have moderate to severe lameness, decreased range of motion, and heat, pain, or swelling around the wound site. Leakage of synovial fluid from the wound may be evident. Of primary importance in evaluation of a wound overlying a synovial structure is definitively confirming or ruling out synovial penetration and contamination. After aseptic preparation, large wounds may be palpated with a gloved (sterile) hand, and penetration can be confirmed by palpation of joint surfaces or flexor tendon structures. Alternatively, a needle can be placed in the suspected synovial cavity in a site distant to the wound. After needle placement, synovial fluid aspiration is attempted, and 0.9% saline solution is then injected. If the synovial cavity is intact, saline injection will pressurize the structure and result in visible distension. If the cavity has been recently penetrated, saline may leak from the site of penetration and be evident at the wound surface. Attaching a 30-inch extension intravenous set between the needle and syringe is helpful if the horse moves during this evaluation. In horses with puncture wounds that have sealed before initial examination, other diagnostic modalities must be used for synovial evaluation.
Synovial fluid from cavities with penetrating injury may be discolored, cloudy, and nonviscous in consistency. Clinicopathologic parameters of primary interest in synovial fluid evaluations include total protein concentration, total nucleated cell count, and white blood cell population differential. Synovial total protein greater than 4 g/dL and nucleated cell counts of 30,000 cells/µL or greater, with 80% or greater neutrophils, support synovial cavity wound communication. Diagnosis of sepsis is also supported by synovial fluid pH less than 6.9, lactate higher than 4.9 mmol/L, and serum-synovial glucose differences greater than 39.6 mg/dL. Despite contamination, not all synovial fluid samples from penetrated joints will have a positive culture result. Isolates from synovial fluid after penetrating contamination most commonly include Staphylococcus spp and Streptococcus spp, as well as Escherichia coli, Actinobacillus spp, Enterobacter spp, Pseudomonas spp, Corynebacterium pyogenes, Actinobacter spp, Pasteurella spp, Bacillus spp, and Aspergillus spp. The likelihood of culture success is improved if synovial fluid is transferred immediately upon collection to blood culture enrichment media. After the onset of infection, susceptibility testing is essential to determine appropriate antimicrobial treatment, and culture success may be further improved with larger volumes of sample fluid being placed in media containing antimicrobial inhibitors.
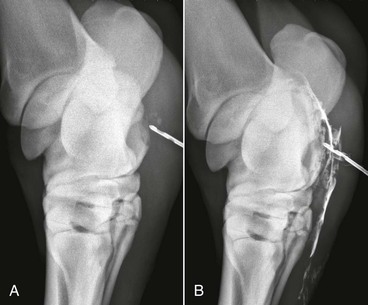
Another method of determining synovial cavity penetration is to perform a radiographic fistulogram by injecting radiopaque contrast solution into the wound. Injection can be facilitated by use of a teat cannula if the wound is small (Figure 8-1). If the contrast material injected into the wound highlights a synovial structure on subsequent radiographic examination, communication between wound and synovial cavity is confirmed. Additionally, contrast can be injected into synovial cavities adjacent to wounds, and leakage of contrast into the wound bed evident radiographically may confirm communication. Standard iodinated contrast solutions have antimicrobial properties and are safe to inject into wounds and joints for diagnostic purposes. Survey radiographs taken before contrast injection are also helpful to evaluate injury to collateral bony structures (see Figure 8-1). Other imaging modalities, such as ultrasound and magnetic resonance imaging, may be helpful for identification in challenging cases of septic synovitis.
Treatment
Treatment of horses with penetrating synovial wounds consists of a combination of systemic and local antimicrobials, judicious use of nonsteroidal antiinflammatory drugs, wound care, and surgical synovial irrigation. Broad-spectrum systemic antimicrobial treatment is indicated after traumatic synovial penetration, despite concern of limited local penetration. Parenteral antimicrobials, most often a combination of aminoglycoside and ß-lactam agents, are selected initially, and the horse may be transitioned to enteral medications for longer treatment intervals (Table 8-1). A typical course of systemic antimicrobial treatment for uncomplicated synovial penetration would consist of 3 to 5 days of intravenous antimicrobials, followed by 10 to 14 days of orally administered antimicrobials.
TABLE 8-1
Systemically Administered Antimicrobials Used in Treatment of Horses With Penetrating Wounds in Synovial Structures
| Antimicrobial | Dosage | Route | Comments |
| Amikacin | 15-25 mg/kg q 24 hr | IV, IM | Nephrotoxic; preferred in foals |
| Ampicillin | 15-20 mg/kg q 8-12 hr | IV | |
| Cefazolin | 11-22 mg/kg q 6-8 hr | IV | |
| Cefotaxime | 25 mg/kg q 6 hr | IV | |
| Ceftiofur | 3-4 mg/kg q 8 hr | IV | |
| Chloramphenicol | 44 mg/kg q 6-8 hr | PO | Limit human contact with drug |
| Doxycycline | 5-10 mg/kg q 12 hr | PO | |
| Enrofloxacin | 5-7.5 mg/kg q 24 hr | IV, PO | Safety not demonstrated in foals |
| Gentamicin | 6.6 mg/kg q 24 hr | IV, IM | Nephrotoxic; ensure hydration |
| Imipenem-cilastin | 10-20 mg/kg q 6 hr | IV | Use only with confirmed culture and limited sensitivity |
| Penicillin | 22,000-44,000 IU/kg q 6-12 hr | IV, IM | |
| Trimethoprim-sulfamethoxazole | 20-30 mg/kg q 12 hr | PO | |
| Metronidazole | 15-25 mg/kg q 6-8 hr | PO |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree