Chapter 11 Musculoskeletal Disorders
DIGITAL LAMENESS—LESIONS AND TREATMENTS
General principles of therapy for digital diseases are to eliminate the pain first and foremost and then to correct the underlying problem if possible. Hoof horn that is detached from underlying layers of hoof or corium should be removed. Around areas of exposed corium the wall or sole should be thinned to make the existing hoof capsule more flexible along the border of newly developing cornified epithelium. Bandages do not promote healing but may be used to control hemorrhage or to maintain some antibiotic or antiseptic in contact with a wound. Regardless of original intent, most bandages should be removed in a few days and the lesion left uncovered. Hoof blocks are an essential tool for managing painful conditions, and their use should be routine (Figure 11-1). Nonsteroidal antiinflammatory drugs (NSAIDs) such as flunixin and ketoprofen (although the latter is not approved for use in dairy cattle in the United States) should be considered to reduce the pain of some severe claw horn diseases and following surgery of the digit. Their use is not encouraged enough by most veterinary practitioners.

Figure 11-1 Polyurethane hoof block adhesive, two types of blocks, and a heat gun for drying the hoof surface.
Basic tools for lame cow therapy include left and right hoof knives and small hoof nippers. Additional tools that are in wide use are long-handled hoof nippers and electric angle grinders with carbide-toothed chipper wheels. There is a wide variety of restraint devices present on farms, and still some farms have nothing. Practitioners should encourage every client to have a safe and efficient place or device for lameness work because every herd will have lame cows, and most practitioners, at least in the United States, do not travel with a trimming chute to every call. Because most lameness occurs in the rear feet, simple devices for small herds should be made available to make rear limb lifting and examination easy. Examples are illustrated in Figure 11-2, A to C.
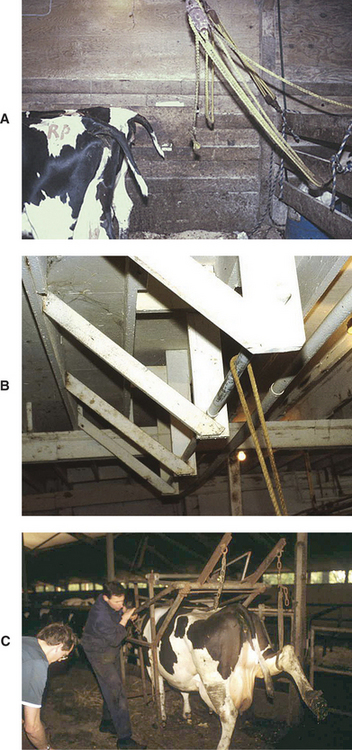
Figure 11-2 A to C, Simple devices that can provide adequate restraint and support for hoof work on rear limbs.
Overwear, Thin Soles
IncreasinglyS in large confinement dairies where cows walk long distances to and from the milking parlor and in some moderate-sized dairies using sand bedding, hooves wear away faster than new hoof is produced (Figure 11-3). There may be no other hoof diseases, but the lameness caused by subsolar bruising or exposure of the corium at the white line can be very painful. Individual animal treatment is to apply hoof blocks to allow regrowth of the overworn sole. Some hoof trimmers have suggested placing a layer of hoof block adhesive on the sole to increase its thickness and to reduce wear of the horny tissue. As a herd problem, environmental modification is indicated, which usually means installing rubber in the holding pen and travel lanes to and from the free stall pens.
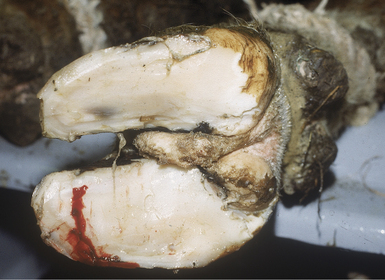
White Line Abscess
The most common location is in the posterior third of the white line of the rear lateral claw. The presence of this lesion may be detected with the response to finger pressure on the bulb of the heel of the affected digit. If the abscess is near the toe tip, it may be necessary to apply pressure with hoof testers to identify the location. In the forelimbs, the most common site is the posterior quarter of the medial claw. Usually white line abscesses are obvious after a thin layer of horn has been removed. There often is dark discoloration of a portion of the white line (Figure 11-4). Sometimes the white line is fissured with manure packed into the resulting crevice, which must be cleaned before the specific site of the abscess becomes visible. Relieving the pressure within the abscess provides some immediate pain relief. Abscesses near the heel may dissect between layers of sole horn to exit at the heel, resulting in a transverse flap of detached horn. Much less frequently than in the horse, abscesses under the wall may erupt at the coronary band. Treatment is to remove the detached horn and trim to allow walking without pressure on the inflamed corium. Large abscesses and those at the toe tip will benefit from the use of a hoof block on the healthy digit (Figures 11-5 and 11-6). Bandaging is discouraged. Most cows recover uneventfully, and reexamination is not necessary. Hoof blocks should be removed in about 4 weeks. Occasionally white line abscesses will extend into the soft tissue structures of the digital cushion and involve structures posterior to the distal interphalangeal joint. These conditions require surgical intervention that is described later.
Sole Ulcer
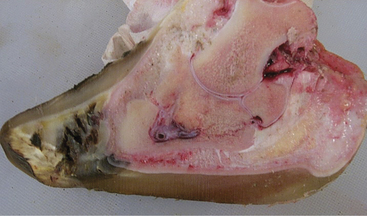
Ulceration of the sole may occur in any digit but is most common in the lateral claws of the rear feet and the medial claws of the forelimbs. Symmetrical ulcers occur in both rear limbs or both forelimbs. The typical site for ulceration is in the corium that overlies the flexor process of the third phalanx (Figure 11-7). Ulceration at the toe tip is a less common lesion in housed cattle but the most common lesion in extensive grazing dairies of the southern hemisphere. When it occurs in housed cattle, it is thought to be caused by either overtrimming at the toe or from wear that exceeds growth. A third location of ulceration is at the heel-sole junction. This may occur secondary to severe interdigital dermatitis or, as is usually seen in the medial claw of the rear foot, from unknown causes. The degree of damage to the sole and underlying corium varies from slight hemorrhage visible at trimming to complete absence of a portion of the sole to extensive necrosis of the underlying corium. The term complicated sole ulcer is used for those that have necrosis extending beyond the corium to include other tissues in the hoof.
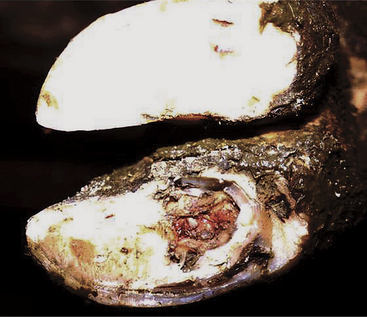
Figure 11-7 Sole ulcer in the typical site in the lateral claw superficial to the flexor tuberosity of P3.
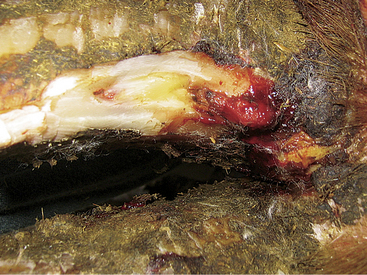
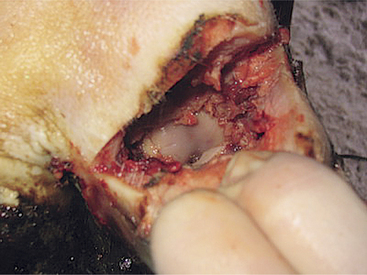
Toe Ulcer, Toe Necrosis
This condition results from overwear or overtrimming at the toe tip. The resulting thin sole at the tip is more susceptible to deformation from stepping on stones or irregular features of the flooring. If a hematoma results at the toe tip, it may lead to avascular necrosis of the soft tissues at the toe tip (Figure 11-8). If the lesion is open to the environment, miscellaneous bacteria may invade and produce osteomyelitis or pathologic fracture of the tip of the third phalanx (Figure 11-9). Conservative therapy with a hoof block and cleaning of the toe tip usually results in a chronic state of infection and mild pain. Our current approach to this problem is to place a hoof block on the sound digit and amputate the distal portion of the affected digit. Either obstetrical wire or hoof nippers may be used to remove slices of the affected digit until all tissue exposed appears healthy (Figure 11-10). A tight bandage is applied over some antibiotic powder to control hemorrhage. The bandage is removed in a few days. There is no need for parenteral antibiotics. Regrowth of functional cornified epithelium will cover the partial amputation in about 1 month. The prognosis is excellent.
Thimbling or Transverse Wall Separation
This condition results from an insult to the coronary corium that results in an interruption in growth and resulting break in continuity of the horn tubules of the hoof wall. It is not apparent until the hoof has grown sufficiently for the break point to be about 5 cm from the coronary band. It is always present in all eight digits but usually noticed because of pain in only one. The distal portion of the hoof capsule separates from the more proximal section along the entire axial, dorsal, and abaxial regions. The sole is normally attached to the younger healthy wall and the older detached wall. Pain occurs when movement of the distal portion relative to the rest of the hoof pinches the corium at the toe tip. The goals of trimming are to minimize weight bearing at the toe tip by shortening as much as possible and thinning the sole at the toe relative to the rest of the hoof. Pain may shift from one limb to another as successive thimbles become more detached from the younger hoof wall. Recovery is complete and without complications as the thimbles wear or are trimmed away.
Vertical Wall Cracks or Sand Cracks
Cracks in the dorsal or lateral hoof wall that extend from the coronary band distally are much more common in range cattle than in dairy cattle but do rarely occur (Figure 11-11). It is important to verify that the crack is the cause of lameness before proceeding. If the crack is causing pain, it should be carefully debrided of foreign material. There may be exposed corium or granulation tissue. Care must be taken to not extend the hoof wall defect during trimming. Removing granulation tissue may be necessary, followed by controlling hemorrhage and protecting the healing corium from damage. Standard procedure is to stabilize the adjacent portions of the hoof wall with acrylic and to place a block on the sound claw.
Vertical cracks in the axial wall are more common in dairy cattle although far less frequently seen than ulcers and white line abscesses. The strategy of treatment is similar to that used in range cattle, although acrylic is less often used (Figure 11-12). The greatest challenge to treatment of the axial wall cracks is to visualize and trim affected tissues in the interdigital space. Separated or detached horn should be removed, granulation tissue resected, and a tight bandage with antibiotic powder, usually tetracycline, applied. The tight bandage is to help prevent the formation of granulation tissue. A hoof block is applied to the healthy digit. Several visits may be required at about 1-week intervals to achieve healing.
Corkscrew Claw, Splayed Toes—Inherited Defects
The appearance of corkscrew claws, although inherited, does not become evident until the cow reaches 3 or more years old. Both lateral rear digits, both medial fore digits, or all four may be affected. The entire configuration of the third phalanx, the soft tissues between the claw capsule and bone, and the claw capsule are abnormal. The external appearance is of a hoof that is rotating around an axis perpendicular to the articulation of the third phalanx. The abaxial wall develops a curvature that extends the wall into the normal location of the sole. The axial wall becomes dorsal, and the tip of the toe curls up from the ground (Figure 11-13). This conformation creates a mild predisposition to lameness but of more importance is the technique required for routine trimming to prevent exposure of the corium. The toe tip should be trimmed slightly longer than normal. Removal of the overgrowth of the abaxial wall can return weight bearing to the sole and wall in a flat plane. Care must be taken near the toe tip because the corium is abnormally close to the exterior, about one fourth of the distance from the toe tip to heel. Thus the toe tip should be left about 1 cm thick. Exaggerated dishing of the axial margin of the sole may prolong the time until the next trimming is needed.
Fracture of the Third Phalanx (P3)
This injury may occur in cattle of any age or size. In a hospital population, it is observed primarily in dairy bulls, but others report that young cattle and young milking cows are predisposed. Excessive dryness of the hoof, leading to reduced cushioning of routine weight bearing, or hoof trauma may predispose to P3 fracture. Trauma from a hoof becoming stuck in a floor slot may result in fracture (Figure 11-14). The incidence of P3 fractures may be increased when fluorine toxicity exists in a herd. Hoof trauma resulting from blunt injury or falling to the ground following mounting a cow also is a suspected cause of P3 fractures.
Acute severe lameness with no weight bearing in the affected limb is observed. Careful local examination frequently reveals warmth in the affected digit, and flexion of the hoof, hoof tester pressure, and percussion all elicit a painful response from the affected animal. If one digit is affected, the cow will attempt to touch the foot down only on the nonaffected digit, if at all, when forced to walk. Occasional bilateral fractures of the medial P3 in the forelimbs have been described wherein affected cattle stand with the forelimbs crossed in an effort to bear all weight on the nonaffected lateral claws. Bilaterally affected cattle may refuse to rise on their front feet and rest on their knees, similar to laminitis patients.
Interdigital Fibroma
Redundant skin in the interdigital space is a hereditary condition associated with lax interdigital ligaments, resulting in a splay-toed conformation. It also occurs in cattle secondary to chronic interdigital dermatitis. By itself, it is not painful unless the fibroma becomes so large that the cow pinches it between the sole and floor when walking. However, fibromas predispose a risk of foot rot and are common sites of digital dermatitis in endemically infected herds. For most dairy cattle, fibromas occur secondary to interdigital dermatitis and should not be treated as a specific problem but as a reflection of the poor management of hygiene or foot bathing (Figure 11-15). There exists some pressure from farmers on veterinarians and hoof trimmers to remove fibromas as part of routine procedures, and this should be discouraged. Rather, the underlying causal factors should be addressed.
Foot Rot or Interdigital Phlegmon
Recognition of this acute disease is straightforward. The bacterial causes are Fusobacterium necrophorum and Bacteroides melaninogenicus, with both required for disease to occur. There may be other important bacterial contributors from the genus Prevotella. The cow becomes lame over the course of a day or two with symmetrical swelling above the hoof. Pain may be severe with unwillingness to bear any weight on the affected limb. Rear limbs are more commonly affected. There is a fissure in the interdigital skin with necrosis of the underlying tissues (Figure 11-16). Usually this is a dry necrosis with no exudate, but some very virulent strains of F. necrophorum may produce tissue liquefaction. The odor of foot rot is strong and characteristic. Corrective claw trimming may be used along with some topical antiseptic to the interdigital space. Bandaging is strongly discouraged so that air may reach the interdigital tissues. Parenteral antibiotics are the most important part of therapy. For almost all cases of foot rot, many antibiotics are effective and the choice is unimportant. In the United States, as of this writing, ceftiofur is registered for foot rot and requires no milk discard. There are cases of foot rot caused by multiple drug-resistant F. necrophorum. Trial and error has determined that these cases respond to treatment with tylosin at label-recommended dosages. Recognition of the presence of drug-resistant strains in a herd comes after treatment failure with the usual choice of antibiotic. It is important to verify that the disease problem is foot rot because many cases are diagnosed and treated by farmers or their employees. If the original problem was a sole ulcer, changing antibiotics will not help.
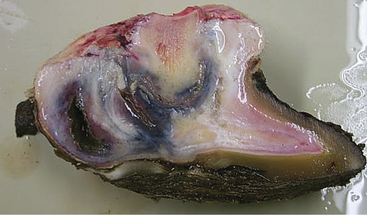
Interdigital Dermatitis, Heel Horn Erosion, and Heel Cracks
Chronic interdigital dermatitis caused by infection with Dichelobacter nodosus is very common in cattle that live in moist environments. The presence of infection may be detected in subclinically affected cattle by nonpainful erosion or ulceration of the interdigital skin (Figures 11-17 and 11-18). There is usually a moist, white exudate with a characteristic odor distinct from that of foot rot. The infection produces a mild irritation that results in underlying skin hypertrophy and may produce a faster growth rate of the adjacent axial hoof wall. Skin hypertrophy may result in an interdigital fibroma as discussed earlier or excessive horn accumulation along the axial wall. The axial wall may flare toward the interdigital space or cause an abnormally high region in the adjacent sole. Corrective trimming should remove all the excessive horn and open the interdigital space so that it is more self-cleaning and more accessible to air. If the infection spreads across the heels, it may erode the horny portion of the heel in irregular patterns or create a transverse crack at the heel-sole junction. D. nodosus produces proteases that are capable of digesting the keratin of hoof tissues.
Digital Dermatitis, Mortellaro, or Heel Wart
The condition goes by the name of hairy heel warts, strawberry foot, verrucous dermatitis, digital warts, interdigital papillomatosis, and probably most correctly digital dermatitis (or papular digital dermatitis). Since 1994 the disease has developed to epidemic proportions in most of Europe and spread throughout the United States. One wonders why a disease that was reported originally in 1974 suddenly spread worldwide in dairy cattle in the past few years. Currently researchers are still trying to define the specific cause(s); several strains of spirochete bacteria of the genus Treponema are believed to be responsible for the disease. Histological specimens of lesions stained with silver that demonstrate spirochetes reveal their presence in great numbers throughout the stratum spinosum of the dermis.
The earliest lesion recognizable as digital dermatitis is a reddened circumscribed area typically just above the interdigital cleft on the plantar aspect of the pastern, the strawberry form of digital dermatitis. The most striking feature of the lesion is the degree of pain expressed by the cow (Figure 11-19). Hairs at the periphery of the lesion are often erect and matted in exudate to form a rim. As the lesion progresses, focal hypertrophy of the dermis and epidermis leads to raised conical projections appearing much like wet, grey terrycloth. In even later stages, papilliform projections of blackened keratin may extend 10 to 15 mm from the surface, the hairy wart stage. Typical lesions may be seen affecting any of the limbs, but rear limbs are more commonly involved. The location and extent of affected skin are variable and include interdigital skin, anterior and posterior margins of the interdigital cleft, and distinct lesions that do not touch the coronary band. Many cows have simultaneous infection with D. nodosus, leading to significant erosion of the horn of the heels in a hemispherical pattern surrounding the axial space (Figure 11-20). The hoof may be noticeably misshapen from abnormal wear caused by the altered use of the limb, resulting in short rounded toes and exaggerated heel depth. Interdigital fibromas, regardless of etiology, are commonly infected with digital dermatitis in endemic herds. In our experience, after digital dermatitis has been present in a herd for a year or so, most cases of lameness are found in the first-lactation animals even though lesions may be seen on the digits of older cows during routine hoof trimming (Figure 11-21).

Figure 11-19 Typical posture of a cow with digital dermatitis affecting the plantar surface of the pastern region.
We recommend topical treatment of lame cows with oxytetracycline in the form of 5 to 15 cc of injectable 10% oxytetracycline applied on a cotton dressing with a flimsy wrap. Others use tetracycline powder under some form of bandage with or without a cotton pad. We have examined many of these cows after 2 to 5 days and have been amazed at the regression of the lesion and complete elimination of pain. Because the response is so rapid, we use less and less of a bandage so that the cotton will fall off in a few days. Reoccurrence in the same cow and even in the same location is common. Some cows in an endemic herd never develop lesions. However, all cows in endemic herds will have antibodies to at least two species of treponemes. Autogenous and commercial vaccines have come and gone with none proving efficacious in preventing the development of lesions. An apparently related skin disorder is udder cleft dermatitis on the ventral midline at the attachment of the fore udder. Histologically this lesion is undistinguishable from digital dermatitis, including the presence of spirochetes throughout the epidermis.
Deep Sepsis of the Digit
Untreated or late-treated foot rot, complicated sole ulcer, white line abscess that extends into retroarticular structures, and puncture wounds may all result in necrosis and/or infection of structures important for weight bearing. These problems have in common severe pain that is not relieved by hoof blocks or analgesic medication. Specific diagnosis of the problem may be aided by using a probe to explore fistulous tracts or by inserting a hypodermic needle (14 or 16 gauge) into joints or tendon sheaths but rarely requires radiography (Figure 11-22). Cows suffering from deep sepsis are truly suffering, and a decision should be made at the first recognition of this problem to euthanize, slaughter, or perform surgery. Too many cases receive no treatment or systemic antibiotics in the hope that the problem will somehow resolve spontaneously (Figure 11-23). These cows deserve a more humane approach.
Surgery of the Digit
Anesthesia is most easily performed by intravenous infiltration of lidocaine distal to a tourniquet on the metatarsus or metacarpus. Lidocaine without epinephrine, 20 to 30 ml, is infused using a butterfly catheter (19 gauge, 15 to 25 cm) (Figure 11-24). Any accessible vein will result in complete anesthesia of both digits after a few minutes. If no vein can be found, regional perfusion above the intended surgical site is an alternative. The distal limb is scrubbed and disinfected as for any surgery but usually not shaven because the hair is typically very short or absent. Surgical procedures are commonly done in the field and are considered “clean” procedures but not sterile. The goal is to debride necrotic tissues and provide drainage for pus and exudate. If a hoof block is to be used as part of the therapy, it should be attached before the surgery because adhesives require dry hoof to bond. Injecting the lidocaine followed by applying the block or scrubbing the area ensures adequate time for diffusion of the anesthetic to all tissues distal to the tourniquet.
Digit Amputation
Amputation of one digit at the proximal interphalangeal joint or just above is a common procedure in cattle practice. After preparation, a skin incision is made in the interdigital space and then beginning about 2 cm proximal to the interdigital cleft angling upward to a point on the lateral or medial side of the leg even with the distal margin of the accessory digit or dewclaw. All soft tissues can be sharply incised along the line of the skin incision. Obstetrical wire is then placed between the digits, and the distal end of the first phalanx is cut (Figure 11-25). If the cut misses this landmark and a portion of the second phalanx remains proximal to the cut, it should be removed. If the articular surface of the first phalanx is intact, it should be roughened with a knife. Alternatively, the digit may be amputated by sharp dissection to disarticulate the proximal interphalangeal joint (Figure 11-26). Some practitioners ligate one or two arteries, and others simply use a very tight bandage. The cut surface of the removed portion should be carefully examined for evidence of sepsis or necrosis. If damaged tissue extends above the amputation and it is not debrided, the outcome will be poor. After determining that all diseased tissue is removed, the surface of the wound is covered with an antiseptic or antibiotic dressing and a bandage applied to control hemorrhage. The bandage should be removed or changed in about 1 week if there was no need for maintaining drainage of septic regions proximal to the incision. If a tendon resection is performed, the bandage should be removed in 2 or 3 days. Depending on the environment in which the cow must live after surgery, either no bandage is placed after the first one is removed or a light wrap to minimize painful contact with environmental objects is used. Parenteral antibiotics are usually given for 5 days.
Flexor Tendon Resection
If, after amputation, it is evident that sepsis extends proximally along the deep flexor tendon, it should be resected. A 3-cm incision parallel to the path of the tendon is made over the affected branch of the flexor tendons beginning just proximal to the accessory digit. There is strong fascia surrounding the sheath of the combined superficial and deep flexor tendons. In fact, the superficial flexor tendon forms a tube around the deep at this level. Sharp dissection oriented along the skin incision through the superficial flexor tendon will reveal the deep flexor tendon. The deep flexor tendon is grasped with a strong instrument such as a dental extractor or exteriorized with the aid of curved hemostats (Figure 11-27). There may be adhesions of the deep flexor tendon to surrounding structures at the level of the distal transaction that require sharp dissection. In some cases, the tendon will simply be pulled to the outside from the proximal incision. The deep flexor tendon is transected at the most proximal exposed part, and surgical drainage tubing is placed through its original course to exit at the distal incision. It may be knotted into a loop or each end affixed by suture. One or two skin sutures are placed in the proximal incision. Systemic antibiotics are routinely given for 5 days. The drainage tubing is removed in 2 weeks.
Retroarticular Abscess
White line abscesses near the heel, penetrating foreign bodies, and deep flexor tendon avulsion or fracture of the flexor process of the P3 all may result in severe lameness with extensive painful swelling of the heel region of a single digit (Figure 11-28). Following anesthesia and standard surgical preparation, an incision is made into the heel bulb. The choices are a vertical incision extending into the sole (after paring away enough sole at the heel so that it is thin enough to make an incision with ordinary surgical instruments) or a transverse incision in the middle portion of the cornified heel. Exploration of the cavity encountered will dictate further steps. If the limits of the abscess or hematoma do not involve the navicular bursa or deep flexor tendon, the prognosis is excellent and resolution should be prompt. The cavity is flushed with water and mild disinfectant such as povidone iodine. A surgical drain is inserted in the wound and affixed with sutures. Antibiotic powder is placed in the cavity, and the incision is closed with a few skin sutures. A hoof block should be placed on the healthy digit. If the condition resulted from mechanical disruption of the deep flexor tendon or an avulsion fracture of P3, there is risk of involvement of the navicular bone and bursa. If no sepsis is evident, the outcome should be satisfactory. The cow will probably need the hoof block renewed in 1 month, but no further treatment is necessary.
Septic Distal Interphalangeal Joint
When the distal interphalangeal joint is septic, there is enlargement of the joint space and distention of the joint capsule. This may be observed as painful swelling at the coronary band in the caudal third of the abaxial coronet. It is possible to insert a needle into the joint capsule through the coronary band to verify the nature of the joint contents. In those cases when there is no swelling of the heel or deep flexor tendon, a simple fenestration of the joint may result in a satisfactory cure following ankylosis of the joint. The most common means of this sepsis occurring are secondary to foot rot or to a complicated sole ulcer. In either case, after anesthesia and cleaning the sole, if it is intact, a 7- to 12-mm (⅜ to ½ in) drill is used to fenestrate the joint. Beginning in the typical site for sole ulcer, the drill is directed in a sagittal plane to exit the digit just at the coronary band on the dorsal surface (Figure 11-29). This will satisfactorily provide drainage of the joint. Surgical tubing or braided nylon rope is passed through the drilled hole and tied around the abaxial side of the hoof (Figure 11-30). A block is placed on the healthy digit, and systemic antibiotics are given for 5 days. The drain is removed in 2 weeks. Full ankylosis requires several months, but the cow will usually be sound without a block in 1 month.
Extensive Deep Sepsis of the Digit
Amputation is an acceptable therapy for extensive deep sepsis of the digit. However, claw-sparing procedures have been adapted for field use and provide excellent results. We have combined the transverse heel incision (Figure 11-31) described above with drilling through the distal interphalangeal joint, navicular bone resection, and deep flexor tendon resection to resolve some extensive problems with deep sepsis. A hoof block should be applied before beginning surgery. The approach is as for retroarticular abscess but includes incising deeply just proximal to the navicular bone. This will transect the deep flexor tendon if it is still intact. Through the same skin incision, a more distally directed incision is made to cut the distal attachments of the navicular bone and remove a wedge of tissue. In some cases, the navicular bone and its attachments are so necrotic that it has already disappeared or is easily removed through this incision, allowing visualization of the distal interphalangeal joint (Figure 11-32). If the collateral ligaments are intact and difficult to incise, use a 5-mm (¼ in) drill to make a hole in the center of the navicular bone. Insert a stout metal rod or screwdriver into this hole to fracture the bone into two pieces. Each piece can then be grasped and twisted to rupture any remaining attachments. A useful inexpensive tool for this procedure is a canine dental extractor. If the flexor tendon is necrotic or septic, it should be resected as described above. Use a 7- to 12-mm (⅜ to ½ in) drill to fenestrate the distal interphalangeal joint through the incision. To exit at the coronary band it will be necessary to overextend the distal interphalangeal joint. Surgery tubing should be placed through the joint and secured in a loop around the axial side (Figure 11-33). If tendon was resected a drain should be placed there as well. If there was an existing fistula that is not connected to the transverse heel incision, it should also have a surgical drain. Once all drains are in place, antibiotic powder is placed in the heel incision, and the incisions are closed with a few skin sutures. Parenteral antibiotics should be given for 5 days, and all drains should be removed in 2 weeks. We do not recommend wiring the toes of the two digits together as is done by others. The intended ankylosis of the distal interphalangeal joint will proceed more quickly if there is no motion in the joint. If the digits are fastened together, every step will cause motion of the joint receiving surgery. The block may need replacement at 1 month.
FUNCTIONAL ANATOMY OF CATTLE DIGITS: WHAT GOES WRONG THAT RESULTS IN LAMENESS
Introduction to Biomechanics
Why do we see more disease in rear feet than fore? Why is there more disease in lateral rear claws than medial? The fore versus rear argument in dairy cattle has three components. The rear limbs of dairy cattle are forced to carry weight in excess of the original design criteria. The wild-type cow that gave us our modern dairy cows never had a large udder, even at calving. As geneticists have selected for more milk production, we do not think they have been able to simultaneously modify the musculoskeletal system to accommodate this extra weight at the rear of the cow. Second, the forelimbs are attached to the body by elastic components versus the direct bony connections in the rear limbs. Concussive forces created during locomotion must be absorbed by the digital cushion and the flexion of the hock and stifle. Third, rear feet are always more exposed to the bacteria and moisture of manure and urine. The skin near the hooves is more likely infected with bacteria as a result of maceration by this moisture, and the hoof capsule is softer because of greater hydration. The medial versus lateral argument is potentially more confusing. Lateral claws grow about 10% faster than medial claws and wear about 8% more in free stall-housed Holsteins. Thus lateral claws can progressively outgrow medial claws. They are larger even in fetal calves. Larger lateral claws are more heavily loaded than medial claws. Larger loads result in more potential for mechanical insults. Cows may adopt a toed-out posture to help equilibrate the weight between the rear claws when overgrowth and some discomfort occur. This toed-out posture or being “cow hocked” can be used as an indicator of the need to trim an individual cow or by population evaluation to determine when a group or herd needs trimming.
It is important to note that the lesions of the corium that we recognize as and call laminitis require weight bearing during the period of primary damage to the corium. No one knows how long episodes of altered permeability and edema last following the chemical messengers from ruminal acidosis. However, if the cow did not stand during that period, there would be no mechanical damage to the corium. In the vast majority of cases, the lesions within the claw that we call laminitis are the consequence of standing or walking on damaged corium. Standing is perhaps a worse insult to the corium than walking. With each step there is normal movement of P3 within the horny capsule of the claw. This movement results in periodic perfusion of parts of the corium. When a cow stands without shifting her weight, these periodic changes in blood flow within the corium are probably interrupted. Thus standing motionless is potentially more damaging to an already insulted corium than walking. Only in the rarest cases do the lesions of laminitis develop while cows are lying. Thus the great stress in recent years on cow comfort and maximizing opportunities through time management and providing attractive lying surfaces are antilaminitis efforts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree