Ophthalmic Diseases
9.1 Ocular anatomy and physiology
Rabbits have large, prominent eyes that are positioned on the side of the head with a cornea that occupies approximately 25% of the globe. These features give rabbits a visual field of nearly 360° (they have a blind spot under the chin). However, despite their wide vision, accommodation is poor. The lens is large and spherical and the ciliary body is poorly developed (Bagley and Lavach, 1995). The retina has a horizontal area of high photoreceptor density, the visual streak, that allows the rabbit to concentrate on all points of the horizon at one time, enabling it to be aware of a predator coming from any direction (Williams, 1999). Rods are the predominant photoreceptor cells and rabbits have good nocturnal vision (Bagley and Lavach, 1995).
Rabbits are born with their eyelids closed. Separation of the eyelids occurs at about 10 days of age. The upper eyelid is shorter, thicker, and more mobile than the lower lid. Both eyelids consist of four main layers: skin, muscle, fibrous tissue and conjunctiva. The layer of fibrous tissue in the eyelids provides firmness and shape. The eyelids contain a row of 40–50 meibomian glands, which are modified sebaceous glands, arranged parallel to one another. They contain a fatty secretion derived from the breakdown of epithelial cells that originate from the stratum germinativum that lines the meibomian gland (Eglitis, 1964).
Rabbits blink approximately 10–12 times per hour (Peiffer et al., 1994). A third eyelid is present that does not actively nictitate but passively covers the cornea as the globe is retracted. It does not move more than two-thirds of the way across the cornea. Some of the palpebral hairs are larger than others and have a different root structure that contains blood sinuses, which provide an erectile function. These ‘sinus hairs’ or vibrissae have a rich sensory nerve supply and are tactile.
9.1.1 The glands of the eye
The glands of the eye are illustrated in Figure 9.1. The nomenclature for the glands of the eye in rabbits can be confusing. There are two glands associated with the third eyelids that are often collectively referred to as the Harderian gland. To conform to official veterinary nomenclature, the terms glandula palpebrae tertiae superficialis (superficial gland of the third eyelid) and glandula palpebrae tertiae profunda (deep gland of the third eyelid) are preferable. The deep gland of the third eyelid has two lobes. The dorsal lobe is white and the larger ventral lobe is pink despite a similar histological appearance (Janssens et al., 1999). The deep gland of the third eyelid can prolapse, causing swelling and protrusion of the third eyelid. It is larger in males than in females, especially during the breeding season. Within the orbit, the deep gland of the third eyelid lies adjacent to the globe and follows its contours. It is enclosed in a thin connective tissue capsule and is almost completely surrounded by the venous sinus. A duct from the gland opens on to the internal surface of the third eyelid.
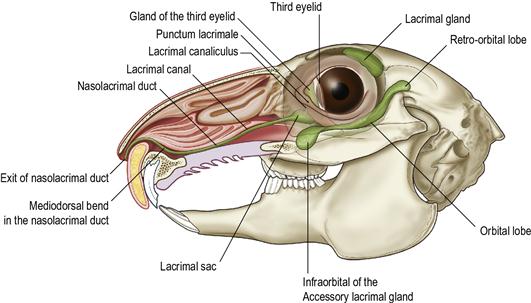
Figure 9.1 Nasolacrimal duct and glands of the eye.
The figure shows the course of the nasolacrimal duct and its relationship with surrounding structures and was drawn from dissections using Barone et al. (1973), Burling et al. (1991), Eglitis (1964) and Janssens et al. (1999) as reference sources. The aperture to the nasolacrimal duct, the punctum lacrimale, is situated in the anteromedial aspect of the lower eyelid. The punctum opens into a short (2 mm) canaliculus that opens into a dilation of the duct or lacrimal sac. The nasolacrimal duct leaves the lacrimal sac through a small aperture in the lacrimal bone (the lacrimal foramen, see Figure 9.3) into the maxilla where it is encased in the bony lacrimal canal. At the root of the primary maxillary incisor, the duct makes an abrupt mediodorsal bend and its diameter is reduced from approximately 2 to 1 mm. At this point, the duct is compressed between the alveolar bone surrounding the root of the primary maxillary incisor and the nasal cartilage. The duct then courses medially alongside the incisor tooth root and emerges in the nasal cavity at the ventromedial aspect of the alar fold a few millimetres inside the mucocutaneous junction.
There are three glands within the orbit: the lacrimal gland, the accessory lacrimal gland and the deep gland of the third eyelid. The lacrimal gland is situated in the caudodorsal sector of the orbit. The large accessory lacrimal gland lies in the lower part of the orbit and has three lobes: the orbital lobe, retro-orbital lobe and infraorbital lobe. The infraorbital lobe rests between the zygomatic bone, the superficial gland of the third eyelid and the globe. It is in close proximity with the alveolar bulla that contains the roots of the maxillary cheek teeth.
The deep gland of the third eyelid has two lobes, the white dorsal lobe and the larger, pink ventral lobe. Within the orbit, the deep gland of the third eyelid lies adjacent to the globe and follows its contours. It is enclosed in a thin connective tissue capsule and is almost completely surrounded by the venous sinus. A duct from the gland opens on to the internal surface of the third eyelid.
The lacrimal gland is situated in the caudodorsal sector of the orbit. There is also a large accessory lacrimal gland that lies in the lower part of the orbit (Eglitis, 1964). The accessory lacrimal gland has three lobes: the orbital lobe, retro-orbital lobe and infraorbital lobe (Janssens et al., 1999). The bulging infraorbital lobe rests between the zygomatic bone, the superficial gland of the third eyelid and the globe. This lobe has been confused with the zygomatic salivary gland. It is in close proximity to the alveolar bulla that contains the roots of the maxillary cheek teeth. Elongated roots of these teeth penetrate the infraorbital lobe of the accessory lacrimal gland. The glandular tissue of the lacrimal gland has marked regenerative properties. Thyroxine and testosterone stimulate growth of the lacrimal gland (Eglitis, 1964).
Secretions from the lacrimal glands and glands of the third eyelid moisten, lubricate and flush the surface of the eyeball. In rabbits, the secretion from the lacrimal gland is clear and the secretion from the glands of the third eyelid is milky (Eglitis, 1964). There are numerous goblet cells and intraepithelial cells within the fornix of the eye. The superficial epithelial cells are characterized by large osmiophilic granules (Peiffer et al., 1994). The precorneal tear film is composed of glandular secretions in conjunction with secretions from the meibomian glands and goblet cells. Tears are drained from the conjunctival sac through the nasolacrimal system into the nose.
9.1.2 Nasolacrimal system
The mechanism of tear drainage through the nasolacrimal system has been studied extensively, especially in humans (Habin, 1993). The action of blinking propels tears medially into the lacrimal lake. During blinking, contraction of the orbicularis oculi muscle causes occlusion of the punctum lacrimale and compression of the lacrimal canaliculus. This forces tears into the lacrimal sac and nasolacrimal duct. The lacrimal sac dilates during blinking and is compressed during relaxation of the eyelids. A valve mechanism is present within the lacrimal sac that prevents reflux, which aids the propulsion of tears from the eye into the nasolacrimal duct.
In rabbits, the aperture of the nasolacrimal duct, the punctum lacrimale, can be seen in the anteromedial aspect of the lower eyelid by gently pulling the lid away from the globe. Unlike the dog and cat, there is no punctum in the upper eyelid. The punctum opens into a short (2-mm) canaliculus that opens into a dilation of the duct or lacrimal sac. The nasolacrimal duct leaves the lacrimal sac through a small aperture in the lacrimal bone (the lacrimal foramen) into the maxilla where it is encased in the bony lacrimal canal (see Figure 9.1). This section of the nasolacrimal duct runs rostrally and medially until it reaches the root of the primary maxillary incisor. At this point, the duct makes an abrupt mediodorsal bend and the diameter is reduced from approximately 2 to 1 mm (Burling et al., 1991). It is compressed between the alveolar bone surrounding the root of the primary maxillary incisor and the nasal cartilage. Elongation of the root of the incisor can easily occlude the duct at this point. The duct then courses medially, alongside the incisor tooth root, and emerges in the nasal cavity at the ventromedial aspect of the alar fold, a few millimetres inside the mucocutaneous junction.
The nasolacrimal duct is lined with stratified or pseudostratified columnar epithelium richly supplied with goblet cells. In some areas, the epithelium is folded (Burling et al., 1991).
9.2 Conjunctival flora
Swabs taken from the conjunctival sac of healthy rabbits can yield a variety of organisms. Bacillus subtilis and Staphylococcus aureus, Pseudomonas, Neisseria, Bordetella, Moraxella and Pasteurella spp. are among the organisms that have been isolated from healthy laboratory rabbits (Marini et al., 1996). A survey of the conjunctival flora of healthy pet rabbits showed a predominance of DNase-negative Staphylococcus spp. followed by Micrococcus, Bacillus, Stomatococcus, Neisseria, Pasteurella, Corynebacterium and Moraxella spp. (Cooper et al., 2001). This same survey also noted that bacteria were isolated in 83% of rabbits, with rabbits under 12 months of age being more likely to yield bacteria. No statistical difference was found between different breeds of rabbit.
9.3 Examination of the eye
Examination of the eyes begins with a comparison of the size and shape, to look for evidence of exophthalmos or glaucoma. Fear can cause a bilateral exophthalmos. The eyelids open wide and the globe appears protuberant due to engorgement of the orbital vascular sinus (Eglitis, 1964). The condition is bilaterally symmetrical and no other abnormality is detected. The rabbit appears to be frightened, usually adopting a frozen, crouched stance. The bulging appearance of the eyes wears off after a few minutes. The eyes of entire males can also appear protuberant, especially during the breeding season, due to enlargement of the deep gland of the third eyelid. Vernau et al. (1995) determined that masses in the anterior thoracic cavity can also cause bilateral ocular protrusion, due to impedance of venous return from the head. The commonest cause is a thymoma. A unilateral bulging eye indicates the presence of a retrobulbar lesion, such as an abscess or tumour. A Coenurus serialis cyst has been reported in the orbit of a pet rabbit exhibiting unilateral exophthalmos (Wills, 2001). Ocular enlargement is due to glaucoma. In most cases, exophthalmos is advanced by the time the rabbit is presented for treatment and it is easy to see whether a globe is enlarged. Placing a finger over the globe to estimate how hard an enlarged eye feels can be helpful but is often unreliable. Tonometry should be used for a definitive answer. The normal intraocular pressure of rabbits is 15–23 mmHg (Williams, 1999).
Next, the eyelids should be examined for abnormalities. Eversion of the upper eyelid reveals the beige-coloured rectus dorsalis muscle attached to the sclera. The normal position and structure of the eyelids can be altered by entropion, ectropion or acquired deformities. Myxomatosis causes progressive hyperaemia, oedema and thickening of the eyelids. Severe swelling of the eyelids prevents the eye opening and secondary bacterial infections and purulent discharges develop in the later stages.
The skin surrounding the eyes should be examined for evidence of ocular discharge or epiphora. Chronic epiphora results in matted, damp fur on the skin of the nose beneath the medial canthus of the eye. Secondary bacterial infection can cause inflammation and alopecia. Lack of grooming around the eye is often the result of underlying dental disease. Sharp spurs on the maxillary cheek teeth grow into the soft tissue of the cheek and cause pain if pressure is applied to the overlying skin. Epiphora is due to either excessive tear production or impaired tear drainage through the nasolacrimal system. Excessive tear production or blepharitis can be due to conjunctivitis, keratitis, corneal ulceration or ocular foreign bodies. Impaired tear drainage is often due to elongation of the root of the upper primary incisor.
The Schirmer tear test has been evaluated in rabbits and theoretically might be of value in the investigation of epiphora. The test paper is inserted into the lower conjunctival fold in the lateral third of the eyelid and is held in place for 1 min. The amount of wetness is measured in millimetres. Topical anaesthesia is not used. Normal values for rabbits range from 0 to 11.22 mm/min, with a mean of 5.30 + 2.96. There are distinct breed differences in volume of tear production, with Netherland dwarf rabbits having unusually high tear production compared to other breeds (Williams, 2007). High values indicate excessive tear production or impaired drainage, but low values are of doubtful significance (Abrams et al., 1990). Keratoconjunctivitis sicca has not been recognized clinically in rabbits, although it has been induced experimentally. Biricik et al. (2005) compared the validity of the Schirmer tear test with the phenol red thread test for diagnosis of reduced tear production. The premise of the research was that Schirmer test strips are more appropriate for evaluating increased tear production in smaller species; however, they can cause ocular irritation and damage and thereby alter tear production. The phenol red thread test shows a colour change when in contact with tears. It is more sensitive than the Schirmer tear test for detecting dry eyes and requires a shorter contact time (15 s vs 1 min). The phenol red thread is less likely to cause ocular irritation.
Good illumination is required for examination of external structures of the globe and the uveal tract. Instillation of local anaesthetic drops and fluorescein facilitates examination of the cornea and conjunctival sac for foreign bodies and areas of inflammation or ulceration. Fluorescein can be seen at the nostrils of rabbits that have patent nasolacrimal ducts, although it can take several minutes to arrive. A prominent third eyelid may signify retrobulbar disease and exophthalmos. Samples for cytological or bacteriological examination can be taken from the fornix using a swab moistened with a few drops of sterile saline.
Mydriasis may be required for ophthalmoscopic examination of the fundus. Approximately 40% of rabbits produce atropine esterases that inactivate atropine. Tropicamide (0.5 or 1%) should be used as an alternative. The optic nerve is situated above the horizontal midline. It is necessary to look upwards into the eye with an ophthalmoscope to view the optic disc, which has a deep natural depression or cup that can be mistaken for a coloboma. Two broad white bands of myelinated nerve fibres, the medullary rays, extend horizontally from the optic disc (Peiffer et al., 1994). The retina is merangiotic or partially vascularized. There is an area of high photoreceptor density, the visual streak, which is inferior and parallel to the medullary rays. In non-pigmented rabbits, the choroidal vessels are easily seen.
9.4 Relationship between dental disease and ophthalmic conditions of pet rabbits
Dental examination is a vital part of the investigation of ophthalmic disease in pet rabbits. There is a close anatomical relationship between the roots of the maxillary teeth and the structures of the eye and nasolacrimal duct (see Figure 9.1). Root elongation and periapical infections are part of the syndrome of acquired dental disease that is so common in pet rabbits (see Box 5.1) and dental disease is often manifested by ocular symptoms. Radiology is nearly always indicated to assess the position, shape and structure of the tooth roots and their association with the structures of the eye and nasolacrimal duct.
Elongated tooth roots, especially of the upper primary incisors, can block the nasolacrimal duct and interfere with drainage of tears from the conjunctival sac. Epiphora is often the first indication of acquired dental disease (see Section 5.6.5). Examination of the teeth and surrounding structures may reveal other signs of dental disease, such as horizontal ribbing of the enamel on the incisors, or palpable swellings along the ventral border of the mandible. Blockage of the nasolacrimal duct and impaired drainage of tears from the conjunctival sac allow bacteria and debris to accumulate. Secondary bacterial infection can ensue, causing conjunctivitis and/or infection and inflammation of the lacrimal sac (dacryocystitis). Dacryocystitis is characterized by a profuse mucopurulent ocular discharge that is most marked at the medial canthus. Digital pressure on the skin just below the medial canthus expresses purulent material from the lacrimal sac through the punctum lacrimale into the conjunctival sac.
Root elongation and periapical infections of the upper cheek teeth are sometimes manifested by epiphora, conjunctivitis, dacryocystitis or exophthalmos. Elongated, distorted premolar roots penetrate the maxilla and/or the lacrimal bone and can obstruct the nasolacrimal duct. They can also grow into the orbit, causing ocular pain or infection of the periorbital structures. Retrobulbar abscesses or osteomyelitis are usually the result of periapical infection.
9.5 Congenital ocular conditions
9.5.1 Buphthalmia
Buphthalmia is an autosomal recessive trait in rabbits that causes unilateral or bilateral enlargement of the eyeball with secondary changes in the cornea. It can occur in rabbits of any breed. The age of onset is variable. Changes have been observed in baby rabbits as early as 2–3 weeks of age (Lindsey and Fox, 1994). The disease is due to a decrease in drainage of aqueous humour from the anterior chamber and a rise in intraocular pressure. Corneal oedema, conjunctivitis and increased prominence of the eyeball occur. In severe cases, corneal ulceration can result in rupture and collapse of the eye with subsequent scarring and healing. The condition can be unilateral or bilateral. Protrusion of the anterior chamber gives rise to the term ‘moon eye’, which is sometimes used by breeders to describe the condition (Bauck, 1989). At one time, it was hypothesized that vitamin A deficiency was involved in hereditary buphthalmos. The theory was tested on rabbits of the hereditary buphthalmic strain with various levels of vitamin A. However, no correlation between intraocular pressure and serum vitamin A levels could be found (Fox et al., 1982).
9.5.2 Congenital eyelid disorders
Entropion and ectropion occur in rabbits, especially in loose-skinned breeds such as the French lop. Short-nosed breeds, such as the Netherland dwarf, are prone to inadequate tear drainage and epiphora due to the conformation of the lower eyelid. Taut eyelids, a shallow medial canthal lake or mild medial lower lid entropion compromise drainage of tears through the punctum lacrimale. The natural bend in the nasolacrimal duct at the lacrimal foramen and at the base of the upper incisor can be enhanced in flat-faced individuals with a short, distorted nasolacrimal duct.
9.5.3 Conjunctival hyperplasia
Hyperplasia of the bulbar conjunctiva results in a circular flap of tissue that grows over the cornea. The condition can be unilateral or bilateral and the term ‘precorneal membranous occlusion’ has been used to describe it. The aetiology is unknown (Wagner et al., 1998).
The flap is not adherent to the cornea and often does not affect vision. Treatment is not always necessary. Surgical excision is straightforward but the membrane tends to grow back within weeks. Extending the excision to a few millimetres posterior to the limbus was successful in a case described by Dupont et al. (1995). Alternatively, postoperative topical cyclosporin therapy can be used in an attempt to prevent regrowth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


