Chapter 24 New Technologies on the Horizon
Improved Diagnosis
New imaging modalities such as tissue spectroscopy and confocal microscopy are being applied to cellular surfaces with endoscopic techniques and provide innovative diagnostic information to enable three-dimensional, high-quality resolution of cells below the tissue surface and investigation of tissue properties such as blood flow or oxygen concentration. These new technologies can now identify abnormal or dysplastic cells that have the potential for future malignant transformation. This field is an entirely new area of medicine beyond the scope of this chapter, and interested readers are encouraged to pursue current reviews of literature on these topics.1
Transition to Therapeutic Procedures
Several factors in human medicine have enabled a transition from diagnostic to therapeutic endoscopy. Screening colonoscopy is the most frequently performed clinical endoscopic procedure. Colonoscopy is performed in high-risk individuals and all people older than age 50 years to aid in early detection of colonic carcinoma. Identification and treatment of early stage lesions have reduced the risk of death from colon cancer. Benign polyps are removed with an electrocautery snare. In selected cases, endoscopic submucosal resection of suspected malignant lesions is now being performed by an increasing number of gastroenterologists. Using a flexible endoscope in submucosal dissection, gastroenterologists perform an en bloc resection of mucosal lesions suggestive of cancer, sparing patients the morbidity of an invasive surgical procedure.2 The procedure was first performed on upper gastrointestinal tract lesions by gastroenterologists in Japan, where gastric cancer is quite prevalent. A number of new tools and techniques have been developed to enable these procedures to be performed safely with less risk of perforation. Therapeutic endoscopes contain dual working channels for simultaneous introduction of two devices, such as a snare and a grasping forceps. A recent development by Olympus is the R-scope3 (Olympus America, Center Valley, Pa.).
Evaluation of gastroesophageal reflux disease (GERD) is the most common reason that Americans undergo upper gastrointestinal endoscopy. The condition is manifested clinically by heartburn and is usually treated with antacids, lifestyle modification, and proton pump inhibitor drugs to reduce acid production. Prevention of acid reflux is important because the chronic reflux can lead to dysplastic changes in the distal esophagus, known as Barrett’s esophagus, a premalignant condition that can progress to esophageal adenocarcinoma. Only patients with refractory GERD or those with a severe hiatal hernia are referred to undergo a surgical procedure. The most commonly performed procedure, laparoscopic Nissen fundoplication, creates a gastric wrap around the distal esophagus to prevent reflux. Several new devices have been developed and introduced into clinical trials, aimed at addressing the incompetent gastroesophageal sphincter mechanism. The Stretta procedure, developed by Curon Medical (Fremont, Calif.), used radiofrequency (RF) energy delivered on the outside of a basket-like device on the end of a flexible endoscope. The RF energy was intended to cause controlled scarring of the tissue around the gastroesophageal (GE) junction but was abandoned because of an unacceptable risk–benefit ratio for the patients undergoing the procedure. Endoscopic injection of bulking agents, such as hydrogels or inactive polymers, in and around the GE junction has also been investigated and abandoned. A number of companies have introduced systems for plicating the tissue around the GE junction with sutures or fastening devices. One of these, the Bard EndoCinch Suturing System (CR Bard, Murray Hill, N.Y.) is currently still being sold. The company is involved in a clinical trial with a new suturing system, the RESTORe Suturing System, which is targeted at creating a sutured gastropexy for weight reduction in obese patients.4 All of these device developments were targeted as therapeutic procedures.
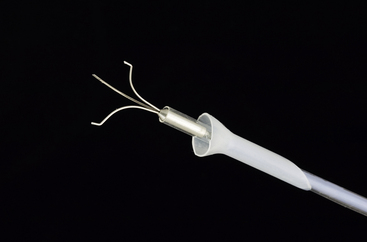
Human gastroenterologists frequently must address gastrointestinal bleeding. The two primary sources are esophageal varices and gastrointestinal ulcers. Esophageal varices are dilated submucosal blood vessels that form as a result of portal hypertension, usually as a result of hepatic cirrhosis. When the vessels erode, significant bleeding occurs. Esophageal varices are treated by injection of materials to cause scarring (sclerotherapy) or by placement of ligating bands around the dilated or bleeding vessels. Bleeding from gastrointestinal ulcers is usually addressed by application of electrocautery or endoscopic clips to stop acute active bleeding and administration of proton pump inhibitors for long-term management. Several companies have introduced endoscopic clip appliers. The Tri-Clip endoscopic clipping device (Cook Medical, Bloomington, Ind.) is currently available (Figure 24-1).
Just after expansion of therapeutic procedures, creative gastroenterologists and surgeons began to explore the feasibility of intralumenal treatment of obesity. The Garren-Edwards gastric bubble was introduced in the late 1980s and subsequently withdrawn from the market because of complications of deflation and small bowel obstruction. Fogel et al5 used the Bard EndoCinch to create a sutured endoscopic gastroplasty procedure, which was evaluated and reported in 64 patients. A second generation device is in development. Surgeons used endoscopic suturing devices to narrow the gastrojejunostomy site in gastric bypass patients that gained weight after bypass surgery.6 A sleeve stapling device developed by Satiety, Inc. (Palo Alto, Calif.)7 and the StomaphyX device by EndoGastric Solutions (Seattle, Wash.) that applies polypropylene fasteners in the stomach are currently being evaluated in clinical trials.8 These endoscopic device innovations have enabled surgeons and gastroenterologists to expand their delivery of therapeutic endoscopy.
The most significant move toward therapeutic endoscopy occurred with the introduction of natural orifice translumenal endoscopic surgery (NOTES). The field has rapidly expanded with more than 200 citations in PubMed during the past 4 years. These procedures use a natural orifice (e.g., stomach, vagina, bladder, bowel, or esophagus) to introduce a flexible endoscope into a body cavity and perform procedures under endoscopic visualization. The first laparoscopic procedure was technically a natural orifice procedure. First described in 1901, George Kelling of Dresden, Germany, introduced a cystoscope through the bladder into the abdominal cavity of a dog and advocated insufflation as a theoretical means of controlling bleeding.9 In 2004, Anthony Kalloo and his collaborators in the Apollo group introduced a technique for creating access to the abdominal cavity through the stomach in pigs.10 The technique rapidly expanded to other investigators and procedures. Exploration of the abdominal cavity, liver biopsy, fallopian tube ligation, lymph node biopsy, cholecystectomy, and splenectomy were developed in animal models.11–17 Urologists are exploring the application of NOTES for performing nephrectomy procedures through a transvaginal approach.18 An esophageal approach is being investigated as an access means for NOTES procedures in the thoracic cavity.19 We have recently demonstrated the feasibility of performing transgastric ovariectomy in dogs.20
Anticipating that the NOTES techniques might spread in an uncontrolled manner, two human societies, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and American Society for Gastrointestinal Endoscopy (ASGE), representing the surgeons and the gastroenterologists, convened a meeting in 2005 to discuss the topic and propose guidelines for technology evaluation. The collaborative group, known as Natural Orifice Surgery Consortium for Advancement and Research (NOSCAR), provides oversight for conducting research and evaluating these procedures through meetings and discussion of issues, publication of white papers, and funding of research in this area.21,22 Because NOTES procedures are anticipated to be the next revolution in endoscopic surgery, a general description of the procedure follows. In addition, several recent review articles are available.23,24
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree