Chapter 242
Pearls of the Ophthalmic Examination
Although signalment and historical data often provide essential clues to ocular diagnoses, ready visualization of almost all parts of the eye means that nothing can replace a complete examination. Fortunately a thorough ophthalmic examination is performed with just five requirements, five skills, and minimal equipment.
There are five essential requirements for a thorough ophthalmic examination:
To minimize the extent to which the eyelids and orbital structures obscure the ocular structures, the patient should always be placed at eye level with the examining veterinarian. This is usually achieved simply by placing the patient on the examination table, which also limits patient movement. Having an assistant rather than the owner restrain the pet further reduces movement and is especially important when a detailed examination with magnification is performed. Since many structures within the normal eye are transparent, they are best examined in a darkened room using a very focal light source. This combination maximizes reflections, which are useful for examining ocular surfaces. Dim ambient light also facilitates examination of the darker interior structures of the globe. Many ocular abnormalities are small and will be missed without a source of magnification and a bright light source. This combination can best be achieved in practice by using a magnifying head loupe (e.g., Optivisor) and Finnoff (Welch Allyn) transilluminator. A readily available alternative is the otoscope used without the plastic cone. This provides a focal light source and approximately 2× to 3× magnification, but does not permit the direction of illumination and examination to be varied independently of one another. Slit-lamp biomicroscopes are used by ophthalmologists and some general practitioners and maximize the combination of magnification and a focal light source. By focusing the light to a narrow slit, an optical section provides microscopic detail of transparent ocular media such as the tear film, cornea, aqueous, lens, vitreous, and (to a lesser extent) conjunctiva.
The ophthalmic examination should be carried out in a repeatable and sequential manner to ensure that nothing is overlooked. A prepared examination sheet reminds the practitioner to perform all necessary tests in the correct sequence and permits lesions to be drawn. The examination begins by observing the patient from a distance for behavioral evidence of vision loss. The patient’s head and periocular tissues should then be more closely examined for facial symmetry, globe position and movement, periocular discharge, and overt ocular abnormalities. Brief but complete testing of the cranial nerves involved in normal ocular function follows. This should include tests of the menace response, palpebral reflex, direct and consensual pupillary light reflexes, and dazzle reflex. More detailed examination of each eye is then performed. Examining the unaffected eye before the affected eye in animals with unilateral disease ensures that the normal eye is not forgotten and provides information on each patient’s normal ocular appearance.
Mastering the following five skills ensures that the essential findings from the anterior and posterior segments of the eye are not missed:
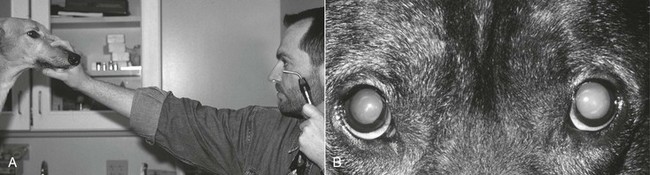
Retroillumination is a simple but extremely useful technique for assessment of pupils and all parts of the transparent ocular media (tear film, cornea, aqueous, lens, and vitreous). A focal light source such as a Finnoff transilluminator is held close to the examiner’s eye and directed over the bridge of the patient’s nose from at least arm’s length (Figure 242-1, A). Alternatively, the direct ophthalmoscope can be held against the examiner’s eye (as for the fundic examination) but about arm’s length from the patient. Either technique elicits the fundic reflection, which is usually gold or green in tapetal animals or red in nontapetal individuals (Figure 242-1, B). Because the examination is done at arm’s length, each eye can be illuminated equally, and the fundic reflex can be used to assess and compare equality of pupil size and shape. In addition, opacities in any of the clear ocular media (e.g., corneal blood vessels, cataracts, vitreous debris) obstruct the fundic reflection and are noted as black “shadows” against the fundic reflection. These opacities should be noted for subsequent and more detailed examination, with retroillumination repeated from close to the patient following pupil dilation. They should also be examined using transillumination and a source of magnification. Retroillumination is particularly useful for differentiating nuclear sclerosis from cataract.
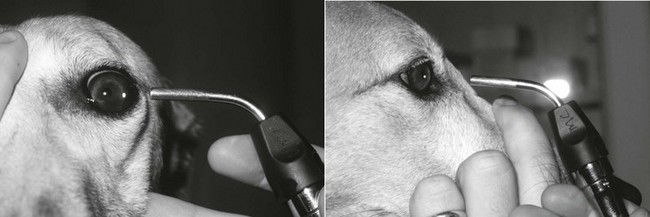
Transillumination (sometimes called focal illumination) is then used to sequentially examine all ocular structures in front of and including the lens (the “anterior segment”). A focal light source should be directed at the eye from many angles while the examiner simultaneously varies the viewing angle (Figure 242-2). Varying the viewing and lighting angles relative to each other permits the examiner to use parallax, reflections, perspective, and shadows to gain valuable information regarding lesion depth. This technique is particularly useful for examining the anterior chamber since changes within this chamber can be more easily differentiated from corneal, iridal, or lenticular changes when viewed transversely. In cats the corneal curvature and anterior chamber depth are so great that limited visualization of the iridocorneal angle is also possible.
The importance of a sequential anterior segment examination cannot be overstated. An obvious method is to begin at the front and progress to the back of the eye while simultaneously moving from peripheral to axial. This ensures that the eyelids (including periocular skin, eyelid margin, and cilia), conjunctiva (third eyelid, bulbar, and palpebral conjunctival surfaces, as well as nasolacrimal puncta), sclera, cornea (including the limbus and tear film), anterior chamber, iris, pupil, and lens are examined completely. Anterior segment examination should be initiated before dilation so that the iris face is easily examined; however, complete examination of the lens requires full dilation. The complete anterior segment should be examined using transillumination and a source of magnification such as the Optivisor, the otoscope head, or a slit-lamp biomicroscope. Following pupil dilation, retroillumination can be repeated from close to the patient and with a source of magnification so that lesions in the clear ocular media can be both backlit and magnified without the pupil constricting. The otoscope head is particularly useful for this because the examiner can alter the viewing angle until the lesion is either backlit by the tapetal reflection dorsally or viewed against the dull nontapetal area of the fundus ventrally while illuminated from in front. In both cases the otoscope head is moved in or out from the eye until the lesion is in crisp focus and under full magnification against the chosen background.
Tonometry is the estimation of IOP and is essential for differentiating between the two major vision-threatening conditions in which red eye is the hallmark feature: uveitis and glaucoma (see Chapters 251 and 252). Digital tonometry, in which the IOP is crudely assessed by compressing the globe against the orbital rim, is completely unreliable. The Schiøtz tonometer is reliable but awkward to use and requires conversion tables to convert the scale reading to the standard unit of IOP (millimeters of mercury). The availability of easily used and reasonably priced tonometers such as the Tono-Pen and TonoVet has made estimation of IOP easier in all species, particularly cats. Unlike the Schiøtz tonometer, the Tono-Pen and TonoVet estimate IOP directly and do not require any conversion. They can also be held horizontally and therefore allow recordings to be performed with the patient’s head held in a normal, relaxed position. Finally, they each have a small probe that permits measurement of IOP in even the smallest feline and pediatric canine eyes.
The Tono-Pen comes with an excellent instructional video and manual; however, the following tips may help the veterinarian achieve optimal results. The tonometer should be periodically calibrated according to the manufacturer’s directions. A drop of topical anesthetic is applied to the cornea. A disposable cover is placed over the Tono-Pen tip, and the pen is turned on with firm, somewhat protracted pressure on the large black button about one third down the shaft. Correct patient restraint is essential. The patient should be lightly restrained so as to not artificially raise IOP. In particular, direct pressure on the jugular veins by the holder or by a collar should be avoided. Similarly, no pressure should be exerted on the globe itself via the eyelids. This is best achieved by having an assistant (not the owner) restrain the patient’s head, holding the angle of the mandible and the occiput. The Tono-Pen is then held in the dominant hand, and the patient’s eyelids are gently parted using the nondominant hand so that pressure is applied to the underlying orbital rim, not the globe. The hand holding the Tono-Pen should then be rested onto the hand holding the eyelids or onto the patient’s head itself. Very small, rapid movements of the Tono-Pen away from and back toward the cornea such that the cornea is very lightly “blotted” with the Tono-Pen tip enhance the reliability and reproducibility of the readings while reducing the number of readings necessary. Particular attention should be paid to the “approach angle” of the Tono-Pen tip to the cornea. The flat surface of the tip should be exactly parallel to the corneal surface. This is best achieved by viewing the interface between the cornea and the tip from the side. Said another way, the Tono-Pen itself should approach the globe as close to perpendicular to the corneal surface as possible. Therefore, because of corneal curvature, the approach angle must be changed dramatically if any area other than the central cornea is used or if the patient redirects its gaze from straight ahead.
Each time the cornea is appropriately “blotted” with the probe, an electronic tone advises the operator that a reading has been obtained. When a suitable number of readings have been obtained, a longer tone of a different pitch sounds, and no further readings can be obtained without restarting the Tono-Pen using the black button. The number of readings required to achieve an average varies, depending on how disparate the readings are from each other and from the normal physiologic range. A small digital screen displays the IOP in mm Hg and provides an estimate of the “reliability” (coefficient of variance) of the result. This appears as a small bar located above one of four percentage readings. This bar should be above the 5% mark, or tonometry should be repeated for that eye. Estimates of IOP with the Tono-Pen are highly correlated with manometric pressure; however, this tonometer tends to overestimate pressure at lower IOPs and underestimate IOPs at higher pressures.
The TonoVet tonometer uses the mechanical principle called rebound tonometry to estimate IOP. A small probe is ejected at a fixed distance from the cornea and the motion of the probe is measured as it rebounds from the cornea and returns to the instrument. Since this technique is affected to some degree by ocular surface tension, it must be performed before application of any topical medications, including topical anesthetic, and it is unclear what effect reduced tear film might have on IOP readings obtained from patients with dry eye or other corneal pathologies. Tono-Pen applanation tonometers are probably less susceptible to erroneous readings attributable to these variables than rebound tonometers. The TonoVet has been calibrated for normal dogs, cats, and horses; thus the correct software must be selected before IOP recordings begin. Because of this species-specific calibration in normal animals, the rebound tonometer tends to estimate IOP very close to true pressure measurements as determined with a manometer.
Across large populations, normal canine and feline IOP is reported as approximately 10 to 20 mm Hg (using any tonometer). However, variation is noted between individuals, technique, tonometer, and time of day. Therefore comparison of IOP between right and left eyes is critical to interpretation of results. A good rule of thumb is that IOP should not vary between eyes of the same patient by more than 20%. Because IOP measured by the Schiøtz tonometer, Tono-Pen, and TonoVet can differ, it is important to record which tonometer was used.
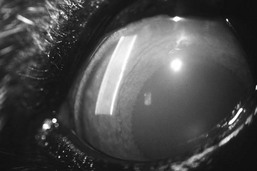
Aqueous flare is a pathognomonic sign of uveitis and is the result of breakdown of the blood-aqueous barrier, with subsequent leakage of plasma proteins into the anterior chamber where, with special technique, they can be seen. Aqueous flare is best detected using a very focal, intense light source in a totally darkened room. The passage taken by the beam of light is viewed from an angle. In the normal eye a focal reflection is seen where the light strikes the cornea. The beam is then invisible as it traverses the almost protein- and cell-free aqueous humor in the anterior chamber. Because of the presence of lens proteins, the light beam becomes visible again as a focal reflection on the anterior lens capsule and then as a diffuse beam through the body of the normal lens. If uveitis has allowed leakage of serum proteins into the anterior chamber, these proteins will cause a scattering of the light as it passes through the aqueous humor (Figure 242-3). This is called aqueous flare and is seen as a beam of light traversing the anterior chamber and joining the focal reflections on the corneal surface and the anterior lens capsule or iris. A slit lamp provides ideal conditions for detecting aqueous flare; however, the beam produced by the smallest circular aperture on the direct ophthalmoscope, at brightest illumination, in a completely darkened room, held as closely as possible to the cornea, and viewed transversely with some form of magnification also provides excellent results. The slit beam on the direct ophthalmoscope is not as intense as the small circular aperture and does not provide as many “edges” of light along which flare can be most readily appreciated. Aqueous flare is best seen against a black “backdrop,” which in the eye is the pupil. Therefore assessment of flare is sometimes easier after complete pupil dilation. Combined assessment of IOP and aqueous flare should be performed whenever glaucoma or uveitis is suspected because of the frequency with which these conditions coexist.
< div class='tao-gold-member'>