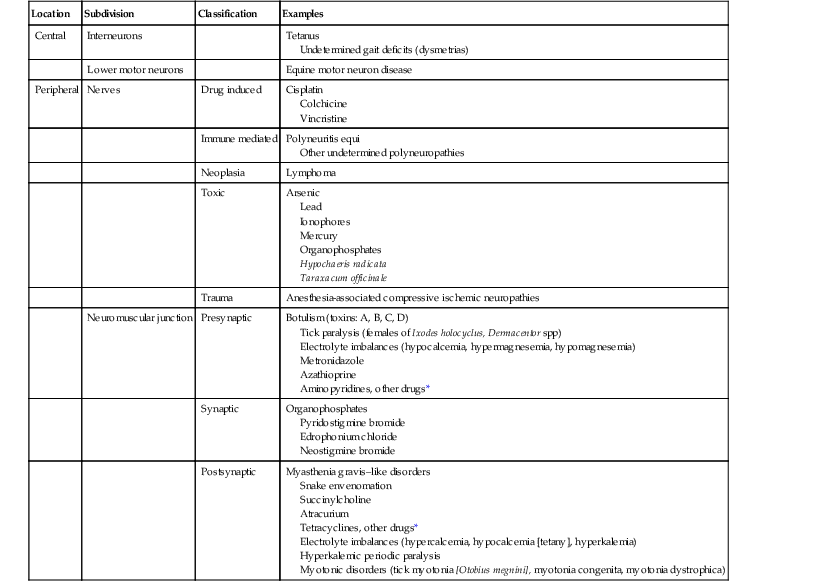
Monica Aleman The neuromuscular (NM) system, which is composed of motor units, is an important component of the nervous system. Motor units consist of a single lower motor neuron located in the central nervous system (CNS), either in the cranial nerve nuclei of the brainstem (III to VII, IX to XII) or in the ventral horns of gray matter in the spinal cord. The motor neuron reaches the periphery through its axons, located in the ventral nerve roots and spinal nerves or in the cranial nerves. The axon, which is surrounded by supportive Schwann cells that produce myelin, terminates at the NM junction. Each muscle fiber (myofiber or myocyte) is innervated by a single α-motor neuron, but a single motor neuron may innervate from a few to thousands of myofibers, depending on the function of a given muscle. In muscles such as those of the eye, which are responsible for fine movements, one motor neuron supplies only a few myofibers. In contrast, in muscles involved in posture and locomotion, hundreds to thousands of myofibers are innervated by a single motor neuron. All motor neurons innervating skeletal muscle are excitatory, and a single discharge of a motor neuron results in contraction of all the myofibers that it innervates. However, interneurons within the spinal cord can have either excitatory or inhibitory effects on the motor neurons. The NM junction or motor end plate consists of a presynaptic membrane of the axonal terminal of the motor neuron, the synaptic space, and the postsynaptic membrane and junctional sarcoplasm of the myofiber. The neurotransmitter released at the NM junction is acetylcholine (ACh), which binds to nicotinic receptors in the postsynaptic membrane and generates an end-plate potential. The end-plate potential can result in an action potential and contraction of the skeletal muscle. For more detailed information on anatomy and function of the NM system, the reader is referred to the Suggested Readings. Neuromuscular disorders may affect any component of the NM system and its supporting cells. Neuromuscular disorders are classified on the basis of the components of the motor unit that are affected as follows: neuronopathy includes disorders of the neuron cell body; neuropathy includes disorders of the nerve (degeneration of axons [axonopathy] or demyelination [Schwannopathy]); junctionopathies are disorders of the NM junction (presynaptic, synaptic, and postsynaptic); and myopathy is a disorder of muscle. Disorders can be mixed and may affect both neurons and muscles. Myopathies will not be discussed in this chapter except for those resulting from abnormal postsynaptic membrane conduction. Causes of NM disorders are summarized (Table 92-1). TABLE 92-1 Location and Causes of Neuromuscular Disorders * Presynaptic and postsynaptic effects: aminoglycosides, procaine penicillin, polymyxin B, various antiarrhythmics (quinidine, procainamide, lidocaine, phenytoin, propranolol, and verapamil). Signs of NM dysfunction can be variable depending on the specific area of the NM system affected and the severity and stage of disease. For example, flaccid paresis or paralysis can result from NM blockade or exhaustion of ACh, whereas rigid paresis or paralysis can manifest if there is lack of inhibitory input from interneurons to lower motor neurons, as in the case of tetanus. It is important to note that different NM disorders might appear clinically similar despite having different etiologies, as with botulism and tick paralysis, both of which manifest as an acute onset of flaccid paresis. Disorders affecting lower motor neurons can result in diffuse or focal muscle weakness, paresis to paralysis, decreased muscle tone, and neurogenic muscle atrophy. Cranial nerves and segmental reflexes may be normal, decreased, or absent. Muscle weakness may manifest as muscle fasciculations, low carriage of head and neck, the horse standing with thoracic and pelvic limbs under the abdomen, toe dragging, and exercise intolerance. Fasciculations can be observed in horses with botulism, tick paralysis, equine motor neuron disease, lead toxicosis, electrolyte imbalances (e.g., hypercalcemia and hyperkalemia), hyperkalemic periodic paralysis (HYPP), and West Nile virus encephalomyelitis. Lesions of specific nerves in the thoracic (e.g., suprascapular, brachial plexus, radial) or pelvic (e.g., femoral, obturator, peroneal, tibial, and sciatic) limbs result in specific gait deficits. Hypocalcemia can manifest as muscle fasciculations, colic, colic-like signs, sweating, salivation, synchronous diaphragmatic flutter, tetany, high-stepping gait, trismus, tremors, seizure-like activity, seizures, staggering, ataxia, and recumbency. In horses in which dysphagia, dysphonia, or difficult breathing has been evaluated and nonneurogenic causes ruled out, the clinician should consider NM dysfunction as a possible cause. Clinical manifestations of junctionopathies vary according to the location of the dysfunction (presynaptic, synaptic, or postsynaptic); the type of synaptic disorder (alterations in production, release, binding, breakdown, or reuptake of neurotransmitter); and the function of the specific ion channels at each location. Examples of reduced release of ACh include botulism, tick paralysis, aminoglycoside toxicosis, hypermagnesemia, and hypocalcemia. Examples of increased release of ACh include hypomagnesemia. Excitable tissues such as nerve and muscle are particularly susceptible to derangements in electrolyte concentrations (e.g., calcium, magnesium, and potassium), administration of drugs with NM effects, and toxins. These can alter function at multiple levels in the NM system. Drugs listed in Table 92-1 have been reported to cause NM dysfunction in humans and are commonly used in equine medicine, some with known or suspected NM effects. If rhabdomyolysis, cardiomyopathy, and neurologic signs are observed in horses eating commercial diets, ionophores should be considered as a cause of the intoxication. Carboxylic ionophores are used as growth promoters in poultry and livestock and are not intended for use in horses. By binding to specific cations, these ionophores disrupt transmembrane ion gradients and thereby the transmembrane electrical potentials, which results in altered function of excitable cells in nervous tissue and in cardiac and skeletal muscle. This intoxication is usually the result of accidental substituting or mixing of livestock diets for horse feed. Feed-through fly control is sometimes accomplished by use of a pelleted complete feed containing the organophosphate (OP) tetrachlorvinphos. The latter has been reported to cause toxicosis in horses. Because they inhibit cholinesterase, OP toxicosis most commonly manifests as acute signs of muscarinic receptor activation. These signs include salivation, lacrimation, urination, and diarrhea. In some cases, signs of nicotinic receptor activation (i.e., rigidity, tremors, and weakness) and central excitation (tremors and seizure-like activity) can also be observed. In severe cases of OP poisoning, rhabdomyolysis, characterized by severe necrotizing myopathy, can affect skeletal musculature, including pharyngeal, laryngeal, and respiratory muscles, and also cardiac muscle. Muscle weakness, dysphagia, nostril flare, fasciculations, low carriage of the head, reluctance to walk, and signs of muscle pain, especially involving the masseter muscles, have been observed in intoxicated horses. Disorders that affect function of the postsynaptic muscle membrane ion channels can cause muscle weakness, as in myasthenia-like disorders (exercise-induced weakness) and HYPP; or myotonia, as in tick myotonia, myotonia dystrophica, and myotonia congenita. Myotonia is characterized by sustained muscle contraction, which can occur spontaneously or is induced by voluntary muscle contraction or percussion. Myotonia can be focal, multifocal, or diffuse. Impaired gait, stiffness, and muscle hypertonicity and hypertrophy are other common signs. Muscle atrophy and weakness can follow the previous signs in progressive myotonias such as myotonia dystrophica.
Neuromuscular Disorders
Anatomy and Function
Classification
Location
Subdivision
Classification
Examples
Central
Interneurons
Tetanus
Undetermined gait deficits (dysmetrias)
Lower motor neurons
Equine motor neuron disease
Peripheral
Nerves
Drug induced
Cisplatin
Colchicine
Vincristine
Immune mediated
Polyneuritis equi
Other undetermined polyneuropathies
Neoplasia
Lymphoma
Toxic
Arsenic
Lead
Ionophores
Mercury
Organophosphates
Hypochaeris radicata
Taraxacum officinale
Trauma
Anesthesia-associated compressive ischemic neuropathies
Neuromuscular junction
Presynaptic
Botulism (toxins: A, B, C, D)
Tick paralysis (females of Ixodes holocyclus, Dermacentor spp)
Electrolyte imbalances (hypocalcemia, hypermagnesemia, hypomagnesemia)
Metronidazole
Azathioprine
Aminopyridines, other drugs*
Synaptic
Organophosphates
Pyridostigmine bromide
Edrophonium chloride
Neostigmine bromide
Postsynaptic
Myasthenia gravis–like disorders
Snake envenomation
Succinylcholine
Atracurium
Tetracyclines, other drugs*
Electrolyte imbalances (hypercalcemia, hypocalcemia [tetany], hyperkalemia)
Hyperkalemic periodic paralysis
Myotonic disorders (tick myotonia [Otobius megnini], myotonia congenita, myotonia dystrophica)
Clinical Signs
Neuromuscular Disorders
Chapter 92
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


