Romain Pizzi
Minimally Invasive Surgery Techniques
Minimally invasive surgery (MIS) techniques such as laparoscopic cholecystectomy and appendectomy are used routinely in human surgery in the developed world and are currently regarded as the gold standard for these and numerous other human surgical procedures.17,32,33,63 They demonstrate notable improvements in rapid recoveries and reduced postoperative pain compared with traditional open surgery. Veterinary MIS techniques also hold the potential for reduced patient morbidity, reduced wound contamination and breakdown, shorter patient recovery periods, and reduced postoperative care requirements.6,15,25,30,31,35,64 It stands to reason that MIS is likely to hold even greater advantages in captive or free-ranging wildlife than in domestic animals, although the current evidence base is still small.
Although wildlife surgery is a small specialist field, it can still play an important role in zoo and free-ranging wildlife medicine. MIS has obvious welfare advantages for permanent captive wildlife species as well as for free-ranging wildlife species undergoing rehabilitation, potentially shortening the stressful time of treatment in captivity. Wildlife surgery may also play an occasional role in the conservation of endangered species. In critically endangered species, optimal treatment of each remaining individual is important if a species is to survive and maintain reasonable genetic heterogeneity. For example, only four Yangtze giant soft shell turtles (Rafetus swinhoei) remain in the world, of which 2 remain in the wild, and one of these last remaining wild turtles recently required capture and surgical treatment for wounds.3 Similarly, other critically endangered species exist, with small remaining wild populations under 50 individuals. Successful surgical treatment and return to the wild of even a single injured individual in such small critical populations could have an important impact on maximizing the remaining genetic diversity in the population. In these cases, the least invasive method of intervention with the most rapid healing and return to the wild would be ideal.
This chapter will provide a brief overview of current techniques and applications of MIS in wildlife, highlight MIS-specific risks and disadvantages, and discuss some recent developments in human and domestic animal surgery that have relevance or implications for wildlife surgery. Several available texts provide detailed discussions of the basic MIS equipment and instruments needed for most animal species and describe the basic procedures commonly performed in humans, domestic animals, and exotic pets.10,15,20,26,39,40,60
Overview
The term minimally invasive surgery (MIS) is generally used to refer to any procedure that is less invasive than open surgery used for the same purpose.65 Although this has most often been used to refer to rigid endosurgical procedures such as laparoscopy, the term can also be applied to percutaneous interventional techniques.
Laparoscopy, thoracoscopy, and arthroscopy are also alternatively referred to as minimal access surgery, video surgery, endosurgery, and endoscopic surgery and, by lay persons and professionals alike, as “keyhole surgery.” It appears advisable to avoid the use of the term “keyhole surgery” as some ambiguity surrounds the meaning of this term; for example, it is not uncommon for veterinarians to also refer to open surgery performed through small incisions as “keyhole surgery.” Small wounds are a clearly recognizable feature and an obvious benefit, but these small wounds are not the only benefit of this type of MIS. A very notable benefit is the markedly enhanced visualization (helped by the magnification allowed by the endoscope), which, if used correctly, leads to safer and more physiologic surgery. The ultimate aim of all MIS should always be safe, visual physiologic surgery, the added benefit being small wounds. In contrast, very small open abdominal surgery incisions tend to lead to poor visualization and result in unsafe surgery.40
Laparoscopy and Coelioscopy
Laparoscopy encompasses MIS procedures in the abdominal cavity. Coelioscopy, which is endoscopy of the coelomic cavity in nonmammalian species, is also commonly referred to as laparoscopy, although this usage is not strictly accurate. This is the most widely recognized and the best reported MIS technique in the zoo and wildlife surgical field. It has been applied in mammal species ranging from mice56 to elephants,58 as well as in birds, reptiles, amphibians, and fish.10,39 It has applications in diagnosis, surgery, and assisted reproduction in wildlife. The emphasis in this chapter is on laparoscopy and coelioscopy, as still relatively few reports on the application of other MIS modalities in wildlife have been published.
Thoracoscopy
Thoracoscopy holds potential for further application in zoo animal surgery. Maintenance of postoperative chest drains commonly employed in open thoracotomy procedures is difficult in wildlife patients. Many human surgeons prefer the term video-assisted thoracic surgery (VATS) to thoracoscopy, which highlights one of the main benefits that endosurgery brings to thoracic surgery—visualization. Endoscopic visualization allows examination of parts of the pleural cavity, which are difficult to access or see adequately in open thoracotomy procedures. VATS also recognizes that although the majority of a procedure such as a lung lobectomy can be completed thoracoscopically, a mini-thoracotomy is usually still needed for tissue extraction. In laparoscopy, alternatives such as insertion of hand access ports, motorized tissue morcellators, and rip-proof impervious extraction bags allow an entire liver lobe to be broken down with sponge forceps and extracted through a 10- to 15-millimeter (mm) port site.
Currently, published thoracoscopy reports have largely been limited to those on laboratory primates such as macaques4 and domestic animals.40 Postmortem thoracoscopic access was assessed in an adult giraffe, but visualization and access were notably limited by the wide, closely spaced ribs that allowed for little angulation of the endoscope and instruments,44 which is also an issue with other large herbivores and megavertebrates. Access was, however, sufficient for peripheral lung biopsies. Thoracoscopy is not possible in elephants because of the lack of a pleural space.8
Vascular ring anomalies such as persistent right aortic arch have been treated in zoo animals such as a tiger by open thoracotomy,22 and the procedure has been performed in domestic animals via 3-mm thoracoscopy,40 making this equally applicable in zoo animals not intended for breeding. Esophageal hiatal hernias, diaphragmatic hernias, and chylothorax, reported in zoo species,19,21,23,29 are amenable to operative thoracoscopy techniques.
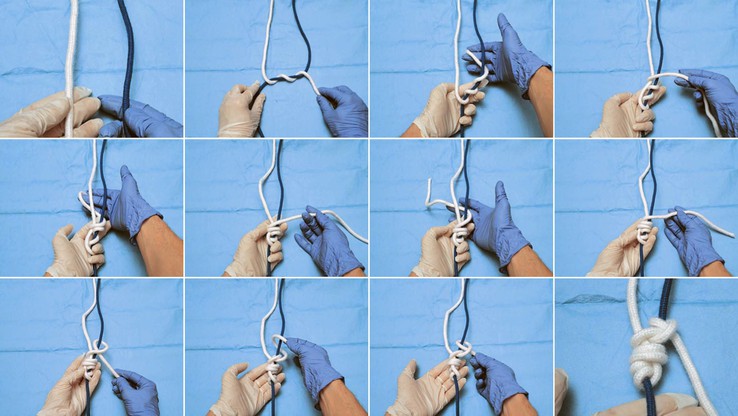
The extracorporeal applied Meltzer knot (Figure 72-1), which is an extremely useful technique for performing lung biopsies, also has other MIS and open surgery applications. It can be used in a wide range of taxa and body sizes, in cases where alternatives such as endosurgical staplers cannot be used. It is more cost effective than staplers or commercially available pretied endoloops (Surgitie, Covidien; Endoloop, Ethicon). This also allows surgeons greater choice of suture material and diameter than commercially available endoloops. The author has used this in species ranging from 1 to 650 kilograms (kg), via 3-mm ports and larger ports in thoracoscopy and laparoscopy. A loop with a pretied Meltzer knot is inserted via one port with a knot pusher and grasping forceps inserted via a different port. The forceps end is passed through the loop to grasp the tissue to be ligated for purposes such as biopsy. The tip of the knot pusher is then placed on the tissue where ligation is required, and the suture loop tightened, thus locking the knot. Knot ends of about 1 centimeter (cm) length should be left for safety. The tissue may then be transected. A suture may also be first passed around a fixed structure such as the cystic duct or ligamentum arteriosis before the suture exits from the same port, and the knot is then tied and similarly placed with a knot pusher for ligation.
It is inadvisable for surgeons not already familiar with standard thoracotomy techniques to attempt thoracoscopic procedures. An emergency situation such as intrathoracic hemorrhage is not the time to learn how to perform a thoracotomy. During surgical preparation and draping, the decision to convert to a thoracotomy, if needed, may be determined.
Arthroscopy
Surprisingly few reports of arthroscopic surgery in wildlife species have been published, considering how widespread and established the use of this MIS modality is in domestic animals. Two reports of arthroscopy in giraffe—one of arthroscopic treatment of a metacarpophalangeal joint injury and osteochondral fragment,50 and the second of exploratory arthroscopy in the femorotibial joint of a giraffe with an avulsion fracture of the peroneus tertius origin—have been published.49 Arthroscopy has also been reported in the Dromedary camel,2,36 alpaca, and llama.37With the increased longevity of zoo animals and the associated needs for diagnosis and management of geriatric conditions such as osteoarthritis, arthroscopy is likely to be increasingly performed in individual zoo animals in future. Arthroscopy also has a potential role to play in the diagnosis of some dysplastic joint diseases that may have heritable factors, with subsequent implications for captive breeding.
Further studies are needed to clarify optimal safe entry sites in the joints of different species, particularly in species that markedly differ anatomically from domestic animal models and humans. Poor site selection for joint entry or lack of experience in the operators poses the risk of cartilage and joint damage. In larger animals, as in domestic equines, insufflation of the joints with carbon dioxide may be helpful in improving visualization.51
Percutaneous Surgical Interventions
Interventional procedures include interventional radiology, interventional cardiology, and ultrasound-guided procedures. Some conditions that were surgically managed previously are increasingly performed via percutaneous techniques, which hold potential applications in wildlife species. These include occlusion of patent ductus arteriosis, balloon valvuloplasty for pulmonic stenosis, cardiac pacemaker implantation, and attenuation of single portosystemic shunts, performed under fluoroscopy. These percutaneous techniques are all based on the Sildinger technique of vascular access.55 The implantation of a cardiac resynchronization device in a gorilla has been reported,52,53 and in the future more interventional procedures may be used for managing the health and welfare of nonbreeding great apes, carnivores, and other charismatic exhibit animals.
Ultrasound-guided procedures are also replacing surgical procedures used previously and even other more invasive MIS techniques such as laparoscopy in some applications. Much of the initial research on wildlife laparoscopy was focused on its applications in assisted reproduction, such as examination of ovaries, artificial insemination, and oocyte retrieval.5,8 These applications of laparoscopy are increasingly being replaced by ultrasonography, transcervical insemination, and transvaginal ultrasound-guided fine-needle techniques. Transrectal ultrasound-guided oocyte recovery has been performed in white and black rhinoceroses,18 in which, as in other megavertebrates, laparoscopic access to the ovaries is not easily achieved.44,58
Other Endosurgical Techniques
Other rigid and flexible endoscopic modalities may be used for both diagnostic and operative applications, although only a small number of reports of their operative use in wildlife have been published. Operative rhinoscopy has been used to remove obstructing nasal polyps in a chimpanzee12 and a California sea lion.57 Endoscopy, in conjunction with fluoroscopy, may be used to apply temporary or permanent stents. Urethral stenting, in conjunction with laser lithotripsy, has been used in a bottlenose dolphin54 and an Asian small-clawed otter.66 Bilateral urethral stenting in a Guinea baboon has been reported in the management of urethral strictures caused by endometriosis that occurred after an ovariohysterectomy.9 The author is unaware of any reports of permanent stenting for tracheal collapse in zoo animals, but the technique appears feasible in many mammalian species, should it be needed.
Natural orifice transluminal endoscopic surgery (NOTES) has been investigated for its potential for truly “scarless” surgery in human abdominal surgery. Transvaginal and transgastric cholecystectomies have been performed in humans, as an alternative to laparoscopy or open surgery. However, the use of NOTES in human surgery is still highly controversial and has only been performed in a small number of cases. Besides studies in laboratory animals, NOTES has been investigated experimentally in domestic horses for standing bilateral ovariectomies with reasonable initial technical results.34 Transvaginal laparoscopy for oocyte retrieval was investigated in a black rhinoceros,48 as a potential alternative to flank laparoscopy, but the technique was problematic and has been replaced by other less invasive methods such as an ultrasound-guided fine-needle transrectal technique,18 which appears safer and more feasible.
Cosmesis is the main reason for the development of NOTES in human surgery and is of little concern in wildlife patients. The need for expensive specialist equipment such as double-channel operative flexible endoscopes; difficulties in monitoring surgical entry sites in the stomach, rectum, or vagina postoperatively; increased technical difficulty and increased procedure time; and ongoing controversy over its safety and benefits in humans make it unlikely that NOTES will find much application in wildlife surgery in the near future.
Current Knowledge
Evidence for the advantages of MIS in domestic animals is increasing,30 but further research is still needed to better establish an evidence base for the safe, relevant, and ethical application of MIS techniques in captive and free-ranging wildlife patients. The current literature on MIS in wildlife species consists largely of concept trials and case reports and is likely to have an unintentional positive publication bias. Type II error, that is, not meeting sample size requirements, is a particular limitation in surgical trials, even in human medicine.
The large sample sizes needed to demonstrate statistical significance of low-frequency adverse events is problematic in wildlife surgery, with the relatively small numbers of procedures performed. Preemptive power calculations highlight how difficult it would be to perform a randomized controlled trial to demonstrate the reduced complication rates in wildlife MIS compared with open surgical techniques. Demonstration of a 50% reduction in baseline risk from 20% to 10% would require a total study group of 438 individuals. Demonstration of a more modest improvement, or a lower frequency event requires even larger numbers: Demonstration of a 50% reduction in baseline risk from 2% to 1% would require a study group of 5030 individuals; and demonstration of a 10% reduction in baseline risk from 20% to 18% would require a study group of 12,278 individuals.7 At least for the foreseeable future, the evidence base for wildlife surgery, including MIS, is likely to continue to be based on small feasibility trials, case series, case reports, and anecdotal experience. The profession needs to debate on and determine the ethics of what is not only possible but also reasonable. Increasing surgical capabilities make correction of numerous congenital abnormalities and other previously untreated conditions feasible, but the possibility of unknown heritable components and the implications for the genetic viability of captive populations of endangered animals require consideration.
Cognitive Bias in Wildlife MIS
Cognitive bias caused by heuristics and subsequent errors in decision making need to be recognized in wildlife MIS.61 Veterinary surgeons able to perform MIS may inadvertently be subject to the risk of “technology bias,” or “law of the instrument,” which is summed up by Maslow as follows: “If the only tool you have is a hammer, everything looks like a nail.”28 All surgery, even MIS, is invasive and carries risks of adverse consequences for the patient. A 2010 study in the British Journal of Surgery found that not only were a significant number of human elective surgery patients not better a year after elective surgery, 17% actually suffered worse pain than before surgery, and 14% had less function than before surgery.38 This indicates that approximately 1 in 7 human elective surgery patients are, in fact, worse off a year later after the surgery. No comparable veterinary data are available, but it is uncertain whether veterinary surgical patients fare any better. It is strongly recommended that wildlife surgical decisions be routinely discussed with nonsurgical colleagues, to evaluate if a procedure is technically feasible and if it, in fact, is indicated, carries a reasonable likelihood of a successful outcome for the patient, and another equally applicable nonsurgical option is not available. Without this consideration, everything may start to resemble “a chance to cut being a chance to cure,” rather than “Primum non nocere” (“First do no harm”). Auditing surgical outcomes is vital to improving surgical skills and reducing complications, as well as to improving future surgical decisions.
MIS being less invasive does not always mean that it is better than open surgery. Recent systematic reviews have found no evidence for better long-term oncologic or functional outcomes among open prostatectomy, laparoscopic prostatectomy, and robotic radical prostatectomy in men.14,24
Wildlife surgeons may benefit from surgical research into nonpatient factors that affect surgery on humans, domestic animals, and wildlife equally. Even relatively small changes in surgical practice may have a large influence on patient safety and outcomes. Under the World Health Organization (WHO) “Safe surgery saves lives” initiative, the use of a simple surgical checklist in human surgery has been found to reduce surgical complications by more than one third and reduce deaths by almost half.27 A safety checklist modified for veterinary endosurgery can be downloaded from http://www.veterinarylaparoscopy.com/Vet endosurgery safety checklist.pdf.
Cognitive bias may also lead to the belief that new equipment or additional instrumentation would improve surgical capabilities and the procedures that can be performed, when the procedures may not, in fact, be necessary. The author is aware of several hundred laparoscopic cholecystectomies safely and rapidly performed by experienced surgeons in human medicine working in developing countries, when electrosurgery was not available, simply by careful and meticulous dissection.59 When performing laparoscopic cholecystectomies in bears (Figure 72-2), self-tied extracorporeal knots may be the only viable option for ligation of the cystic duct, as clips are too small and access for 12-mm diameter endosurgical staplers is insufficient.45
In human surgery, some surgeons wish to further improve cosmetic results by reducing the number and diameters of ports used in MIS procedures. This has culminated in the controversial “scarless surgery” approaches of the natural orifice transluminal endoscopic surgery (NOTES) previously mentioned, as well as single incision laparoscopic surgery (SILS). SILS is performed by inserting a single, large, multiple-instrument cannula via the navel, with the resulting umbilical scar remaining hidden after surgery. The improved cosmetic result comes at the cost of several other compromises. The incision and body wall deficits are larger, at least 2 to 3 cm, and carry a greater risk of developing postoperative hernias and other complications. Visualization and instrument angulation are markedly more restricted, with limited ability to mobilize tissues; this results in notable increases in surgery times, requires greater technical skills from the surgeon, and results in increased surgical risks.
Some reported veterinary SILS procedures are only from proof-of-concept technical feasibility studies, without strong evidence regarding patient benefit or safety to justify many applications in wildlife surgery. SILS may perhaps have a role to play in the removal of large, firm organs such as the spleen in carnivores or in nephrectomy, when a morcellator is not available or the tissue is not amenable to pulping in a rip-proof impervious bag (E-sac, Espiner Medical), followed by suction or piecemeal removal from the exteriorized neck of the bag via a slightly enlarged standard port site wound. In many mammals, a liver lobectomy (performed by means of an extracorporeal knot) can be effectively performed by this means. In wildlife patients, a single, larger wound is generally less desirable than several smaller incisions because of the increased risks of wound interference, complications, and herniation.
Emphasis is commonly placed on the small wounds and reduced postoperative pain in veterinary MIS. However, the enhanced magnified visualization, access to parts of the body and structures difficult to visualize in open surgery, provision of excellent illumination, and ability to perform less traumatic and more physiologic surgery in MIS are also of considerable value to the wildlife surgeon. Reducing the invasiveness of surgical procedures through different MIS techniques should not, however, be accomplished at the cost of increased risks to the patient.46
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree