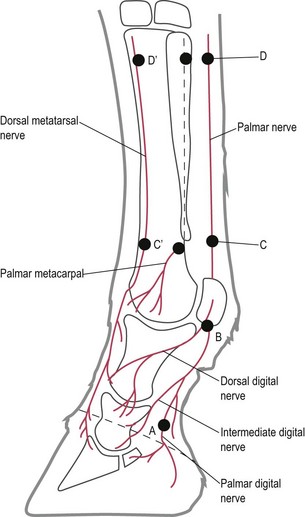
Chapter 15 15.1 Diagnostic approach to lameness Osteoarthritis (degenerative joint disease) Osteochondritis dissecans (OCD) Subchondral bone cysts (osseous cyst-like lesions) Nutritional secondary hyperparathyroidism (bran disease, big head, osteodystrophia fibrosa) Hereditary multiple exostoses (multiple cartilaginous exostoses, osteochondroma) Hypertrophic osteopathy (hypertrophic pulmonary osteoarthropathy, Marie’s disease) Diagnosis of orthopaedic problems involves a number of basic steps namely: 1. Essential information includes: • Use (or intended use) of the horse. • Nature of the problem (lameness or loss of performance). • Duration of the problem (recent or chronic). 2. Details of recent management may be relevant including exercise, shoeing, housing and feeding. 3. Previous locomotor problems known to the owner should be noted. 1. Overall inspection of the horse from all angles noting particularly: • Conformation of body, limbs and feet. • Posture and weight-bearing on the limbs. • Skeletal and soft tissue symmetry. 2. Detailed evaluation of all individual regions of the limbs by: • Inspection, which should reveal deformity, swelling or thickening, skin wounds and muscle wasting. • Palpation, which is helpful in detecting heat and pain as well as characterizing the precise location and consistency of any swellings or thickenings. • Manipulation of the joints, which allow evaluation of range of movement – detecting restriction, instability, pain or crepitus. The aim should be to identify: 1. The presence or absence of a gait abnormality. 2. The limb or limbs involved. 3. The character of any abnormality present. • The gait is usually best evaluated on a hard level surface. Ideally this should be done in a safe, enclosed area free of distractions and dangers such as traffic and other horses. • Some forms of lameness are best examined immediately after taking the patient out of its stable (i.e. ‘cold lameness’). Chronic low-grade lameness may require a period of sustained exercise to become more obvious. • Horses should be stripped of all tack, rugs and blankets and should be held by a loose rope that is fixed to a headcollar or bridle. • Abnormalities of gait are usually most apparent when the horse is moving at the walk or slow trot. Initial evaluation should be performed at the walk to identify those horses which are markedly lame where trotting may be hazardous. Variations in foot placement and limb movement, e.g. shortening of one phase of the stride on one limb, are generally most easily appreciated at the walk when limb movement is slower. In addition, mechanical and neurological causes of lameness are often more apparent at the walk. • Abnormalities in head and hindquarter movement resulting from pain during weight-bearing are usually most apparent at the slow trot. • The horse should be observed moving in a straight line and at an even pace from in front, the side and behind. • Forelimb lameness is best observed while the horse is trotted towards or past the examiner. Hind limb lameness is best observed while the horse is trotted away or past the examiner. Observation from the side is easier if the observer is on the side of the lame limb. • Lunging the horse in tight circles is helpful in demonstrating more clearly lameness that is subtle or inapparent when the horse is moving in a straight line. If circumstances do not permit such an examination, trotting the horse around sharp corners may accentuate lameness in a similar, though more transient, way. • It is rare for horses to have to be ridden or driven to make lameness noticeable. Lameness in Standardbreds is an exception to this rule and can often only be observed on the track at full racing speed. • Canter or gallop is only occasionally of value in the observation of lameness. • Horses with forelimb lameness due to pain on weight-bearing shift the distribution of weight from the affected limb across to the contralateral forelimb and back to the hind limbs. This is achieved, at least in part, by lowering the head and neck less as the lame forelimb takes weight, and, in compensation, lowering the head and neck more as the sound forelimb strikes the ground. This downward nodding of the head as the sound forelimb strikes the ground is generally the easiest abnormality of movement to appreciate and allows identification of the lame (or lamer) forelimb. The sound limb may also be heard to strike the ground with greater force, particularly if the horse is shod. • In hind limb lameness the normal symmetrical vertical movements of both quarters, as observed from behind the horse, is disturbed. The quarter on the lame side rises and falls through a greater range of motion than that of the sound limb. This is usually characterized by a long downwards drop during the swing-phase of the stride, followed by a fast, sudden, upwards flick, or hike, during the weight-bearing phase of the stride. • Head movements are less helpful in the recognition of hind limb lameness. With moderate to severe lameness, the horse may attempt to shift its centre of gravity forward when the lame hind limb starts to bear weight, which can give the misleading impression of a downward head nod during the support phase of the contralateral forelimb, and hence ipsilateral forelimb ‘referred’ lameness. • Bilateral forelimb or hind limb lameness is often very difficult to recognize when the horse moves in a straight line. The horse usually shows a stiff, stilted gait with bilaterally shortened stride length. More pronounced unilateral signs of lameness are usually observed when the limbs are subjected to uneven stresses (e.g. by lunging in tight circles). • Abnormalities of limb movement may also be appreciable in the lame horse: Certain gait characteristics may be indicative of the site of pain: • Swinging limb lameness often originates from the proximal limb. • Supporting limb lameness usually reflects pain in the distal limb. • In bilateral lameness, the cranial phase of the stride is bilaterally shortened, even in distal limb lameness. This results in a stiff, stilted gait. It is useful to examine the horse on both soft and hard ground. • Lameness in the distal limb is often exacerbated on hard ground. • Proximal lameness may be exacerbated on soft ground. • Lunging or circling the horse provides further information for the observer: 0. Lameness not perceptible under any circumstances. 1. Lameness is difficult to observe and is not consistently apparent, regardless of circumstances (e.g., under saddle, circling, inclines, hard surface, etc.). 2. Lameness is difficult to observe at a walk or when trotting in a straight line, but consistently apparent under certain circumstances (e.g., weight carrying, circling, inclines, hard surface, etc.). 3. Lameness is consistently observable at a trot under all circumstances. 4. Lameness is obvious at a walk. 5. Lameness produces minimal weight-bearing in motion and/or at rest or a complete inability to move. 0–10 scale (assessed at the trot): 1. The minimal degree of lameness detectable which may be inconsistent. 2. A consistent, but mild, degree of lameness – detectable and consistent subtle head-nod. 3. Consistent and obvious head nod/pelvic asymmetry. 4. Pronounced head nod/pelvic asymmetry. 5. Marked head nod/pelvic asymmetry. 6. Very marked head nod/pelvic asymmetry. 7. Difficulty trotting; only just able to place heels to the ground. 8. Minimal weight-bearing, heels not placed on the ground. 9. Only able to touch the limb to the ground. Provocative tests may be used for three basic reasons: 1. To demonstrate occult lameness in a horse that appears ‘sound’ on initial gait evaluation. 2. To exacerbate a mild lameness. 3. To aid localization of the abnormality causing the lameness. A variety of manoeuvres are employed. The most commonly used are ‘flexion tests’: • A flexion test is performed by holding the joint under consideration in a firmly flexed position for a period (usually 1 minute) and then immediately watching the horse move, usually at the trot, to detect any change in gait compared to that observed before performing the test. The response to a flexion test should be interpreted in the light of other findings, and it is wise to avoid using it as the sole criterion upon which to base a firm diagnosis. • As far as possible, the examiner attempts to flex the suspected joint only. Since some joints are inherently linked together in flexion and extension (i.e. hock and stifle; phalangeal joints and fetlock), exact differentiation of pain responses between these joints is not possible. • Extension of the distal interphalangeal (DIP) joint may be performed using a wedge-shaped piece of wood with a 20° inclination, which is placed under the weight-bearing foot to raise the toe and increase the load on the deep digital flexor tendon (DDFT), the navicular bone and its ligaments. After 2 minutes, the horse is trotted away. Unfortunately, the response to this test is inconsistent, even in confirmed cases of navicular syndrome. • Response to localized pressure over exostoses, tendon swellings, splints, etc., can be assessed. Localized pressure is maintained for 1 minute over the suspected site of pain, after which the horse is immediately trotted away. • In all tests, the examiner looks for any significant exacerbation of lameness. Only by experience can one learn where the boundaries of normality lie for the amount and duration of tension applied. A sound horse should not show consistent lameness following any of these tests. • The use of local analgesia relies on accurate placement of local analgesic into or around the structure to be desensitized, followed by evaluation of its effect on the gait. • The results of regional analgesia are most easily and reliably interpreted in horses with an obvious and consistent degree of lameness. • Interpretation is more difficult and less reliable in horses with slight or inconsistent lameness. • If the lameness is chronic and low-grade, it may be helpful to exacerbate the problem by exercising the horse for a few days to make the lameness more apparent prior to the use of local analgesia. • Conversely, caution should be exercised with the use of regional analgesia in acutely lame horses if there is a possibility that the cause may be an injury which could be exacerbated by injudicious use of a limb rendered pain free by the use of local analgesia. An example would be a horse with an undisplaced fracture that may displace with increased weight-bearing. Initial radiographic and/or scintigraphic examination may be prudent if such injuries are suspected. Local analgesia may be used for: 1. Perineural infiltration around specific nerves to desensitize regions of the limbs supplied by those nerves distal to the site of injection. 2. Intrasynovial analgesia of joints, tendon sheaths or bursae. 3. Direct local infiltration over suspect superficial lesions. 4. Field analgesia, performed by circular injection around the suspected site of disease, thereby blocking all nerve fibres entering the area. • All local analgesics prevent depolarization of the nerve by changing the permeability of the cell membrane to sodium ions (Na+). The analgesic cation binds to the nerve cell membrane anion. This results in blocking of the Na+-channels in the cell membrane. • The preparations used for nerve blocks in lameness examinations should be intermediate in duration of action (60 to 90 minutes). Lidocaine hydrochloride is commonly used but may produce more soft tissue swelling than mepivacaine which causes minimal tissue reaction and has a slightly longer duration of action. • The site of injection should be clean. The hair need not be clipped for nerve blocks or for intrasynovial centesis. Strict adherence to aseptic technique is required for all intrasynovial injections and it is good policy for all regional injections as many of these are close to synovial cavities, and so inadvertent penetration is possible. 1. Some of the smaller joints and bursae contain only a very small amount of synovial fluid (e.g. the navicular bursa or the distal intertarsal joint). 2. Synovial villi may be sucked into the end of the needle and prevent any synovial fluid escaping through it. Anatomy: Two distinct systems of innervation have been identified in the lower limbs: the superficial and deep innervation systems. • The superficial innervation of the forelimb is supplied by the lateral and medial palmar nerves, which course distally between the suspensory ligament (SL) and the DDFT. These nerves form a continuation of the median and ulnar nerves. • The deep innervation of the forelimbs originates from the lateral palmar nerve (palmar branch of the ulnar nerve) which forms the lateral and medial palmar metacarpal nerves. These nerves course distally between the splint bones, the SL and the metacarpus. Distal to the button of the splint bone these nerves regain a subcutaneous location, turn to the dorsal aspect of the fetlock, and end halfway down the dorsal aspect of the pastern. • The pattern of distribution of the deep and superficial innervation of the lower hind limb is similar to that of the forelimb, apart from one major difference – the presence of a dorsal deep innervation system that originates from the deep peroneal nerve. The lateral and medial dorsal metatarsal nerves course distally all the way down into the laminar corium of the foot. • Variations on this pattern of nerve distributions are commonly found in the forelimbs. Palmar/plantar digital nerve block (PDNB) (Figure 15.1): The Palmar/plantar digital nerves are palpated along the lateral and medial borders of the DDFT, palmar/plantar to the accompanying artery. One to two millilitres of local analgesic solution are injected in the angle between the ungular cartilages of the distal phalanx and the palmar/plantar aspect of the pastern, on the palmar/plantar border of the neurovascular bundle. This results in desensitization of the entire foot including the navicular bone, the navicular bursa, the suspensory ligaments of the navicular bone, the distal part of the DDFT, the digital cushion, the corium of the frog, the solar and laminar dermis, the DIP joint and the distal phalanx. The only part of the foot that is not desensitized by a PDNB is the dorsal aspect of the coronary band and the sensitive laminae of the dorsal wall of the toe. The understanding that the PDNB only desensitizes the palmar/plantar half of the foot is obsolete. Absence of skin sensation over the heels indicates that the block has taken effect. Abaxial sesamoid nerve block (ASNB) (Figure 15.1): The dorsal and palmar/plantar digital nerves are part of the neurovascular bundle which is easily palpated over the abaxial surface of the proximal sesamoid bones. The needle is inserted in a distal direction, just palmar/plantar to the neurovascular bundle, by the base of the proximal sesamoid bone, and 2–3 mL of local analgesic solution is injected on both sides. Correct injection leads to desensitization of the entire foot, the DIP joint, the distal sesamoidean ligaments and flexor tendons distal to the site of injection, the proximal interphalangeal (PIP) joint, and often part of the fetlock joint. The skin around the coronary band should be entirely desensitized. A ring block of the pastern may be a useful alternative to the ASNB, because it avoids the sometimes confusing partial desensitization of the fetlock joint that is frequently achieved with an ASNB. Low 4-point nerve block (low palmar and palmar metacarpal nerve block) (L4-PNB) (Figure 15.1): The palmar nerves are desensitized by injection of 3 mL of local analgesic solution subcutaneously on either side of the limb, between the SL and DDFT at the level of the distal buttons of the splint bones. High 4-point nerve block (high palmar and palmar metacarpal nerve block) (H4-PNB) (Figure 15.1): The palmar nerves are desensitised between the SL and the DDFT, deep to the heavy fascia of the flexor retinaculum, 2 to 3 cm distal to the level of the carpometacarpal joint. For reasons mentioned before, this nerve block becomes a 6-point block in the hind limb. Desensitization of the origin of the suspensory ligament (SL): To desensitize the most proximal part of the SL in the forelimb, the following techniques can be used: performed just below and halfway along the palmar border of the ligament between the accessory carpal bone and the proximal end of the lateral splint bone. performed at the medial aspect of the distal third of the accessory carpal bone in the vertical groove close to the palmar border of the bone. a 25-gauge, 5/8 inch needle is inserted perpendicular to skin in a mediolateral direction down to its hub, and 3 mL of analgesic solution is injected. • Lateral palmar nerve block – palmaromedial to accessory carpal bone. • Direct infiltration from both medial and lateral aspects of the limb over the proximal aspect of the SL with the limb raised. Median and ulnar nerve blocks: Median and ulnar nerve blocks desensitize the carpus and most structures distal to it. As with tibial and peroneal blocks in the hind limb, skin desensitization is not complete distal to the nerve block but only affects certain areas (see below). This makes it advisable to perform these proximal limb blocks on a different occasion to the more distal regional blocks to be able to demonstrate that appropriate skin desensitization has occurred. • Needle: 20-gauge, 1-inch (2.5-cm). • Site: In the muscular groove between the ulnaris lateralis and the flexor carpi ulnaris muscles on the caudal aspect of the antebrachium, 10 cm proximal to the accessory carpal bone, at a depth of one to two cm. Skin desensitization occurs on the proximodorsolateral aspect of the metacarpus. Tibial and peroneal nerve blocks: Tibial and peroneal nerve blocks eliminate deep sensation from the hock and structures distal to it. As with median and ulnar blocks in the forelimb, loss of skin sensation is limited to certain areas and may be inconsistent. • Needle: 19-gauge, 1.5-inch (3.7-cm). • Volume: 15 mL total (10 mL deep and 5 mL superficially). • Site: In the muscular groove between the long and lateral digital extensor muscles on the lateral aspect of the crus, 10 cm proximal to the lateral malleolus. The peroneal nerve has deep and superficial branches. Ten ml are injected around the deep branch, about 3–5 cm deep and 5 mL around the subcutaneous superficial branch during withdrawal of the needle. Skin desensitization usually occurs on the proximolateral aspect of the metatarsus. Analgesia of the navicular bursa: • Needle: 20-gauge, 3.5-inch (9-cm). • Site: The needle is inserted 1 cm proximal to the coronary band on the midline between both heel bulbs, along the sagittal plane of the foot, towards an imaginary point, situated halfway along and just distal to the coronary band. The needle hits the flexor surface of the navicular bone at this point, and 3 to 4 mL of local analgesic solution is injected. Analgesia of the distal interphalangeal joint: • Needle: 23-gauge, 1-inch (2.5-cm). • Site: The needle is inserted 1 cm proximal to the coronary band on the dorsal midline, at an angle of 15 to 45° to the horizontal, and advanced through the common digital extensor tendon. • Extra-articular structures (e.g. the navicular bone) are also desensitized by this injection even though the DIP joint and the navicular bursa do not physically communicate. Analgesia of the proximal interphalangeal joint (PIP): • Needle: 20-gauge, 1.5-inch (3.7-cm). • Site: A needle is introduced through the skin on the lateral aspect of the limb, between the lateral margin of the DDFT and the palmarolateral border of the proximal phalanx and advanced distally in a lateromedial plane towards the palmar border of the middle phalanx until the palmar pouch of the PIP joint is entered. Anaesthesia of the metacarpo/metatarsophalangeal (fetlock) joint: • Needle: 23- or 21-gauge, 1-inch (2.5-cm). • Site: Introduce the needle through the collateral sesamoidean ligament, between the palmar surface of the metacarpal condyle and the dorsal articular surface of the proximal sesamoid bone, with the limb flexed. • Alternative site – dorsally in the weight-bearing limb, to one side of the digital extensor tendons, proximal to the articular margin of the proximal phalanx. Analgesia of the digital synovial sheath: • Needle: 20-gauge, 1-inch (2.5-cm). • Site: Synoviocentesis is best performed by introducing the needle into the distal pouch of the sheath, between the bifurcating branches of the SDFT and the lateral or medial margin of the DDFT in the palmar aspect of the pastern.
Orthopaedics 1. Diagnosis of lameness/diseases of joints and bones
15.1 Diagnostic approach to lameness
History
Physical examination
Gait evaluation
 Alteration in the relative lengths of phases of the stride. The cranial phase of the stride is that part which occurs in front of the footprint of the contralateral limb, while the caudal phase occurs behind it. If the horse is moving in a straight line, the overall stride length in a pair of contralateral limbs must be even; therefore a reduced cranial phase must always be accompanied by an increased caudal phase. Overall reductions in stride length frequently accompany bilateral orthopaedic conditions leading to a ‘pottery’ or restricted gait.
Alteration in the relative lengths of phases of the stride. The cranial phase of the stride is that part which occurs in front of the footprint of the contralateral limb, while the caudal phase occurs behind it. If the horse is moving in a straight line, the overall stride length in a pair of contralateral limbs must be even; therefore a reduced cranial phase must always be accompanied by an increased caudal phase. Overall reductions in stride length frequently accompany bilateral orthopaedic conditions leading to a ‘pottery’ or restricted gait.
 Alteration in the arc of foot flight. Lowering of the arc of foot flight may occur as a compensation to reduce impact when the foot lands or to reduce limb flexion during protraction. If severe, it may lead to dragging of the toes. Exaggerated elevation of a foot due to hyperflexion of the limb joints is occasionally seen in neurological conditions, such as ‘stringhalt’.
Alteration in the arc of foot flight. Lowering of the arc of foot flight may occur as a compensation to reduce impact when the foot lands or to reduce limb flexion during protraction. If severe, it may lead to dragging of the toes. Exaggerated elevation of a foot due to hyperflexion of the limb joints is occasionally seen in neurological conditions, such as ‘stringhalt’.
 Variations in the path of foot flight and in foot placement. These may occur for similar reasons to those that cause alterations in the arc of foot flight. The foot may be swung medially or laterally during protraction of the limb. The foot may land asymmetrically contacting the ground first at the toe, heel or on one side.
Variations in the path of foot flight and in foot placement. These may occur for similar reasons to those that cause alterations in the arc of foot flight. The foot may be swung medially or laterally during protraction of the limb. The foot may land asymmetrically contacting the ground first at the toe, heel or on one side.
 Extension of the metacarpophalangeal/metatarsophalangeal joint. Pain-related lameness results in a reduction in the extension of the metacarpophalangeal joint providing there is no disruption of the palmar soft tissue supporting structures, hence making this sign a useful predictor of the lame limb.
Extension of the metacarpophalangeal/metatarsophalangeal joint. Pain-related lameness results in a reduction in the extension of the metacarpophalangeal joint providing there is no disruption of the palmar soft tissue supporting structures, hence making this sign a useful predictor of the lame limb.
Provocative tests
Regional analgesic techniques
Peripheral nerve blocks of the lower limb
Perineural analgesia of the distal limb
 Infiltration of local analgesic solution only in the region of the palmar metacarpal nerves – i.e. half of the high four-point block.
Infiltration of local analgesic solution only in the region of the palmar metacarpal nerves – i.e. half of the high four-point block.
 The lateral palmar nerve block:
The lateral palmar nerve block:
 In the palmaromedial groove of the accessory carpal bone.
In the palmaromedial groove of the accessory carpal bone.
 25 G – 5/8 inch – 2 mL of local analgesic solution.
25 G – 5/8 inch – 2 mL of local analgesic solution.
 No risk of entering the carpal sheath in one published study.
No risk of entering the carpal sheath in one published study.
 The ulnar nerve block (see below).
The ulnar nerve block (see below).
 In the hind limb the proximal part of the SL is desensitized either by direct infiltration or by desensitizing the deep branch of the lateral plantar nerve axial to the proximal aspect of the lateral splint bone. With the hind limb off the ground, a 21-gauge, 1-inch needle is introduced just distal to the head of the lateral splint bone just off the lateral border of the superficial digital flexor tendon, perpendicular to the long axis and in the sagittal plane of the limb. The needle is introduced down to its hub to a depth of 21-gauge, 1-inch needle, and 3–4 mL of local analgesic solution is injected.
In the hind limb the proximal part of the SL is desensitized either by direct infiltration or by desensitizing the deep branch of the lateral plantar nerve axial to the proximal aspect of the lateral splint bone. With the hind limb off the ground, a 21-gauge, 1-inch needle is introduced just distal to the head of the lateral splint bone just off the lateral border of the superficial digital flexor tendon, perpendicular to the long axis and in the sagittal plane of the limb. The needle is introduced down to its hub to a depth of 21-gauge, 1-inch needle, and 3–4 mL of local analgesic solution is injected.
Peripheral nerve blocks of the upper limb
Intrasynovial analgesia
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree