Chapter 18 Ocular Manifestations of Systemic Diseases
Systemic diseases commonly cause associated ocular lesions and signs in all domestic species as well as in humans. Recognition of ocular signs assists both ocular and systemic diagnosis, because the eye can be examined readily. Such recognition allows earlier and more accurate diagnosis of systemic disorders as well as more effective evaluation of treatment. Ocular signs of some of the less common systemic diseases are poorly documented. Therefore this chapter focuses on the ocular manifestations of the more common systemic diseases. Ocular manifestations of neoplastic, nutritional, and dermatologic conditions as well as uncommon diseases are not discussed in this chapter; the reader is referred to standard internal medicine, oncology, and dermatology texts for discussion of these diseases.
OCULAR MANIFESTATIONS OF SYSTEMIC DISEASES IN DOGS AND CATS (Tables 18-1 to 18-16)
Infectious Diseases
Canine Viral Diseases
CANINE DISTEMPER.
Table 18-1 Systemic Causes of Eyelid Disorders in the Dog and Cat
| DISORDER | DOG | CAT |
|---|---|---|
| Infectious blepharitis* | ||
| Parasitic blepharitis* | ||
| Immune-mediated blepharitis* | ||
| Toxic blepharitis* | Sulfonamide/trimethoprim toxicity (in Doberman pinschers) | — |
| Allergic blepharitis* | ||
| Miscellaneous causes of blepharitis* | Zinc responsive dermatosis | — |
| Eyelid masses | ||
| Ptosis | — |
* The signs of blepharitis are generalized (i.e., not cause-specific); they include dermatitis, alopecia, scales, crusts, ulcers of the skin, and conjunctivitis, chemosis, and congestion of the palpebral conjunctiva.
Table 18-2 Systemic Causes of Conjunctivitis* in the Dog and Cat
| CAUSES | DOG | CAT |
|---|---|---|
| Viral diseases | ||
| Bacterial and rickettsial diseases | Mycoplasmosis (Mycoplasma felis, Mycoplasma gateae, and/or Mycoplasma arginini) has been described as a secondary opportunistic pathogen | |
| Protozoal diseases | — | |
| Parasitic diseases | Ophthalmomyiasis (Diptera spp.) | — |
| Immune-mediated diseases | Canine idiopathic granulomatous disease | — |
| Dermal diseases | ||
| Miscellaneous diseases | — |
* Associated ocular signs include ocular discharge/secretion, chemosis, congestion, and follicular hyperplasia.
Table 18-3 Systemic Causes of Miscellaneous Conjunctival Disorders in the Dog
| DISORDER | CAUSES |
|---|---|
| Conjunctival hyperemia | |
| Conjunctival/subconjunctival hemorrhage |
Table 18-4 Systemic Causes of Corneal Diseases in the Dog and Cat
| DISEASE | DOG | CAT |
|---|---|---|
| Infectious causes of keratitis*/keratoconjunctivitis | ||
| Corneal ulcers | Feline rhinotracheitis (feline herpesvirus 1 [FHV-1]) has been implicated in the pathogenesis of corneal sequestrum | |
| Primary corneal edema† | — | |
| Nonedematous corneal opacities | ||
| Keratoconjunctivitis sicca | Systemic autoimmune secretory gland adenitis (associated with hypothyroidism, systemic lupus erythematosus, etc.) | Feline dysautonomia (Key-Gaskell syndrome) |
| Symblepharon | — |
* Associated ocular signs include epiphora and discharge, blepharospasm, conjunctival congestion, corneal edema, vascularization, infiltration, ulceration, and pigmentation.
† Associated signs include corneal opacity, bullous keratopathy, keratoconus, and impairment of vision.
Table 18-5 Systemic Causes of Scleral and Episcleral Diseases in the Dog and Cat
| DISEASE | DOG | CAT |
|---|---|---|
| Scleritis/episcleritis | — | |
| Scleral/episcleral granulomas | Ophthalmomyiasis (Cuterebra spp.) |
Table 18-6 Systemic Causes of Uveitis in the Dog and Cat*
| CAUSES | DOG | CAT |
|---|---|---|
| Viral diseases | ||
| Mycotic diseases | ||
| Bacterial diseases | — | |
| Protozoal diseases | ||
| Parasitic diseases | ||
| Neoplastic diseases | ||
| Other systemic causes | Periarteritis nodosa |
* Associated ocular signs include corneal edema, flare, keratic precipitates, hypopyon and/or hyphema, hypotony, miosis, ciliary injection, blepharospasm, iris congestion, and photophobia. Secondary glaucoma and lens luxation are possible sequelae.
† Has been reported to cause secondary glaucoma.
Table 18-7 Systemic Causes of Cataract in the Dog and Cat
| CAUSES | DOG | CAT |
|---|---|---|
| Infectious diseases | Infectious canine hepatitis in neonates ([ICH] canine adenovirus 1 [CAV-1]) | — |
| Metabolic diseases | — | |
| Nutritional | ||
| Toxic causes | — | |
| Other systemic causes | Chédiak-Higashi syndrome |
Table 18-8 Systemic Diseases Causing Posterior Uveitis* in the Dog and Cat
| CAUSES | DOG | CAT |
|---|---|---|
| Viral diseases | Canine distemper | |
| Bacterial diseases | ||
| Fungal diseases | ||
| Protozoal diseases | Toxoplasmosis (T. gondii) | |
| Parasitic diseases | Ocular larval migrans (Toxocara canis) | |
| Neoplastic diseases | Lymphoma | |
| Other systemic causes | Periarteritis nodosa |
* Includes chorioretinitis and choroiditis. Associated signs include diffuse or multifocal retinal edema and hemorrhage, subretinal effusion and hemorrhage, vascular cuffing, and loss of vision. Retinal detachment and retinal atrophy are possible sequelae. Retinochoroiditis, which has a similar clinical presentation, is caused by canine distemper virus.
Table 18-9 Systemic Noninfectious Causes of Retinal/Chorioretinal Scarring and Atrophy in the Dog and Cat*
| CAUSES | DOG† | CAT† |
|---|---|---|
| Nutritional causes | Chronic vitamin E deficiency | Taurine deficiency |
| Cardiovascular diseases | ||
| Toxic causes | Sulfonamide/trimethoprim toxicity in Doberman pinschers | |
| Other systemic causes |
* Associated signs include multifocal scarring, pigment clumping, depigmentation, tapetal hyperreflectivity, and attenuation of retinal blood vessels.
† May be caused by any systemic disease causing posterior uveitis.
Table 18-10 Systemic Causes of Lipemia Retinalis in the Dog and Cat
| DOG | CAT |
|---|---|
Table 18-11 Systemic Causes of Retinal Hemorrhage in the Dog and Cat
| CAUSES | DOG | CAT |
|---|---|---|
| Infectious diseases | ||
| Parasitic diseases | Ophthalmomyiasis interna (Diptera spp.) | Ophthalmomyiasis interna |
| Cardiovascular diseases | ||
| Metabolic diseases | Diabetes mellitus* | Diabetes mellitus |
| Toxic causes | Anticoagulant poisoning | Megestrol acetate (may induce diabetes mellitus) |
| Neoplastic diseases | ||
| Other systemic causes | — |
* Has also been associated with increased tortuosity and/or dilatation of retinal blood vessels.
Table 18-12 Systemic Causes of Retinal Detachment in the Dog and Cat*
| CAUSES | DOG | CAT |
|---|---|---|
| Infectious diseases | ||
| Parasitic diseases | Dirofilariasis (Dirofilaria immitis) | Ophthalmomyiasis interna |
| Cardiovascular diseases | ||
| Neoplastic diseases | — | |
| Toxic causes | — | |
| Other systemic causes | — | Periarteritis nodosa |
* Associated signs include anterior displacement of the retina and its vessels, loss of vision and pupillary light reaction, and focal/multifocal/diffuse retinal folds. Retinal detachment may also be caused by any disease causing retinal hemorrhage, as listed in Table 18-11.
Table 18-13 Systemic Causes of Optic Neuritis in the Dog and Cat*
| CAUSES | DOG | CAT |
|---|---|---|
| Infectious diseases | ||
| Cardiovascular diseases | ||
| Neoplastic diseases | Intracranial neoplasia | — |
| Other systemic causes | — |
* Associated signs include papillary edema, optic nerve head congestion, hemorrhage of optic nerve vessels, and loss of vision and pupillary light reaction.
Table 18-14 Systemic Causes of Disorders of the Globe in the Dog and Cat
| CAUSES | DOG | CAT |
|---|---|---|
| Exophthalmos | ||
| Enophthalmos |
Table 18-15 Systemic Causes of Endophthalmitis/Panuveitis in the Dog and Cat
| CAUSES | DOG | CAT |
|---|---|---|
| Infectious diseases | ||
| Parasitic diseases | — | |
| Neoplastic diseases | ||
| Other systemic causes | Uveodermatologic syndrome | Periarteritis nodosa |
Table 18-16 Systemic Disorders Causing Blindness in the Dog and Cat
| CAUSES | DOG | CAT |
|---|---|---|
| Acute blindness | ||
| Progressive blindness |
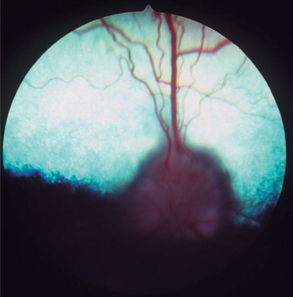
Anterior and posterior uveitis often accompany distemper encephalomyelitis and may be observed even if the dog is clinically asymptomatic for the latter. A high incidence (41%) of multifocal, nongranulomatous chorioretinitis has been found in the neurologic forms of canine distemper. Choroidal exudation may induce retinal detachment. Retinal atrophy and scarring are the chronic sequelae of chorioretinitis. In the tapetal fundus they are characteristically observed as circumscribed, hyperreflective areas with clumps of pigment in the center, whereas the nontapetal lesions are characterized by depigmentation (see Chapter 15, Figure 15-34).
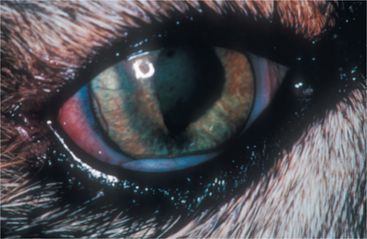
CDV has a predilection for the central nervous system (CNS), including the central visual pathways. It may cause inflammation or demyelinization of the optic nerve and tract, lateral geniculate nucleus, optic radiations, and visual cortex. Patients may present with actue, bilateral blindness and fixed, dilated pupils due to severe optic neuritis (Figure 18-1). The inflammation may be isolated, prodromal, or concurrent with other neurologic signs of canine distemper.
INFECTIOUS CANINE HEPATITIS.
Caused by canine adenovirus 1 (CAV-1), infectious canine hepatitis affects dogs and foxes. The virus is shed in the feces and urine of infected animals, and dogs are exposed through the oronasal route. After an incubation period of 4 to 7 days, seronegative animals infected by CAV-1 exhibit systemic clinical signs that range from those of a mild upper respiratory disease to those of a severe systemic disease, including hepatomegaly, icterus, and bleeding that may progress to disseminated intravascular coagulation. The prevalence of the disease has been dramatically reduced with the introduction of vaccination. Immunization with attenuated CAV-1 and, to a lesser extent, CAV-2 strains led to ocular signs of anterior uveitis and corneal edema in some animals. Dogs are currently vaccinated mostly with attenuated strains of CAV-2.
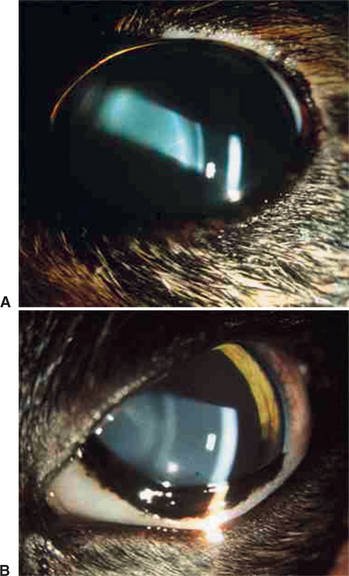
Ocular signs of infectious canine hepatitis are seen within 7 to 21 days of infection or vaccination. The signs are due to the presence of immune complexes in the eye and occur during convalescence. The initial signs include blepharospasm, miosis, hypotonicity, and anterior chamber flare (Figure 18-2) due to anterior uveitis. Corneal edema (“blue eye”) may develop within 1 to 2 days, although it is bilateral in only 12% to 28% of cases. The edema may be severe and lead to formation of keratoconus. Such cases may progress and cause corneal scarring and pigmentation. Persistent or long-lasting corneal edema may also occur, and the Afghan hound has been described as predisposed to chronic edema and glaucoma. However, in most cases the edema is transient, and animals recover spontaneously within a few days to 2 to 3 weeks.
Feline Viral Diseases
FELINE HERPESVIRUS INFECTION.
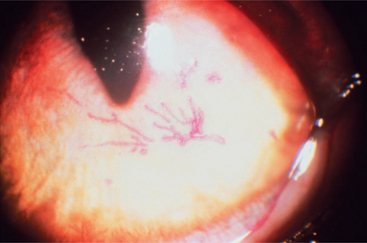
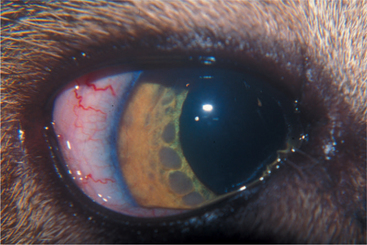
Secondary bacterial infections are common complications, especially with Chlamydophila felis. Unilateral or bilateral conjunctivitis with hyperemia, ocular discharge, chemosis, and blepharospasm are the most common lesions in adult cats with no respiratory disease. Other ocular signs are dendritic (Figure 18-3) or geographic corneal ulcers, KCS, and stromal keratitis. Symblepharon is a common sequel of infection (Figure 18-4), and FHV-1 may also play a role in the pathogenesis of corneal sequestration and eosinophilic keratitis. Vascularization of the cornea and pain may be severe or absent.
Use of human recombinant interferon, administered topically or orally, has shown synergism in vitro and has decreased the severity of clinical signs in experimentally infected cats when given 1 to 2 days after inoculation. l-Lysine, administered orally, may also inhibit viral replication. Treatment of deep corneal ulcers and necrosis includes surgical intervention. The use of glucocorticoids is contraindicated, as it may induce shedding of viral particles in the latent stage. Topical tetracycline is frequently added because coinfections with Mycoplasma spp. and/or Chlamydophila felis (formerly Chlamydia psittaci) are common. Topical treatments are frequently continued for several weeks after resolution of clinical signs to prevent recurrence.
Stress is a very important factor in the pathogenesis of the clinical disease, and events such as the introduction of a new animal to the household or traveling to cat shows may exacerbate the symptoms. For this reason, frequent treatment with multiple drugs may sometimes aggravate the clinical signs of the disease. If worsening of signs is noted, the clinician is advised to carefully consider reducing treatment rather than increasing it.
FELINE LEUKEMIA VIRUS INFECTION.
The ocular disease in FeLV-infected cats may relate to lymphoma, and transformed lymphocytes invade the globe through the uvea, leading initially to a mild uveitis characterized by corneal precipitates. Small masses may be observed on the iris (Figure 18-5), and with progression they will lead to thickening and distortion of the iris. Secondary glaucoma is a common complication because of infiltration and obstruction of the iridocorneal angle by tumor cells.
The treatment of lymphoma in cats usually requires a multidrug chemotherapy protocol. FeLV-positive cats with lymphoma treated chemotherapeutically were found to have significantly shorter remission and survival times compared with FeLV-negative cats with lymphoma treated with the same chemotherapeutic protocols. Other systemic conditions, including the ocular disease, are treated symptomatically. However, frequently the uveitis may be unresponsive to treatment or may cause secondary glaucoma, thus necessitating enucleation.
FELINE IMMUNODEFICIENCY VIRUS INFECTION.
The ocular disease manifests mainly as conjunctivitis and anterior uveitis. Pars planitis has been observed in four of nine cats with natural FIV infection. Many FIV-positive cats may exhibit a concurrent FIV- and Toxoplasma-induced ocular disease that manifests mainly as an anterior uveitis and chorioretinitis. Other ocular abnormalities reported are glaucoma (Figure 18-6) with or without uveitis, focal retinal degeneration, and retinal hemorrhages.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree